Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(10):603-605
DOI 10.1590/S0100-72031999001000007
The cryopreservation of embryos in late developing stages seems to present satisfactory results. With the purpose of better testing the embryos' survival, they were cryopreserved in the morula or blastocyst stage, thawed and left in culture for 24 hours so that their natural evolution could be observed. Amongst the frozen 2 blastocysts and 5 morulas, 4 morulas survived the thawing process, being transferred as blastocysts 24 hours later. The transfer was performed in a young patient, second marriage of a ten-year vasectomized man and resulted in twin pregnancy. Thawing morula embryos and the in vitro observation of their development resumption until the blastocyst stage give us an additional parameter in the quality evaluation of the embryo and probably an improvement in pregnancy rates.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):216-221
DOI 10.1590/S0100-72032005000400009
PURPOSE: to identify the relationship between serum levels of leptin and the levels of estradiol and follicle-stimulating hormone (FSH) in women with pituitary suppression and to evaluate its possible interference on the reproductive axis. METHODS: a total of 64 patients submitted to controlled ovarian hyperstimulation with recombinant FSH for assisted reproduction, due to a male or tubal factor, and 20 patients using estradiol valerate, for endometrial preparation in order to be submitted to oocyte donation treatment were studied. All patients used GnRH analogues before starting treatment in order to avoid premature LH surge. Data were analyzed statistically by the chi2 test, Student's t-test and the Pearson correlation test, when appropriate, with the level of significance set at p<0,05. RESULTS: it was observed that leptin levels correlated with body mass index (BMI) even though they had not influenced growth rate of these hormones. A positive correlation was observed between estradiol and leptin levels in both groups, as leptin levels increased from 10.42 to 15.68 ng/mL in the FSH group and from 11.09 to 14.5 ng/mL in the estradiol group, following estradiol increase. The growth rate of leptin was higher in women with higher estradiol levels, i.e., who had induced cycles with recombinant FSH, than in those who received estradiol valerate (159.60±58.01 and 136.73±34.17, respectively). CONCLOSION: we may state that leptin correlated with BMI and that both FSH and estradiol do interfere in the regulation of leptin production in women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(10):773-780
DOI 10.1590/S0100-72032004001000004
PURPOSE: to compare the information obtained with pelvic and transvaginal ultrasonography (USG), hystero-salpingography (HSG), diagnostic hysteroscopy (HSC), pelvic nuclear magnetic resonance imaging (PNMR), three-dimensional hysterosonography (3D HSSNG), to optimize and simplify the investigation about cervical and corporeal uterine factors in conjugal infertility. METHODS: in the period between January and July 2003, fifty women reporting infertility for at least two years were submitted to USG, HSG, HSC, PNMR, and 3D HSSNG as tracking examinations for uterine factor diagnosis. The endocervical canal, as well as the endometrium, myometrium, and the presence of uterine malformations were investigated. The results of each examination were analyzed and compared. RESULTS: of the 50 women studied, 12 (24%) presented alteration in at least one of the examinations. When 3D HSSNG was compared to USG, 3D HSSNG provided additional information in 7 cases (58.3%); when compared to HSG, it provided additional information in 7 cases (58.3%); when compared to HSC, it provided additional information in 4 cases (32.1%), and when compared to PNMR, it provided additional information in 6 cases (50%). There were only two cases in which HSG detected alterations of the endocervical canal that were not visualized using 3D HSSNG. In the other cases 3D HSSNG imparted the same diagnosis; furthermore, it provided additional information in comparison to the other examinations. Statistical analysis using the kappa test demonstrated that the diagnoses obtained by 3D HSSNG were in agreement with those obtained with USG, HSG and PNMR (p<0,05). When the HSG and 3D HSSNG results were combined, all conditions associated with infertility could be precisely diagnosed, using only these examinations. CONCLUSION: the association of the HSG with 3D HSSNG may be sufficient for the diagnosis of cervical and corporeal uterine factors in infertility, reducing the number of examinations for each patient, the total cost, as well as the anxiety and the delay in treatment.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(10):711-715
