-
Original Article
Effect of COVID-19 on Brazilian cesarean and prematurity rates: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo6
03-18-2025
Summary
Original ArticleEffect of COVID-19 on Brazilian cesarean and prematurity rates: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo6
03-18-2025Views65See moreAbstract
Objective:
To investigate the relationship between prematurity and cesarean section rate in Brazil during the beginning of COVID-19 pandemic.
Methods:
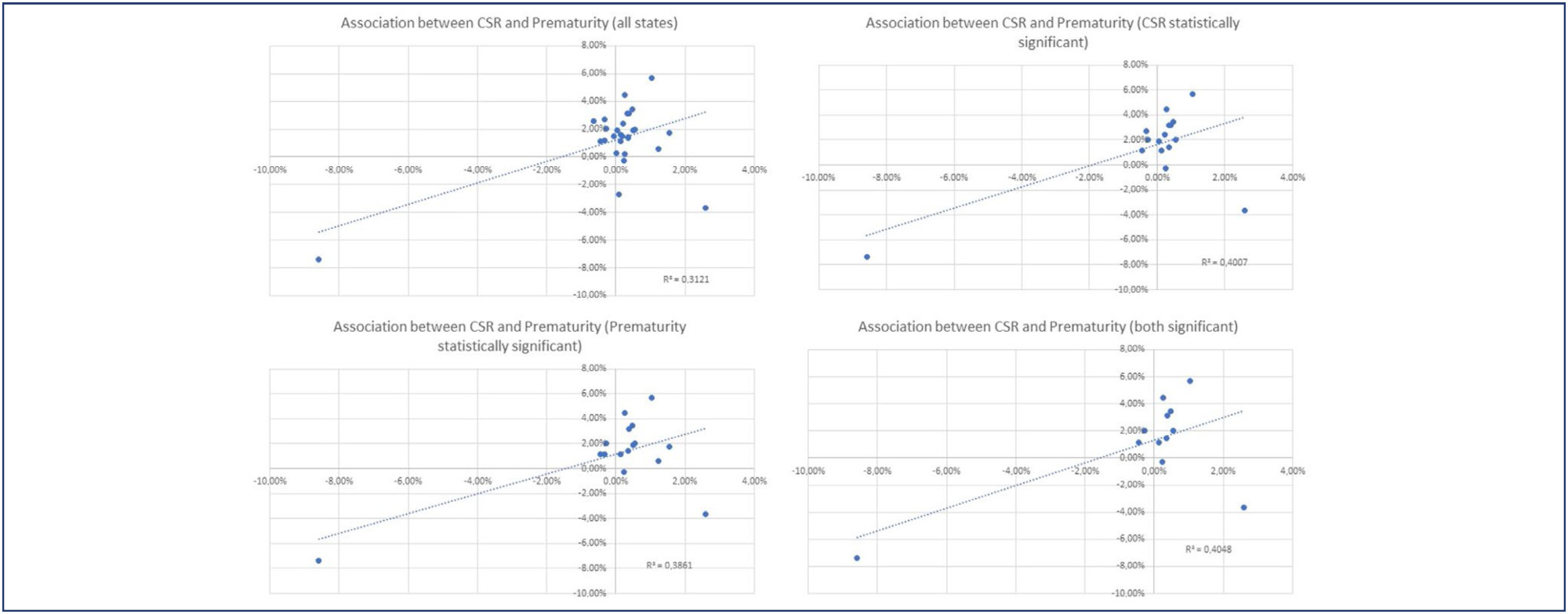
Utilizing the Robson Classification, this study analyzed data from the Brazilian Ministry of Health's Live Births Panel, comparing CSR) and group 10 (preterm deliveries) between 2019 (pre-pandemic) and 2021 (pandemic) in each of Brazilian states and the overall country. The prematurity and CSR were compared using prevalence ratio and confidence interval, and p-value was obtained. The variation of prematurity and CSR were compared through the coefficient of determination (R2).
Results:
A total of 5,522,910 deliveries were evaluated during the period. The CSR increased from 56.34% to 57.05% (p<0.01), and the frequency of preterm deliveries rose from 8.99% to 9.13% (p<0.01). The CSR increased in 23 States and decreased in 4 States, while the prematurity rate increased in 16 States and decreased in 10 States. A positive relationship between the increase of CSR and prematurity was observed during COVID-19, with an R2 value of 0.3121, suggesting a moderate association between these two variables.
