Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1102-1109
To evaluate the use of misoprostol prior to hysteroscopy procedures regarding technical ease, the presence of side effects, and the occurrence of complications.
This is a retrospective, observational, analytical, case-control study, with the review of medical records of 266 patients followed-up at the Gynecological Videoendoscopy Sector of the Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto of the Universidade de São Paulo (HCFMRP – USP, in the Portuguese acronym) from 2014 to 2019, comparing 133 patients who used the drug before the procedure with 133 patients who did not.
The occurrence of postmenopausal uterine bleeding was the main indication for hysteroscopy and revealed a statistical difference between groups (p < 0.001), being present in 93.23% of the patients in the study group and in 69.7% of the patients in the control group. Only 2 patients (1.5%) in the study group reported adverse effects. Although no statistical differences were observed regarding the occurrence of complications during the procedure (p = 0.0662), a higher total number of complications was noted in the group that used misoprostol (n = 7; 5.26%) compared with the group that did not use the drug (n = 1; 0.75%), a fact that is clinically relevant. When evaluating the ease of the technique (measured by the complete performance of all steps of the hysteroscopy procedure), it was verified that although there was no difference between groups (p = 0.0586), the control group had more than twice as many incompletely performed procedures (n = 17) when compared with the group that used misoprostol previously (n = 8), which is also clinically relevant.
The use of misoprostol prior to hysteroscopy in our service indicated that the drug can facilitate the performance of the procedure, but not without side effects and presenting higher complication rates.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(7):530-534
To evaluate the accuracy of transvaginal ultrasound in the diagnosis of intrauterine lesions, using hysteroscopy as the gold standard.
This was a prospective observational study with 307 patients. All patients underwent hysteroscopy after a previous transvaginal ultrasound to compare the results. The hysteroscopy was performed by experienced examiners, and transvaginal ultrasounds were performed in various public and private services, which is reflective of routine healthcare practices in obstetrics and gynecology. The sensitivity, specificity, and accuracy of the transvaginal ultrasound were calculated using hysteroscopy as the gold standard. The level of agreement between the two exams was calculated using the Kappa test.
Themean age was 56.55±12.3 years. For endometrial polyps, we observed a sensitivity of 39.8%, specificity of 72.7%, accuracy of 52.8%, and Kappa index of 0.11 (p=0.025). For fibroids, the sensitivity was 46.7%, specificity was 95.0%, accuracy was 87.9%, and Kappa index was 0.46 (p<0.001). For endometrial thickening, the sensitivity was 68.7%, specificity was 41.7%, accuracy was 47.6%, and Kappa index was 0.06 (p=0.126). For endometrial atrophy, we found a sensitivity of 6.7%, specificity of 99.3%, accuracy of 90.2%, and Kappa index of 0.10 (p=0.006). For the other findings, the sensitivity was 15.6%, specificity was 99.6%, accuracy was 87.3%, and Kappa index was 0.23 (P<0.001).
Our study demonstrated a low level of accuracy of transvaginal ultrasound for the diagnosis of endometrial lesions, when performed by a non-experienced professional. Thus, it is important to consider the use of hysteroscopy to avoid unnecessary and inappropriate treatments.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):35-40
To evaluate the presence of residual disease in the uterine specimen after hysteroscopic polypectomy or polyp biopsy in patients with endometrioid endometrial cancer (EC).
We analyzed a series of 104 patients (92 cases from the Hospital AC Camargo and 12 from the Hospital do Servidor Público Estadual de São Paulo) with polyps that were diagnosed by hysteroscopy, showing endometrioid EC associated with the polyp or in the final pathological specimen. Patients underwent a surgical approach for endometrial cancer from January 2002 to January 2017. Their clinical and pathological data were retrospectively retrieved from the medical records.
In78cases (75%), thepolyphad EC, and in 40(38.5%), itwas restricted tothe polyp, without endometrial involvement. The pathologic stage was IA in 96 cases (92.3%) and 90 (86.5%) had histologic grade 1 or 2. In 18 cases (17.3%), there was no residual disease in the final uterine specimen, but only in 9 of them the hysteroscopy suggested that the tumor was restricted to the polyp. In 5 cases (4.8%) from the group without outside of the polyp during hysteroscopy, myometrial invasion was noted in the final uterine specimen. This finding suggests the possibility of disease extrapolation through the base of the polyp.
