-
Original Article10-01-2016
Value of the Ultrasound in the Study of Ovarian Reserve for Prediction of Oocyte Recovery
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):499-505
Abstract
Original ArticleValue of the Ultrasound in the Study of Ovarian Reserve for Prediction of Oocyte Recovery
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):499-505
Views132See moreAbstract
Purpose
To identify which methods used in the assessment of the ovarian reserve are exclusive or complementary to identify the best response to follicle development.
Methods
Retrospective cohort study, involving patients undergoing assisted reproduction treatment at the Instituto de Medicina Reprodutiva e Fetal, from April 2009 to July 2014. Age, biochemical tests, and ultrasound were assessed. The data were analyzed to predict the follicular development and the relation between them, using, for statistical analysis, Statistical Package for Social Sciences software.
Results
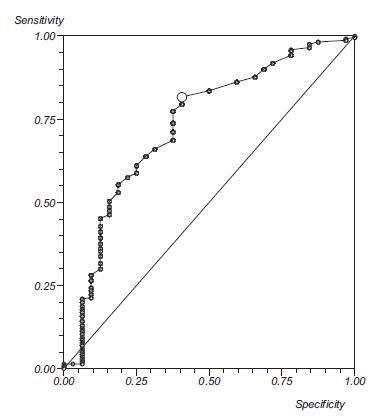
Out of the 293 couples included, 50.2% presented infertility by ovarian factor. Considering the age as the main variable, a significant negative correlation with the volume of both ovaries was observed (right ovary, r = 0.21; left ovary, r =0.22; both p< 0.0001), and with the antral follicle count (right ovary, r =0.38; left ovary, r =0.47; both p< 0.0001). Considering the antral follicle count as the main variable, a significant positive correlation with the total recruited oocytes was observed. When we correlated the antral follicle count with the recruited follicles larger than 18 mm, we observed that, with a cutoff of 12 antral follicles, there is a positive predictive value of 99%, and an area under the ROC curve of 0.76.
Conclusion
We concluded from our study that age and antral follicle count are effective predictors of ovarian response in cycles of assisted reproduction. The ovarian volume, as well as the anti-Müllerian hormone dosage, seem to be adequate markers of the ovarian reserve.
-
Review Article11-01-2015
Limitations and controversies in determining the predictive value of oocyte and embryo morphology criteria
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):533-546
Abstract
Review ArticleLimitations and controversies in determining the predictive value of oocyte and embryo morphology criteria
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):533-546
DOI 10.1590/SO100-720320150005330
Views99See moreIn order to increase the success rate of in vitro fertilization cycles, several studies have focused on the identification of the embryo with higher implantation potential. Despite recent advances in the reproductive medicine, based on the OMICs technology, routinely applicable methodologies are still needed. Thus, in most fertilization centers embryo selection for transfer is still based on morphological parameters evaluated under light microscopy. Several morphological parameters may be evaluated, ranging from the pronuclear to blastocyst stage. In general, despite the day of transfer, some criteria are suggested to present a predictive value for embryo viability when analyzed independently or combined. However, the subjectivity of morphological evaluation, as well as the wide diversity of embryo classification systems used by different fertilization centers shows contrasting results, making the implementation of a consensus regarding different morphological criteria and their predictive value a difficult task. The optimization of embryo selection represents a large potential to increase treatment success rates, allowing the transfer of a reduced number of embryos and inimizing the risks of multiple pregnancy.
-
Review Article03-25-2013
Clinical use for anti-mullerian hormone in gynecology
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(3):136-140
Abstract
Review ArticleClinical use for anti-mullerian hormone in gynecology
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(3):136-140
DOI 10.1590/S0100-72032013000300008
Views83See moreAnti-mullerian hormone (AMH) is a glycoprotein produced by granulosa cells of primary, pre-antral and small antral ovarian follicles and its clinical applicability has been recently demonstrated by several studies. Prediction of the response to ovarian stimulation for in vitro fertilization corresponds to the most frequent utilization of AMH in clinical practice, being routinely assessed in many services to identify subgroups of women susceptible to a poor response or to Ovarian Hyperstimulation Syndrome. There are great perspectives that AMH may be applicable to the individual determination of risk for iatrogenic gonadal injury in women with neoplasms who will be submitted to chemotherapy. It is also probable that AMH assessment will be included in protocols for the investigation of amenorrhea and oligomenorrhea, since AMH levels are increased in Polycystic Ovary Syndrome, reduced in premature ovarian failure and normal in other conditions such as hyperprolactinemia and hypogonadotropic hypogonadism. It is possible that AMH will be utilized in the future for the prediction of age at menopause and of reproductive prognosis, providing solid bases for pre-conceptive and contraceptive counseling.
