Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo47
In Brazil, postpartum hemorrhage (PPH) is a major cause of maternal morbidity and mortality. Data on the profile of women and risk factors associated with PPH are sparse. This study aimed to describe the profile and management of patients with PPH, and the association of risk factors for PPH with severe maternal outcomes (SMO).
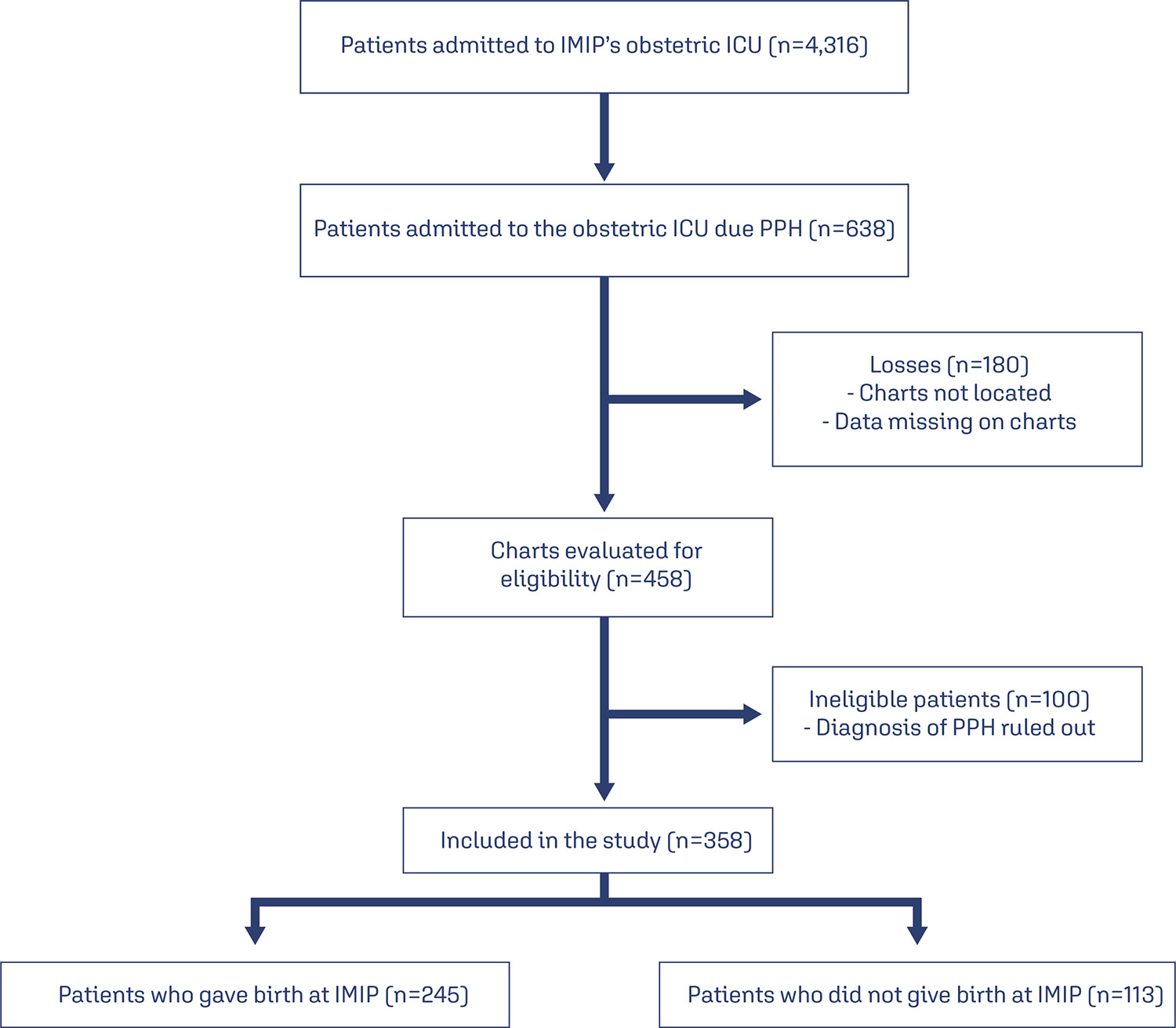
A cross-sectional study was conducted in Instituto de Medicina Integral Prof. Fernando Figueira (IMIP) obstetric intensive care unit (ICU) between January 2012 and March 2020, including patients who gave birth at the hospital and that were admitted with PPH to the ICU.
The study included 358 patients, of whom 245 (68.4%) delivered in the IMIP maternity, and 113 (31.6%) in other maternity. The mean age of the patients was 26.7 years, with up to eight years of education (46.1%) and a mean of six prenatal care. Uterine atony (72.9%) was the most common cause, 1.6% estimated blood loss, 2% calculated shock index (SI), 63.9% of patients received hemotransfusion, and 27% underwent hysterectomy. 136 cases of SMO were identified, 35.5% were classified as maternal near miss and 3.0% maternal deaths. Multiparity was associated with SMO as an antepartum risk factor (RR=1.83, 95% CI1.42-2.36). Regarding intrapartum risk factors, abruptio placentae abruption was associated with SMO (RR=2.2 95% CI1.75-2.81). Among those who had hypertension (49.6%) there was a lower risk of developing SMO.