DOI 10.1590/S0100-72032003001000003
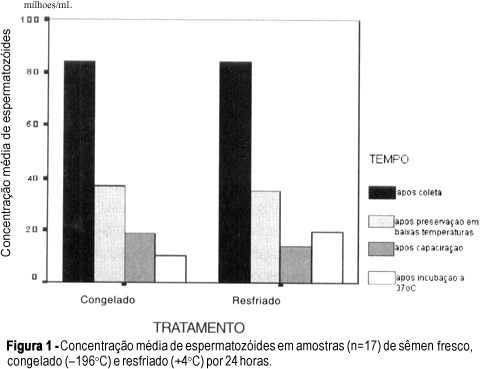
PURPOSE: to compare the characteristics of human semen preserved at +4ºC and at -196ºC for 24 h and to determine which technique is indicated for use in specific procedures. METHODS: semen samples of 24 voluntaries were analyzed after collection and divided into two aliquots, one of them cooled (+4ºC) and the other frozen (-196ºC). Samples were kept at low temperatures for 24 h and then at room temperature for 30 minutes (T1), capacitated (T2) and kept at +37ºC for 90 minutes (T3), being analyzed regarding count and progressive motility at T1, T2 and T3. The General Linear Model was used to analyze results obtained with different techniques, while Wilcoxon's test was used to compare results obtained in two different moments using the same technique (a = 5% e p<0,05). RESULTS: data were missed in one fresh semen sample, in one sample after preservation, in five samples after capacitation and in two samples after incubation. The average number of total motile sperm/mL (NTMS) in fresh semen was 39.7 million (1.3-104.0). After preservation, the average NTMS in cooled semen was 9.6 million (0-37.4) and in frozen semen 8.7 million (0-41.2). After capacitation, the average NTMS was 5.4 million either in cooled (0-21.7), or in frozen semen (0-28). After incubation, the average NTMS in cooled semen was 9.8 million (0-40.5) and in frozen 4.4 million (0-25.6). Concerning count, progressive motility and NTMS, there was no significant difference (p>0,05) between techniques in the three moments of observation. In cooled samples, there was no difference between variables after capacitation and after incubation, but, in frozen semen, count was significantly greater after capacitation. CONCLUSIONS: although there has been no significant difference between semen count and progressive motility in both techniques, the use of cooled semen is recommended for specific procedures within a short time period due to its simplicity and low cost. When frozen semen is necessary, we recommend its use soon after capacitation in order to avoid loss in quality.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):519-523
DOI 10.1590/S0100-72032003000700009
PURPOSE: to analyze the accuracy of sonohysterography for the evaluation of the uterine cavity in patients with an implantation failure, at the first attempt of an in vitro fertilization cycle. METHODS: in a prospective double blind study, the authors analyzed patients previously submitted to at least one embryo transfer, who presented implantation failures. The patients were submitted to a sonohysterographic examination followed by a diagnostic hysteroscopic examination, carried out by different professionals each of whom was not aware of the results of the other. The results were recorded and only interpreted after the end of the trial. Sonohysterography was performed by the introduction of a urethral catheter 8 into the uterine cervix followed by infusion of physiological saline. The anechoic interface shown by the physiological saline can reveal abnormalities, like uterine polyps or submucosal myomas. Hysteroscopy was performed with a Karl Storz equipment, 4 mm 30º rigid telescope, and infusion of physiological saline for uterine cavity distention. RESULTS: twenty-eight of the 33 originally selected patients for this study were analyzed. Sonohysterography detected abnormalities in 8 patients, five with endometrial polyps (62.5%), two with endocervical polyps (25.0%), and one with submucosal myoma (12.5%). Hysteroscopy (gold standard) detected abnormalities in 7 patients, two with endometrial polyps (28.6%), two with cervical polyps (28.6%) and one with submucosal myoma (14.2%). Sonohysterography, when compared with diagnostic hysteroscopy, presented 71.4% sensibility, 85.7% specificity, 62.5% positive predictive value, and 90% negative predictive value of. CONCLUSION: due to its low positive predictive value, the authors suggest confirmation of the sonohysterography result by diagnostic hysteroscopy. Because sonohysterography presents a good level of specificity and a favorable low negative predictive value, the authors suggest that after a normal sonohysterography diagnostic hysteroscopy to evaluate the uterine cavity before in vitro fertlization is not necessary. This study leads to the conclusion that sonohysterography is a good screening method for the detection of polypoid lesions of the uterine cavity, which could be responsible for implantation failures in in vitro fertilization cycles.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):513-516