Conclusion:
Between 2019 (pre-COVID-19 pandemic) and 2021 (the first full year of the COVID-19 pandemic), there was an increase in prematurity and CSR in Brazil. These increases were observed in most Brazilian states and may be correlated. However, it is impossible to establish a cause-effect relationship given the design of this study.
-
Review Article
Neonatal and maternal outcomes of mRNA versus Non-mRNA COVID-19 vaccines in pregnant patients: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo69
09-18-2024
Summary
Review ArticleNeonatal and maternal outcomes of mRNA versus Non-mRNA COVID-19 vaccines in pregnant patients: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo69
09-18-2024Views196Abstract
Objective
To compare the effectiveness and safety of non-mRNA versus mRNA COVID-19 vaccines on pregnant women and their newborns in a systematic review with meta-analysis.
Data sources
We searched PubMed, Embase, and Cochrane Central in May 2023.
Study selection
The search strategy yielded 4451 results, 16 studies were fully reviewed. We selected case-control studies analysing non-mRNA versus mRNA vaccines. Data collection and analysis: we assessed the risk of bias using the Cochrane Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool. Standardised mean differences were pooled using random-effect models.
Data synthesis
We identified 8 prospective and retrospective studies with a total of 32,153 patients. Non-mRNA vaccines were associated with a higher incidence of fever (OR 2.67; 95% CI 2.08-3.43; p<0.001), and a lower incidence of fetal or neonatal death (OR 0.16; 95% CI 0.08-0.33; p<0.001). In subgroup analyses, the Jansen vaccine (Ad26.COV2.S) was found to have a higher rate of premature labor/delivery (OR 4.48; 95% CI 1.45-13.83; p=0.009) and missed/spontaneous abortion (OR 1.90; 95% CI 1.09-3.30; p=0.02), as compared with the Pfizer (BNT162b2) vaccine.
Conclusion
non-mRNA vaccines are associated with a lower incidence of fetal or neonatal death among pregnant women who receive a Covid19 vaccine, although at an increased rate of pyrexia compared with mRNA vaccines. Other studies are required for better assessment.
PROSPERO
CRD42023421814
Key-words coronavirus infectionsCOVID-19COVID-19 vaccinesInfant, newbornmRNA vaccinesPregnancy complicationsPregnant womenSARS-CoV-2See more -
Original Article
Association between dietary patterns and infant birth weight in brazilian pregnancy women with gestational diabetes: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo68
09-06-2024
Summary
Original ArticleAssociation between dietary patterns and infant birth weight in brazilian pregnancy women with gestational diabetes: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo68
09-06-2024Views143See moreAbstract
Objective
To evaluate the association between the dietary patterns (DPs) of pregnant women with GDM (gestational diabetes mellitus) and the birth weight (BW) of the infants.
Methods
Cross-sectional study with 187 adult pregnant women with GDM attended at a maternity in Rio de Janeiro from 2011 to 2014. Dietary intake was assessed in the third trimester using a semiquantitative food frequency questionnaire (FFQ). The outcomes were BW and weight adequacy for gestational age (GA). Reduced Rank Regression (RRR) was used to explain the following response variables: density of carbohydrates, fibres, and saturated fatty acids. Statistical analyzes included multinomial logistic regression models.
Results
The mean BW was 3261.9 (± 424.5) g. Three DPs were identified, with DP 3 (high consumption of refined carbohydrates, fast foods/snacks, whole milk, sugars/sweets, and soft drinks and low consumption of beans, vegetables, and low-fat milk and derivatives) being the main pattern, explaining 48.37% of the response variables. In the multinomial logistic regression analysis no statistically significant association was found between the tertiles of DPs and BW or the adequacy of weight for GA, even after adjustments of confounding covariates.
Conclusion
No significant associations were found between maternal DPs in the third trimester of pregnancy and infant BW or adequacy of weight for GA.
-
Original Article
Factors associated with exclusive breastfeeding in “Near Miss” neonates in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo59
07-26-2024
Summary
Original ArticleFactors associated with exclusive breastfeeding in “Near Miss” neonates in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo59
07-26-2024Views94See moreAbstract
Objective
To assess the association between sociodemographic and perinatal factors and hospital practices to encourage exclusive breastfeeding in near miss neonates in maternity hospitals.
Methods
This is a prospective cohort of live births from the survey “To be born in Brazil” conducted between 2011 and 2012. The weighted number of newborns who met the neonatal near miss criteria was 832. Exclusive breastfeeding at hospital discharge and 45 days after delivery were dependent variables of the study. The sociodemographic and perinatal factors of the puerperal women and hospital practices to encourage breastfeeding were independent variables. The data were analyzed with Poisson regression and set with p value<0.05. Is exclusive breastfeeding in neonatal near misses associated with factors related to sociodemographic conditions, maternal characteristics and the organization of health services?
