Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):327-335
06-27-2022
Determine the predictive criteria for success in inducing labor for live fetuses using misoprostol in pregnant women. Secondarily, the objective is to determine the rates of vaginal or cesarean delivery, duration of induction, interval of administration of misoprostol, the main causes of induction of labor and indication for operative delivery.
Medical records of 873 pregnant women admitted for cervical maturation from January 2017 to December 2018 were reviewed in a descriptive observational study of retrospective analysis, considering the following response variables: age, parity, Bishop Index, doses of misoprostol, labor induction time. Logistic regression models were used to predict success with misoprostol in non-operative deliveries.
Of the 873 patients evaluated, 72% evolved with vaginal delivery, 23% of the cases were cesarean, 5% forceps or vacuum-extractor. For non-operative delivery the predictive variables at admission were age, parity, gestational age and dilation. During hospitalization, fewer vaginal touches,amniotomy or amniorrhexis with clear fluid lead to a shorter induction time and a greater chance of non-operative delivery. False positives and false negatives of the model were always below 50% and correct answers above 65%.
At admission, age less than 24 years, previous normal births, lower the gestational age and greater the dilation, were predictive of greater probability of nonoperative delivery. During hospitalization, the less vaginal touches and occurrence of amniotomy/amniorrhexis with clear liquid indicate shorter induction time. Future studies with a prospective design and analysis of other factors are necessary to assess the replicability, generalization of these findings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):522-528
10-23-2020
To obtain cesarean-section (CS) rates according to the Robson Group Classification in five different regions of Brazil.
A descriptive epidemiological study using data from secondary birth records fromthe Computer Science Department of the Brazilian Unified Health System (Datasus, in Portuguese) between January 1st, 2014, and December 31st, 2016, including all live births in Brazil.
The overall rate of CSwas of 56%. The sample was divided into 11 groups, and vaginal births were more frequent in groups 1 (53.6%), 3 (80.0%) and 4 (55.1%). The highest CS rates were found in groups 5 (85.7%), 6 (89.5%), 7 (85.2%) and 9 (97.0%). The overall CS rate per region varied from 46.2% in the North to 62.1% in the Midwest. Group 5 was the largest obstetric population in the South, Southeast and Midwest, and group 3 was the largest in the North and Northeast. Group 5 contributed the most to the overall CS rate, accounting for 30.8% of CSs.
Over half of the births in Brazil were cesarean sections. The Midwest had the highestCS rates,while theNorth had the lowest. The largestobstetric population in the North and in the Northeast was composed of women in group 3, while in the South, Southeast and Midwest it was group 5. Among all regions, the largest contribution to the overall CS rate was from group 5.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(8):476-484
09-16-2019
Labor induction does not always result in vaginal delivery, and can expose both the mother and the fetus to the risks inherent to the induction procedure or a possible cesarean section. Transvaginal sonography (TVS) of the cervix is a useful tool to predict prematurity; in the present study, this tool was used to evaluate postterm induction.
We evaluated the ultrasound characteristics of the cervix (cervical length, cervical funneling, internal os dilation, the presence or absence of the cervical gland area [CGA], and the morphological changes of the cervix as a result of applying fundal pressure) before the onset of labor induction among women with postterm pregnancy to identify the possible predictors of failed labor induction. The Bishop score (BS) was used for comparison purposes. Three groups were evaluated: successful versus unsuccessful induction; vaginal delivery versus cesarean delivery (excluding cases of acute fetal distress [AFD]); and vaginal delivery versus cesarean delivery (including cases of AFD). A fourth group including only the primiparous women from the three previous groups was also evaluated.
Based on the studied characteristics and combinations of variables, a cervical length ≥ 3.0 cm and a BS ≤ 2 were the best predictors of induction failure.
Although TVS is useful for screening for induction failure, this tool should not be used as an indication for cesarean section.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):363-370
07-22-2019
To evaluate the results of induced labor and to determine the main factors associated with intrapartum cesarean section after patients being submitted to this procedure at the Hospital Universitário of the Universidade Federal de Santa Catarina (HU/UFSC, in the Portuguese acronym), Florianópolis, state of Santa Catarina, Brazil.
A retrospective cross-sectional study that included all the pregnancies that resulted in single-fetus births, whose gestational-age was > 22 weeks and that had been submitted to labor induction at the HU/UFSC in the period from 2013 to 2016.
During the proposed period, 1,491 pregnant women were submitted to the labor induction protocol. In 1,264 cases (84.8%), induction resulted in labor, with 830 (65.7%) progressing to vaginal delivery. Gestational age ≥ 41 + 0 weekswas themost common indication for induced labor (55.2%), and vaginal administration of misoprostol was themost commonly usedmethod (72.0%). Among these pregnant women, the cesarean section rate was of 34.3%. Considering the cases of induction failure, the cesarean section rate rose to 44.3%. The factors associated with cesarean section were: previous history of cesarean delivery (PR [prevalence ratio] = 1.48; 95%CI [confidence interval]: 1.51-1.88), fetuses with intrauterine growth restriction (IUGR) (PR = 1.82; 95%CI: 1.32-2.19), Bishop score ≤ 6 (PR = 1.33; 95%CI: 1.01-1.82), and induction time either < 12 hours (PR = 1.44; 95%CI: 1.17-1.66) or > 36 hours (PR = 1.51; 95% CI 1.22-1.92) between the beginning of the induction and the birth.
Labor induction was successful inmost patients. In the cases in which the final outcome was a cesarean section, the most strongly associated factors were: previous history of cesarean delivery, presence of fetuses with IUGR, and either excessively short or excessively long periods of induction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):53-59
02-01-2017
To evaluate blood loss during misoprostol-induced vaginal births and during cesarean sections after attempted misoprostol induction.
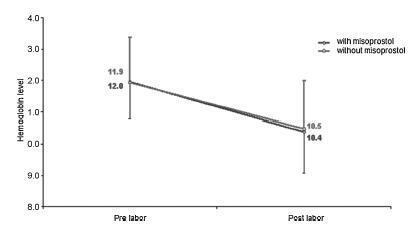
We conducted a prospective observational study in 101 pregnant women indicated for labor induction; pre- and postpartum hemoglobin levels were measured to estimate blood loss during delivery. Labor was induced by administering 25 μg vaginal misoprostol every 6 hours (with a maximum of 6 doses). The control group included 30 patients who spontaneously entered labor, and 30 patients who underwent elective cesarean section. Pre- and postpartum hemoglobin levels were evaluated using the analysis of variance for repeated measurements, showing the effects of time (pre- and postpartum) and of the group (with and withoutmisoprostol administration).
Therewere significant differences between pre- and postpartum hemoglobin levels (p < 0.0001) with regard to misoprostol-induced vaginal deliveries (1.6 ± 1.4 mg/dL), non-induced vaginal deliveries (1.4 ± 1.0 mg/dL), cesarean sections after attempted misoprostol induction (1.5 ± 1.0 mg/dL), and elective cesarean deliveries (1.8 ± 1.1 mg/dL). However, the differences were proportional between the groups with and without misoprostol administration, for both cesarean (p = 0.6845) and vaginal deliveries (p = 0.2694).
Labor induction using misoprostol did not affect blood loss during delivery.