-
Original Article01-17-2010
Concentration of steroid hormones in the follicular fluid of mature and immature ovarian follicles of patients with polycystic ovary syndrome submitted to in vitro fertilization
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):447-453
Abstract
Original ArticleConcentration of steroid hormones in the follicular fluid of mature and immature ovarian follicles of patients with polycystic ovary syndrome submitted to in vitro fertilization
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):447-453
DOI 10.1590/S0100-72032010000900006
Views106See morePURPOSE: to evaluate the concentration of steroid hormones in follicular fluid (FF) of small (10-14 mm) and large (> 18 mm) follicles of women with polycystic ovary syndrome (PCOS) submitted to controlled ovarian hyperstimulation (COH) and in vitro fertilization (IVF) cycles. METHODS: a case-control study was conducted on 13 infertile women with PCOS (17 cycles) and 31 infertile women due to male factor - Control Group (31 cycles). FF was aspirated individually and divided into four groups: G1 (FF of small follicles of the Control Group), G2 (FF of small follicles of the PCOS group), G3 (FF of large follicles of the Control Group) and G4 (FF of large follicles of the PCOS group). Estrogen, progesterone and β-hCG were determined by chemiluminescence, and testosterone and androstenedione by radioimmunoassay. The unpaired t-test was used to compare the hormone determinations in the FF of the PCOS and Control Groups, and the four groups were compared by ANOVA. Fisher's exact test was used to compare the pregnancy rates. RESULTS: the small follicles of the two groups had lower progesterone levels (8,435±3,305 ng/mL) than large follicles (10,280±3,475 ng/mL), p-value <0.01. The progesterone levels of all follicles of group PCOS (8,095±4,151 ng/mL) were lower than Control (9,824±3,128 ng/mL), p-value =0.03. Testosterone differed between G1 (326.6±124.4 ng/dL) and G3 (205.8±98.91 ng/dL), p-value <0.001, and between G3 (205.8±98.91 ng/dL) and G4 (351.10±122.1ng/dL), p-value <0.001. Small follicles had higher testosterone levels (508.9±266 ng/dL) than large follicles (245.10±123 ng/dL), p-value <0.0001. The pregnancy rates did not differ between the PCOS (5/13, 38.5%) and the Control groups (9/31, 40.9%), p-value =072. CONCLUSIONS: women with PCOS had high testosterone concentrations in the FF, regardless of the stage of follicle development, and reduced progesterone levels, suggesting that paracrine factors may inhibit the secretion of the latter by follicular cells. The pregnancy rates showed that treatment with COH and IVF is a good option for women with infertility secondary to PCOS.
-
Original Article03-20-1999
Clinical Treatment Evaluation of Endometriosis
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(2):85-90
Abstract
Original ArticleClinical Treatment Evaluation of Endometriosis
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(2):85-90
DOI 10.1590/S0100-72031999000200005
Views106See morePurpose: to present a profile of endometriosis, stages and results of treatment among the patients seen in our Service. Methods: the medical records of 155 patients with endometriosis treated during the period from 1991 to 1996 according to a preestablished protocol were examined. Results: mean patient age was 31 years, most patients were white, with regular menstrual cycles. The most frequently observed symptoms were dysmenorrhea, pelvic pain and infertility and were mild in most of the cases. The diagnostic methods utilized were laparoscopy or echography. There was agreement between echography and laparoscopy in 96% of cases. Laparotomy was required in 28% of cases for diagnostic elucidation and/or treatment. Endometrioma was detected in 37% of the cases and endometriosis was confirmed in only 74% of the biopsies from the lesion by anatomopathological examination. There was a significant improvement with clinical treatment regardless of the drug used, with improved symptoms in approximately 50% of the patients. Assisted fertilization was performed in 34 patients, consisting of in vitro fertilization (IVF) for 80% of them, with a 27% pregnancy/transfer rate. Conclusions: the diagnostic method of choice should be laparoscopy, although echography presented a high rate of agreement. Anatomopathological examination of the lesions should be used as an adjuvant method in the diagnosis since it is not confirmatory in all of the cases. Clinical treatment with assisted reproductive technologies is a good therapeutic option, especially with the use of IVF.