The principal factors associated with poor maternal outcome were being multiparous and placental abruption.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):498-504
DOI 10.1590/SO100-720320150005286
To evaluate the risk factors for morbidity and mortality in an obstetric intensive care unit at a university hospital.
Observational cross-sectional study with 492 pregnant/puerperal women. Patients were admitted to the obstetric intensive care unit over a period of one year, being informed about the proposals of the study and a questionnaire was applied. The analysis was performed using Microsoft Excel 2013 and GraphPad Prism 6. To evaluate risk factors, χ2 tests were used.
The main risk factors to near miss were: non-white race (OR=2.5; PR=2.3); marital status (married women) (OR=7.9; PR=7.1), schooling (primary) (OR=3.1; PR=2.8), being from the countryside (OR=4.6; PR=4.0), low income (OR=70; PR=5.5), gestational hypertensive disorders (OR=16.3; PR=13.2), receiving prenatal care (OR=5.0; PR=4.254) and C-section before labor (OR=39.2; PR=31.2).
The prevalence of near miss was associated with socioeconomic/clinical factors and care issues, revealing the importance of interventions to improve these indicators. Additionally, we suggest a better curriculum insertion of this subject in the discipline of the medical course due to the importance of avoiding the near miss using adequate medical education. The importance of correct prenatal care is emphasized in order to identify potential risks, to provide nutritional support to pregnant women, to treat potential diseases and to establish a maternal immunization program, as well as providing better care regarding the clinical features of the patients, in order to reduce obstetrical and neonatal risk.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):29-34
DOI 10.1590/S0100-72032014000100007
To evaluate the maternal risk factors that require newborn assistance in neonatal Intensive Care Units (ICU).
A prospective observational case-control study was conducted on 222 pregnant women (1:1 case-control ratio) attended at a public maternity. The following variables were analyzed in the puerperae: age at menarche, age at first sexual intercourse, history of chronic diseases, habits, prenatal care, obstetric history, clinical complications during pregnancy and childbirth, and sociodemographic variables. The variables of the newborns were: Apgar scores, gestational age, birth weight, presence or absence of malformation, need for resuscitation, and complications during the first 24 hours. Proportions were compared using the Fisher exact test or the Person γ2 test. Multivariable models were developed by logistic regression analysis using adjusted Odds Ratio with a 95% confidence interval (CI).
Regarding reproductive history, ≥3 pregnancies and 2 or 3 previous cesareans were sytatistically significant (p=0.0 and 0.0, respectively). Among the complications that required assistance in the neonatal ICU, prematurity was responsible for 61 cases (55.5%), followed by risk of intrapartum infection in 46 cases (41.8%). Regarding the maternal history, the presence of hypertensive disease showed statistical significance (p=0.0). Premature rupture of membranes was strongly associated with the need for the neonatal ICU (Odds Ratio - OR=6.1, 95%CI 2.6-14.4).
Premature rupture of membranes and hypertensive disease should receive special attention in prenatal care due to their strong association with newborns requiring assistance in the neonatal ICU.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(2):80-86
DOI 10.1590/S0100-72032008000200006
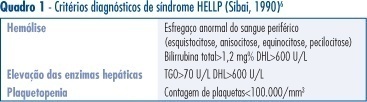
PURPOSE: to describe the clinical and laboratorial profile of HELLP syndrome patients admitted at an Obstetric Intensive Care Unit (ICU) and included in a randomized clinical trial to evaluate the efficacy of dexamethasone in this clinical setting. METHODS: the present study is a secondary analysis of a randomized clinical trial design to evaluate the efficacy of dexamethasone in patients with HELLP syndrome. This sample of patients was composed of patients in the puerperium, with the diagnosis of HELLP syndrome (diagnosis made before or after delivery) who were not chronic corticosteroid users and not carriers of any chronic disease which could modify HELLP syndrome's laboratorial parameters. Patients who were too critical or whose condition did not allow them to consent to participate were not included. Data were extracted from the records used in the randomized clinical trial. Age, parity, gestational age at admission and delivery, time of diagnosis (before or after delivery), HELLP syndrome classification (partial or complete), arterial blood pressure, and diuresis at admission were considered for analysis. Among laboratorial findings, hemoglobin, platelet count, liver enzymes, LDH, and serum bilirubin were analyzed. Complications presented by the patients were also analyzed as well as need of blood transfusions and duration of hospitalization. Analysis was made by the Epi-Info 3.3.2 program. RESULTS: one hundred and five patients were analyzed. Age varied from 14 to 49 years (means of 26.7). Regarding parity, 56 patients (53.8%) were primiparas. Analyzing the timing of the diagnosis, 47 patients (45.2%) had the diagnosis before delivery. The mean gestational age in these patients was 32.4 weeks. Hemorrhagic manifestations were observed in 36 patients (34.3%), oliguria was present in 49 patients (46.7%) and criteria for acute renal failure were seen in 21 (20%) of the cases. Hemotransfusions were necessary in 35 (33.3%) patients. Seven patients (6.7%) had pulmonary edema and four patients died, corresponding to 3.8% of the cases. The mean time from diagnosis of HELLP syndrome to discharge or death was 10.3 days, varying from 1 to 33 days. CONCLUSIONS: HELLP syndrome is an ominous diagnosis, which implicates in elevated maternal morbimortality. Among complications, oliguria and hemorrhagic manifestations were the most common findings and hemotransfusions were frequently required. Lethality reached 3.8%.