Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):188-195
04-01-2018
To analyze the association between the indirect methods of evaluating insulin resistance (IR) and blood pressure, anthropometric and biochemical parameters in a population of polycystic ovary syndrome (PCOS) patients.
Cross-sectional study performed at the Hospital Universitário de Brasília (HUB, in the Portuguese acronym) involving PCOS patients diagnosed from January 2011 to January 2013. Four indirect methods, namely, fasting blood insulin level, fasting glucose/insulin ratio (G/I), homeostatic model-assessment-insulin resistance (HOMA-IR), and the quantitative insulin sensitivity check index (QUICKI), were used to obtain the IR diagnosis. The data were analyzed using the test of proportions, the Chisquare test, and Fisher exact test, when indicated.
Out of the 83 patients assessed, aged 28.79 ± 5.85, IR was found in 51.81- 66.2% of them using the G/I ratio and the QUICKI, respectively. The test of proportions did not show a significant difference between the methods analyzed. The proportion of IR diagnoses was statistically higher in obese women than in women with normal body mass index (BMI). We observed a statistically significant association between all the methods for diagnosing IR and BMI, waist circumference (WC) and lipid accumulation product (LAP). With regards to arterial hypertension (AH), we observed a significant association according to three methods, with the exception of the ratio G/I.
Insulin resistance prevalence varied according to the diagnostic method employed,with no statistical difference between them. The proportion of IR diagnoses was statistically higher in obese women than in women with normal BMI.We observed a significant association between IR andWC, BMI, LAP, as well as dyslipidemia and AH in a high proportion of patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):224-228
05-01-2017
This study analyzed the effectiveness of the thyroid-stimulating hormone (TSH) as a predictor of insulin resistance (IR) and its association with the clinical and metabolic parameters of women with polycystic ovary syndrome (PCOS) without overt hypothyroidism.
A cross-sectional study was performed. Women with PCOS and without overt hypothyroidism (n = 168) were included.
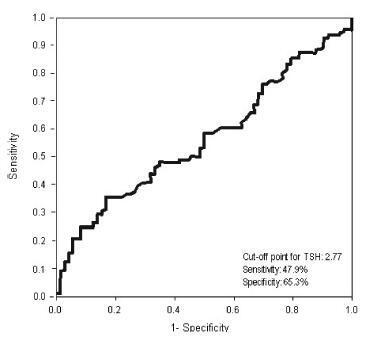
Receiver operating characteristic (ROC) curve was used to determine the cut-off point for TSH that would maximize sensitivity and specificity for a diagnosis of IR using homeostatic model assessment of insulin resistance (HOMA-IR)≥ 2.71. Clinical and metabolic parameters were compared as a function of the TSH cut-off limit and the presence of IR.
Thyroid-stimulating hormone ≥ 2.77 mIU/L was associated with a diagnosis of IR, with sensitivity of 47.9% and specificity of 65.3%. There were no differences in clinical, hormonal or metabolic parameters between TSH < 2.77 and TSH of 2.77 - 10 mIU/L.
In women with PCOS without overt hypothyroidism, TSH ≥2.77 mIU/L is associated with IR; however, with poor sensibility, showing TSH to be a poor predictor of IR in this population. No clinical or metabolic alterations were found that would justify a change in clinical management. Thus, the IR should be investigated in all women with PCOS irrespective of TSH level.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):71-76
02-01-2016
Polycystic ovary syndrome (PCOS) is the most common endocrine metabolic disorder in women between menarche and menopause. Clinical hyperandrogenism is the most important diagnostic criterion of the syndrome, which manifests as hirsutism in 70% of cases. Hirsute carriers of PCOS have high cardiovascular risk. Lipid accumulation product (LAP) is an index for the evaluation of lipid accumulation in adults and the prediction of cardiovascular risk. The aim of this study was to evaluate the association between LAP and hirsutism in women with PCOS.