Results
Data from 498 women and their children were analyzed. Mothers with incomplete primary education were more likely (36%) to have exclusive breastfeeding (RR: 1.36; 95% CI: 1.06-1.74) at discharge. Women who did not offer the breast to the newborn in the joint accommodation (65%) were less likely to be breastfeeding exclusively (RR: 0.65; 95% CI: 0.56-0.75) at discharge. Variables that increased the probability of exclusive breastfeeding after 45 days of delivery were primiparity (RR: 1.36; 95% CI: 1.08-1.69) and having the newborn in the delivery room (RR: 1.90; 95% CI: 1.12-3.24).
Conclusion
Exclusive breastfeeding in neonatal near misses was associated with maternal characteristics and important hospital practices, such as being breastfed in the joint accommodation and the newborn being in the mother’s lap in the delivery room.
-
Original Article
Mode of delivery according to Robson classification and perinatal outcomes in restricted and small for gestational age fetuses
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo30
07-26-2024
Summary
Original ArticleMode of delivery according to Robson classification and perinatal outcomes in restricted and small for gestational age fetuses
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo30
07-26-2024Views151Abstract
Objective
To evaluate the mode of delivery according to Robson classification (RC) and the perinatal outcomes in fetal growth restriction (FGR) and small for gestational age (SGA) fetuses.
Methods
Retrospective cohort study by analyzing medical records of singleton pregnancies from two consecutive years (2018 and 2019). FGR was defined according to Delphi Consensus. The Robson groups were divided into two intervals (1–5.1 and 5.2–10).
Results
Total of 852 cases were included: FGR (n = 85), SGA (n = 20) and control (n=747). FGR showed higher percentages of newborns < 1,500 grams (p<0.001) and higher overall cesarean section (CS) rates (p<0.001). FGR had the highest rates of neonatal resuscitation and neonatal intensive care unit admission (p<0.001). SGA and control presented higher percentage of patients classified in 1 - 5.1 RC groups, while FGR had higher percentage in 5.2 - 10 RC groups (p<0.001). FGR, SGA and control did not differ in the mode of delivery in the 1-5.1 RC groups as all groups showed a higher percentage of vaginal deliveries (p=0.476).
Conclusion
Fetuses with FGR had higher CS rates and worse perinatal outcomes than SGA and control fetuses. Most FGR fetuses were delivered by cesarean section and were allocated in 5.2 to 10 RC groups, while most SGA and control fetuses were allocated in 1 to 5.1 RC groups. Vaginal delivery occurred in nearly 60% of FGR allocated in 1-5.1 RC groups without a significant increase in perinatal morbidity. Therefore, the vaginal route should be considered in FGR fetuses.
Key-words Cesarean sectionFetal growth retardationFetusGestational ageInfant, newbornInfant, small for gestational agePregnancy outcomerobson classificationSee more -
Artigos Originais
Obesity during pregnancy: gestational complications and birth outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
11-01-2014
Summary
Artigos OriginaisObesity during pregnancy: gestational complications and birth outcomes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(11):509-513
11-01-2014DOI 10.1590/S0100-720320140005024
Views120See morePURPOSE:
To evaluate the influence of maternal obesity on pregnancy, childbirth, and neonatal outcomes.
METHODS:
A cross-sectional study with 298 postpartum women. Information was obtained through interviews and access to patients' medical records. The patients were divided into three groups according to their pre-gestational body mass index: normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2). Data are reported as adjusted odds ratios with 95% confidence interval (95%CI) following multinomial logistic regression analysis to account for confounding variables.
RESULTS:
Compared to pregnant women with normal body mass index, overweight women had greater chances of having cesarean delivery, odds ratio (OR) of 2.2 and 95%CI 1.3–3.9, and obese women even more (OR=4.2; 95%CI 2.1–8.1). The chances of gestational diabetes increased in the Overweight (OR=2.5; 95%CI 1.1–5.6) and Obese groups (OR=11.1; 95%CI 5.0–24.6). The occurrence of hypertensive syndrome was also higher in overweight (OR=3.2; 95%CI 1.2–8.1) and obese pregnant women (OR=7.5; 95%CI 2.9–19.1). Major postpartum hemorrhage only showed greater values in the obese women group (OR=4.1; 95%CI 1.1–15.8). Regarding the newborns, the probability of a low Apgar score at first minute was higher in the Obese Group (OR=5.5; 95%CI 1.2–23.7) and chances of macrosomia were higher in the Overweight Group (OR=2.9; 95%CI 1.3–6.3). Data regarding neonatal hypoglycemia were not conclusive.