DOI 10.1590/S0100-72032003000700008
PURPOSE: to evaluate the usefulness of the in vitro maturation technique of human oocyte and subsequent fertilization. METHODS: this is a prospective nonrandomized, descriptive study, carried out during the period of November 1999 to March 2001, with 20 cycles of in vitro fertilization of 15 patients with tubal infertility. All signed the written informed consent before the beginning of the study. The selected patients were at least 18 and at most 32 years of age, with only tubal infertility, and body mass index less than 25 kg/m². The patients received 300 UI of recombinant follicle stimulating hormone (FSH) by intramuscular injection at the second day of the cycle and additional doses of 150 IU at the fourth and sixth days of cycle. The oocyte retrieval was performed at the seventh day of the cycle. Those oocytes classified as immature were cultured in tissue culture medium 199 (TCM-199) with antibiotics, pyruvate, FSH, human chorionic gonadotropin (hCG) and serum (serum substitute supplement - Irvine Scientific®). After 48 h of culture, the oocytes that achieved metaphase II stage were inseminated, and the fertilized ones were transferred. RESULTS: one hundred and forty-four follicles were aspirated. There were 67 (46.5%) immature retrieved oocytes and 43 (64.2%) reached the metaphase II stage and were inseminated. Thirty fertilized oocytes and 25 embryos were transferred to 10 patients. There was one pregnancy with a baby born. CONCLUSION: we conclude that to mature human oocytes in vitro before in vitro fertilization is a procedure able to achieve pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(4):243-248
DOI 10.1590/S0100-72032003000400004
PURPOSE: to analyze the influence of seminal parameters on intrauterine insemination (IUI) outcomes in patients with male factor and to emphasize the predictive value of each parameter for the successful result. METHODS: two hundred and thirty-nine IUI cycles (155 couples) were analyzed for 15 months. Female patients were submitted to ovary hyperstimulation according to the "I Consenso Brasileiro de Indução de Ovulação". Seminal analysis based on the World Health Organization (WHO) for sperm concentration and motility was used and sperm morphology was evaluated according to Kruger's criterion. Samples to be used in IUI were prepared by colloidal discontinued gradient (ISolate®). After IUI two patient groups were formed: group G - positive for pregnancy and group NG - negative for pregnancy. RESULTS: there was no statistical difference in total sperm concentration per mL, total motility and progressive motility before and after the ISolate® procedure. When sperm morphology was compared between the two groups, a statistical difference was observed (group G=10.6% normal morphology; group NG=6.4% normal morphology; p<0.05). Better pregnancy results were obtained when the number of inseminated spermatozoa was more than 15 x 10(6)/mL. CONCLUSIONS: sperm morphology and the number of inseminated sperm seem to be positive parameters for pregnancy and should be emphasized during male infertility propaedeutics.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(10):641-646
DOI 10.1590/S0100-72032001001000005
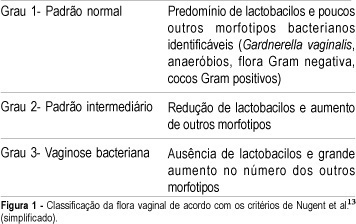
Purpose: to evaluate the prevalence of bacterial vaginosis (BV) in menopausal and in infertile outpatients and to analyze the current clinical diagnostic methods. Methods: we evaluated retrospectively 104 menopausal women and 86 with infertility. Characteristic vaginal discharge on gynecological examination, pH >4.5, positive KOH whiff test, and bacterial vaginosis by Gram test were considered positive. BV was established when at least 3 out of 4 criteria were found. Results: among the menopausal women, 29 patients (28.1%) were clinically positive for BV, 10 (9.6%) had positive whiff test, 68 (65.4%) vaginal pH >4.5, and 34 (32.7%) positive Gram test. For the infertile patients the figures were 20 (23.2%), 13 (15.1%), 61 (70.9%) and 26 (30.2%), respectively. According to our established criteria, BV was diagnosed in 14 menopausal (13.5%) and 15 infertile (17.4%) women. Conclusion: bacterial vaginosis prevalence was similar in both groups of patients. In addition, all diagnostic criteria should be followed in order to avoid underdiagnosing this pathology or treating an otherwise normal vaginal flora.