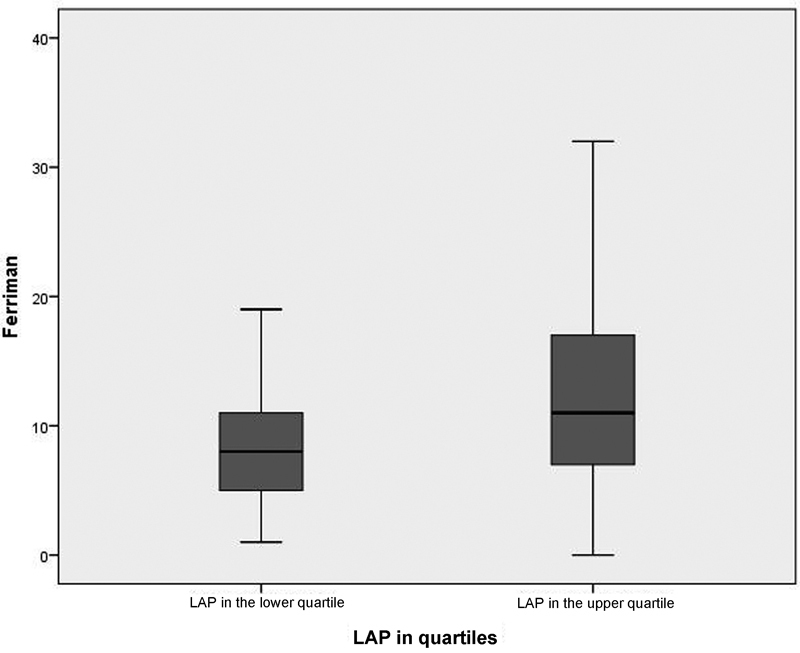
This was a cross-sectional observational study of a secondary database, which included 263 patients who had visited the Hyperandrogenism Outpatient Clinic from November 2009 to July 2014. The exclusion criteria were patients without Ferriman-Gallwey index (FGI) and/or LAP data. We used the Rotterdam criteria for the diagnosis of PCOS. All patients underwent medical assessment followed by measurement and recording of anthropometric data and the laboratory tests for measurement of the following: thyroid-stimulating hormone, follicle-stimulating hormone, prolactin, total testosterone, sex hormone binding globulin, 17-α-hydroxyprogesterone (follicular phase), glycohemoglobin A1c, and basal insulin. In addition, the subjects underwent lipid profiling and oral glucose tolerance tests. Other laboratory measurements were determined according to clinical criteria. LAP and the homeostatic model assessment index (HOMA-IR) were calculated using the data obtained. We divided patients into two groups: the PCOS group with normal LAP (< 34.5) and the PCOS group with altered LAP (> 34.5) to compare the occurrence of hirsutism. For statistical analysis, we used SPSS Statistics for Windows(r) and Microsoft Excel programs, with descriptive (frequencies, percentages, means, and standard deviations) and comparative analyses (Student's t-test and Chi-square test). We considered relations significant when the p-value was≤0.05.
LAP was high in most patients (n = 177; 67.3%) and the FGI indicated that 58.5% of the patients (n = 154) had hirsutism. The analysis by LAP quartiles showed a positive correlation (p = 0.04) among patients with a high FGI and an upper quartile LAP (> 79.5) when compared with those with LAP < 29.0 (lower quartile).
This study demonstrated an association between high LAP and hirsutism. The FGI could represent a simple and low-cost tool to infer an increased cardiovascular risk in women with PCOS.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(2):74-79
03-15-2012
DOI 10.1590/S0100-72032012000200006
PURPOSE: To analyze the prevalence of insulin resistance, according to different biochemical and anthropometric measurements in women with polycystic ovary syndrome. METHODS: A total of 189 patients with polycystic ovary syndrome were retrospectively analyzed. Insulin resistance diagnosis was performed using fasting insulin, HOMA-IR, QUICKI, insulin sensibility index and glucose/fasting insulin ratio. Body mass index and lipid accumulation product were used. Data were analyzed statistically by descriptive statistics, ANOVA, Tukey post-test, and Pearson's correlation. RESULTS: The polycystic ovary syndrome patients had a mean age of 24.9±5.2 and a mean body mass index of 31.8±7.6. The percentage of obese patients was 57.14%. Among the methods of insulin resistance investigation, the insulin sensibility index was the technique that most detected (56.4%) the presence of insulin resistance in women with polycystic ovary syndrome. The insulin resistance was detected in 87% of obese patients. The fasting glucose/fasting insulin ratio and insulin sensibility index were strongly correlated with lipid accumulation product. CONCLUSION: The prevalence of insulin resistance varied according to the method used, and it was greater the higher the body mass index. Lipid accumulation product was also related to insulin resistance.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(6):310-316
08-19-2011
DOI 10.1590/S0100-72032011000600008
PURPOSE: To compare the metabolic characteristics of obese and non-obese young women with polycystic ovary syndrome (POS) from the Brazilian Southeast. METHODS: This was a cross-sectional study conducted on 218 women of reproductive age with a diagnosis of POS - 90 non-obese women (BMI between 18.5 and 29.9 kg/m²), and 128 obese patients (BMI >30 kg/m²) selected at the time of diagnosis. The frequency of insulin resistance (IR), glucose intolerance (GI), metabolic syndrome (MetS) and type 2 diabetes mellitus (DM2) and mean values of total cholesterol (TC), triglycerides (TG), high-density (HDL) and low-density lipoproteins (LDL), were compared between obese and non-obese patients with POS. The two groups were also compared in terms of clinical and hormonal characteristics (follicle stimulating hormone, prolactin, thyroid stimulating hormone, total testosterone, dihydroepiandrostenedione sulfate, and 17-hydroxyprogesterone). Statistical analysis was performed using the SAS 9.0 software. Quantitative variables were compared by the Student´s t-test (data with normal distribution) or by the Mann-Whitney test (non-parametric distribution). Qualitative variables were compared by the Fisher test. The level of significance was set at 5% (p<0.05) in all analyses. RESULTS: The frequency of IR, GI and MetS was significantly higher in obese than non-obese patients with POS (66.7, 29.9, and 63% versus 24.7, 12.2, and 16.4%, respectively). Obese patients had higher TC and TG levels (189.8±35.8 mg/dL and 145.4±71.1 mg/dL, respectively) than non-obese patients (172.1±38.4 mg/dL and 99.3±54 mg/dL, respectively). Both groups had mean HDL levels below 50 mg/dL. CONCLUSIONS: Young obese women with POS have a higher frequency of IR, GI and MS than non-obese. However, the occurrence of metabolic disorders is elevated also in the non-obese patients, suggesting that the presence of the syndrome may favor the development of metabolic comorbidities with potential medium- and long-term repercussions.