-
Original Article03-19-2006
In vitro fertilization outcome for women previously submitted to tubal sterilization
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(12):715-720
Abstract
Original ArticleIn vitro fertilization outcome for women previously submitted to tubal sterilization
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(12):715-720
DOI 10.1590/S0100-72032006001200005
Views132PURPOSE: to investigate the effects of previous bilateral tubal sterilization on the outcome of in vitro fertilization. METHODS: retrospective study of 98 consecutive in vitro fertilization cycles. Fifty-five women with previous tubal sterilization without any other infertility factor (TL group) were compared with 43 women with infertility due only to mild male factor (MI group. Age, cancellation rate per induction cycle, response to ovulation induction (number of days of ovulation induction, total amount of gonadotrophin units used, number of follicles and oocytes retrieved), fertilization and cleavage rates, number of transferred embryos and clinical pregnancy per transfer cycle were the variables considered. RESULTS: the cycle discontinuation rate due to poor response, results of ovulation induction, fertilization and cleavage rates, number of transferred embryos and the occurrence of clinical pregnancy were similar in both groups. Considering solely the variable age in TL group, we observed that patients older than 35 years required higher gonadotrophin doses during ovulation induction (2445 versus 2122 IU), presented lower response with fewer follicular growth (11.3 versus 15.8) and less oocytes retrieved (6.1 versus 8.5) compared to younger women (34 years old or less). CONCLUSIONS: tubal sterilization did not interfere with in vitro fertilization outcomes. We observed a worse response to ovulation induction in women older than 35 years, who had previous tubal sterilization.
Key-words Embryo transferIn vitro fertilizationOvulation InductionReproductive techniques, assistedSterilization, tubalSee more -
Original Article08-07-1999
Human embryo coculture in vero cells and blastocyst stage transfer
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(7):409-414
Abstract
Original ArticleHuman embryo coculture in vero cells and blastocyst stage transfer
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(7):409-414
DOI 10.1590/S0100-72031999000700007
Views68See morePurpose: to determine whether the transfer day or the stage that the embryo is transferred interferes in pregnancy and implantation rates. Methods: oocytes we recovered from 107 patients and submitted to in vitro fertilization. The embryos were cocultured on Vero cells and transferred on day 3 or day 5 post-fertilization, after morphological assessment. Results: the implantation rate of the transferred embryos on day 5 was significantly higher than when the embryos were transferred on day 3, but the pregnacy rates did not change. However, a significant difference was observed in the pregnancy rates for embryos transferred at the expanded blastocyst stage (70.6% of pregnancy) when compared to 20.0% and 10.5% at the earlier blastocyst and morula stages, respectively. Conclusions: the implantation and pregnancy rates were significantly increased when the embryos were transferred at the expanded blastocyst stage, but the culture media and culture conditions now available are not able to provide a satisfactory rate at this stage.
-
Original Article06-19-2006
The pregnancy rate in women submitted to assisted reproduction techniques is lower after the age of 30 years
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(1):32-37
Abstract
Original ArticleThe pregnancy rate in women submitted to assisted reproduction techniques is lower after the age of 30 years
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(1):32-37
DOI 10.1590/S0100-72032006000100006
Views125PURPOSE: to evaluate the rate of chemically diagnosed pregnancy (serum beta-HCG>25 mIU/mL levels obtained fourteen days after the embryonic transfer) clinically diagnosed pregnancy (gestational sac visualized by ultrasound four to six weeks after the embryonic transfer) and miscarriage rates in women submitted in vitro fertilization to (IVF) and intracytoplasmic sperm injection (ICSI) in a tertiary center of assisted reproduction and to correlate these rates with age. METHODS: retrospective transverse study with analysis of 1016 cycles of controlled ovarian hyperstimulation of 932 infertile women with indication of IVF (370 cycles) or ICSI (646 cycles). The patients' age ranged from 22 to 46 years. All women with age over 35 years included in the study had FSH<15 IU/L. The studied cycles were divided into two groups: the first including the cycles referring to women of 22 to 30 years and the second group, to those of 31 to 46 years. The studied variables were: pregnancy (chemical or clinical) and miscarriage rates. The chi2 test was used to compare these rates between the groups. RESULTS: the total pregnancy rate was 36.42%, with a significant reduction starting at 30 years (p=0.0001). From 22 to 30 years (303 cycles) the pregnancy rate was 45.4%, while in the range from 31 to 46 years (713 cycles), it was 25.1%. The miscarriage rates were, 10.2 11,6%, respectively (p=0.6854). CONCLUSION: although the miscarriage rates did not differ between the groups, a decrease in the pregnancy rate of infertile women submitted to IVF or ICSI was observed after the age of 30 years. Thus, we recommend the gynecologists not to postpone the investigation and the referral for treatment of infertility.
Key-words Assisted reproductive techniquesFertilityIn vitro fertilizationOocytesSperm injections, intracytoplasmicSee more


