-
Original Article10-01-2016
Factors Associated with Infant Mortality in a Northeastern Brazilian Capital
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):482-491
Abstract
Original ArticleFactors Associated with Infant Mortality in a Northeastern Brazilian Capital
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):482-491
Views157See moreAbstract
Purpose
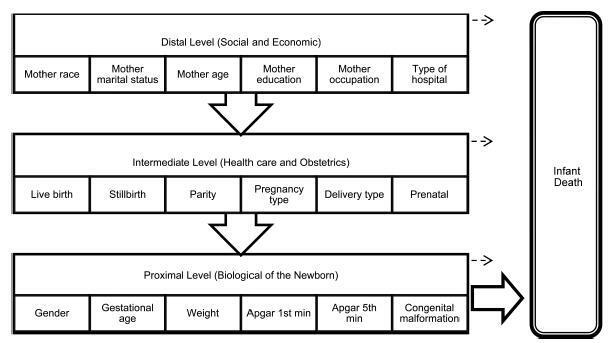
Identify factors associated with infant mortality by a hierarchical model based on socioeconomic, health care, obstetric and biological determinants in a northeastern Brazilian capital.
Methods
Observational, retrospective cohort study based on secondary data of births and deaths of infants of mothers living in the city of Teresina.
Results
Based on the distal level of determination of infant mortality, the characteristics that remained statistically significant were maternal age, maternal education and maternal occupation (p< 0.001). In the intermediate level, all variables were statistically significant, particularly the type of pregnancy and delivery (p< 0.001). The gender of the baby was the proximal level feature that had no significant association with the outcome, while the other variables of this level had association (p< 0.001).
Conclusions
This study evidenced that, in addition to biological factors, socioeconomic status and maternal and child health care are important to determine infant mortality.
-
Original Article12-01-2014
Time trend of the rates of cesarean and vaginal delivery according to the source of financing
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):548-554
Abstract
Original ArticleTime trend of the rates of cesarean and vaginal delivery according to the source of financing
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):548-554
DOI 10.1590/So100-720320140005038
Views125PURPOSE:
To analyze the time trend of the rates of cesarean and vaginal delivery according to the source of financing.
METHODS:
This was an ecological study of the time series analysis of cesarean and vaginal delivery rates according to the financing source, carried out in Maringá, Paraná State, Brazil, from 2002 to 2012. Information available at the System of Information on Live Births and at the System of Hospital Information of the Brazilian Unified Health System (SUS) was used for data collection. Moving averages were calculated for all mode of delivery rates in order to smooth random fluctuations in the series, dispersion diagrams were designed between the coefficients and years of the study, and polynomial regression models were estimated from the functional relation observed, with the level of significance set at p<0.05.
RESULTS:
Throughout the 11 years of the study there were 48,210 births, 77.1% by cesarean delivery and only 22.9% by vaginal delivery. A total of 22,366 procedures were financed by SUS, 54.6% of them being cesareans. Trend analysis was significant for all the regression models, demonstrating an ascending trend for cesarean delivery and a descending trend for vaginal delivery for both types of financing. The non-SUS cesarean rates always exceeded 90.0% and were more frequent than the SUS cesarean rates, even with a 36.0% increase of the latter during the study period.
CONCLUSION:
Based on trend analysis, cesarean deliveries will continue to increase in both health financing sources unless new actions and strategies of reduction are implemented, involving the sociocultural, demographic and obstetric characteristics of women, the training and activity of professionals in the area of obstetrics and an adequate structure of health services for providing vaginal delivery.
Key-words Birth certificatesCesarean sectionHospitals, privateHospitals, publicInformation systemsNatural childbirthSee more -
Original Article02-01-2014
Association between risk pregnancy and route of delivery with maternal and neonatal outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(2):65-71
Abstract
Original ArticleAssociation between risk pregnancy and route of delivery with maternal and neonatal outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(2):65-71
DOI 10.1590/S0100-72032014000200004
Views88See morePURPOSE:
To analyze the relationships among gestational risk, type of delivery and
immediate maternal and neonatal repercussions.METHODS:
A retrospective cohort study based on secondary data was conducted in a
university maternity hospital. A total of 1606 births were analyzed over a 9-month
period. Epidemiological, clinical, obstetric and neonatal characteristics were
compared according to the route of delivery and the gestational risk characterized
on the basis of the eligibility criteria for high clinical risk. The occurrence of
maternal and neonatal complications during hospitalization was analyzed according
to gestational risk and cesarean section delivery using univariate and
multivariate logistic analysis.RESULTS:
The overall rate of cesarean sections was 38.3%. High gestational risk was
present in 50.2% of births, mainly represented by hypertensive disorders and fetal
malformations. The total incidence of cesarean section, planned cesarean section
or emergency cesarean section was more frequent in pregnant women at gestational
high risk (p<0.001). Cesarean section alone did not influence maternal outcome, but was associated with poor neonatal outcome (OR 3.4; 95%CI 2.7-4.4). Gestational high risk was associated with poor maternal and neonatal outcome (OR 3.8; 95%CI 1.3-8.7 and OR 17.5; 95%CI 11.6-26.3, respectively). In multivariate analysis, the ratios were maintained, although the effect of gestational risk has determined a reduction in the OR of the type of delivery alone from 3.4 (95%CI 2.7-4.4) to 1.99 (95%CI 1.5-2.6) for adverse neonatal outcome.CONCLUSION:
Gestational risk was the main factor associated with poor maternal and neonatal
outcome. Cesarean delivery was not directly associated with poor maternal outcome
but increased the chances of unfavorable neonatal outcomes.