CONCLUSION:
Excessive weight (overweight and obesity) during pregnancy increases the chance of maternal complications (gestational diabetes, hypertensive syndrome, and major postpartum hemorrhage) and neonatal outcomes (cesarean delivery, macrosomia, and low Apgar score).
-
Artigos Originais
Influence of cause of death on body and internal organs weight in perinatal autopsies
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):23-28
01-01-2014
Summary
Artigos OriginaisInfluence of cause of death on body and internal organs weight in perinatal autopsies
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):23-28
01-01-2014DOI 10.1590/S0100-72032014000100006
Views90See morePURPOSE:
To evaluate changes in body and internal organ weight of autopsied children in the perinatal period and their relationship with the cause of death.
METHODS:
One hundred and fifty three cases of perinatal autopsies performed at a university hospital in Southeastern Brazil ere included. Information about cause of perinatal death, date of autopsy, gestational age, perinatal weight and organ weight was obtained from the autopsy protocols and medical records of the mother and/or the newborn. Four groups of causes of death were defined: congenital malformations, perinatal hypoxia/anoxia, ascending infection and hyaline membrane. Brain, liver, lungs, heart, spleen, thymus and adrenals were analyzed.
RESULTS:
The weight of children with perinatal hypoxia/anoxi (1,834.6±1,090.1 g versus 1,488 g), hyaline membranes (1,607.2±820.1 g versus 1,125 g) and ascending infection (1,567.4±1,018.9 g versus 1,230 g) was higher than expected for the population. Lung weight was higher in cases with ascending infection (36.6±22.6 g versus 11 g) and lower in cases with congenital malformations (22.0±9.5 g versus 40 g). Spleen weight was higher in children with ascending infection (8.6±8.9 g versus 3.75 g ) and adrenal weight was lower in cases with congenital malformations (3.9±2.1 g versus 5.5 g). Thymus weight was lower in cases with miscellaneous causes (3.7±1.2 g versus 7.5 g) and spleen weight was lower in patients with lung immaturity (0.4±0.1 g versus 1.7 g). All results showed significant differences.
CONCLUSIONS:
This study demonstrates that variations in the weight of children and the weight of their organs are related to the types of cause of perinatal death. These data may contribute to a better interpretation of autopsy findings and their anatomical and clinical relationship.
-
Artigos Originais
Maternal risk factors associated with the necessity of neonatal intensive care unit
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):29-34
01-01-2014
Summary
Artigos OriginaisMaternal risk factors associated with the necessity of neonatal intensive care unit
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(1):29-34
01-01-2014DOI 10.1590/S0100-72032014000100007
Views83See morePURPOSE:
To evaluate the maternal risk factors that require newborn assistance in neonatal Intensive Care Units (ICU).
METHODS:
A prospective observational case-control study was conducted on 222 pregnant women (1:1 case-control ratio) attended at a public maternity. The following variables were analyzed in the puerperae: age at menarche, age at first sexual intercourse, history of chronic diseases, habits, prenatal care, obstetric history, clinical complications during pregnancy and childbirth, and sociodemographic variables. The variables of the newborns were: Apgar scores, gestational age, birth weight, presence or absence of malformation, need for resuscitation, and complications during the first 24 hours. Proportions were compared using the Fisher exact test or the Person γ2 test. Multivariable models were developed by logistic regression analysis using adjusted Odds Ratio with a 95% confidence interval (CI).
RESULTS:
Regarding reproductive history, ≥3 pregnancies and 2 or 3 previous cesareans were sytatistically significant (p=0.0 and 0.0, respectively). Among the complications that required assistance in the neonatal ICU, prematurity was responsible for 61 cases (55.5%), followed by risk of intrapartum infection in 46 cases (41.8%). Regarding the maternal history, the presence of hypertensive disease showed statistical significance (p=0.0). Premature rupture of membranes was strongly associated with the need for the neonatal ICU (Odds Ratio - OR=6.1, 95%CI 2.6-14.4).
CONCLUSIONS:
Premature rupture of membranes and hypertensive disease should receive special attention in prenatal care due to their strong association with newborns requiring assistance in the neonatal ICU.