Patients with endometrioid EC associated with polyps may have the tumor completely removed during hysteroscopy, but the variables shown in the present study could not safely predict which patient would have no residual disease.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(10):649-658
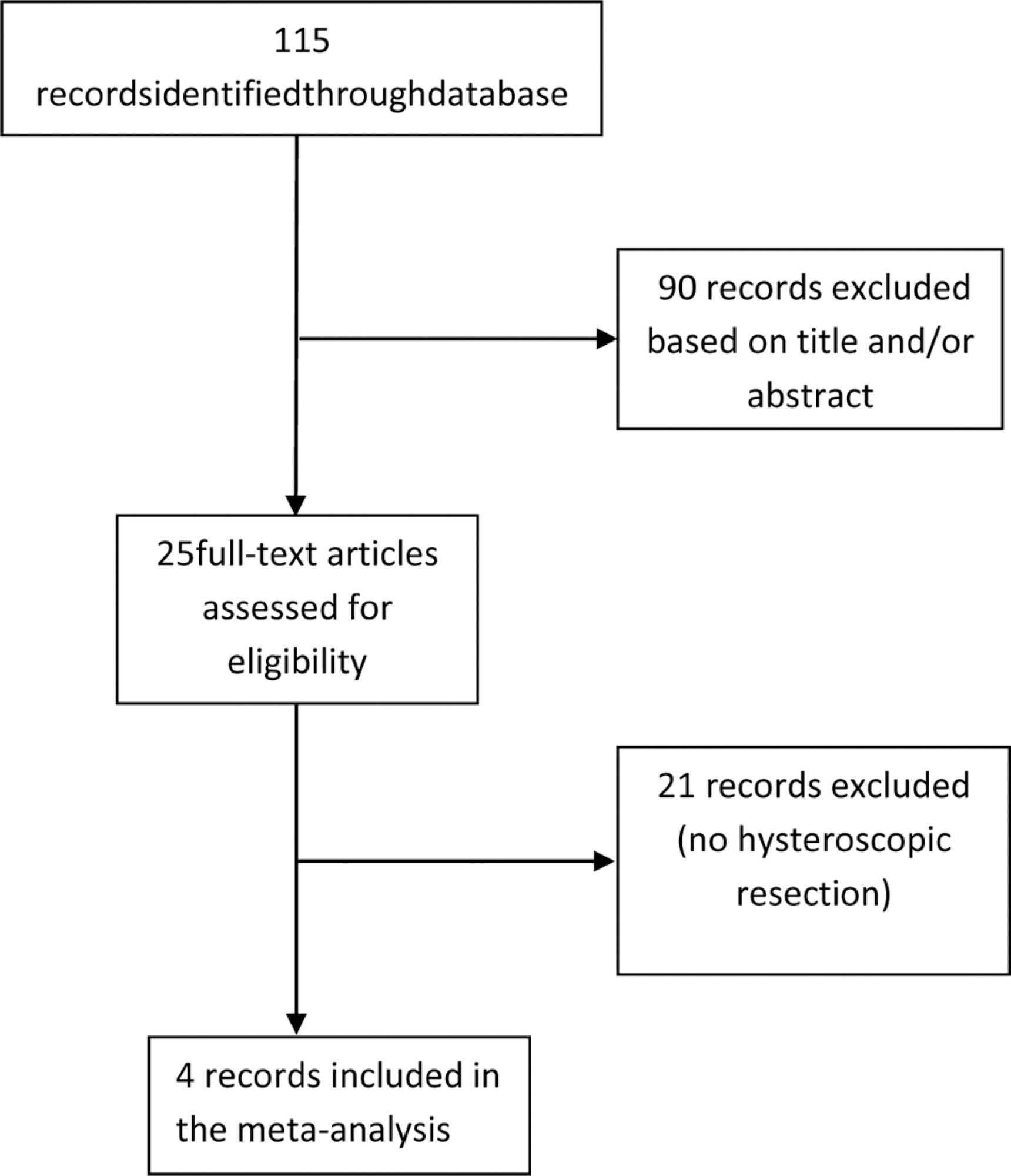
Gonadotropin-releasing hormone analogues (GnRH-a) have been used preoperatively before hysteroscopic myomectomy to decrease the size and vascularization of the myomas, but evidence to support this practice is weak. Our objective was to analyze the use of GnRH-a in the reduction of submucous fibroid as a facilitator for surgical hysteroscopy from published clinical trials.
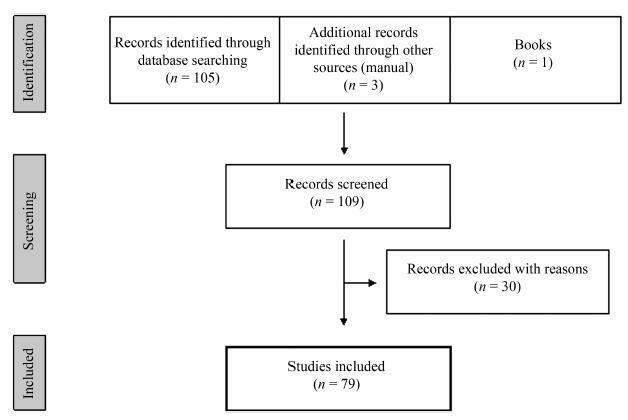
Studies from electronic databases (Pubmed, Scielo, EMBASE, Scopus, PROSPERO), published between 1980 and December 2018. The keywords used were fibroid, GnRH analogue, submucous, histeroscopy, histeroscopic resection and their correspondents in Portuguese.
The inclusion criteria were controlled trials that evaluated the GnRH-a treatment before hysteroscopic resection of submucous myomas. Four clinical trials were included in the meta-analysis.
Two review authors extracted the data without modification of the original data, using the agreed form. We resolved discrepancies through discussion or, if required, we consulted a third person.
The present meta-analysis included a total of 213 women and showed no statistically significant differences in the use of GnRH-a compared with the control group for complete resection of submucous myoma (relative risk [RR]: 0.94; 95%; confidence interval [CI]: 0.80-1.11); operative time (mean difference [MD]: - 3.81; 95%;CI : - 3.81-2.13); fluid absorption (MD: - 65.90; 95%;CI: - 9.75-2.13); or complications (RR 0.92; 95%;CI: 0.18-4.82).
The present review did not support the routine preoperative use of GnRH-a prior to hysteroscopic myomectomy. However, it is not possible to determine its inferiority when compared with the other methods due to the heterogeneity of existing studies and the small sample size.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):415-419
It is estimated that around 28 million surgeries will be postponed or canceled worldwide as a result of this pandemic, causing a delay in the diagnosis and treatment of more than 2 million cancer cases. In Brazil, both the National Health Agency (ANS) and National Health Surveillance Agency (ANVISA) advised the postponement of elective and non-essential surgeries, causing a considerable impact on the number of surgical procedures that decreased by 33.4% in this period. However, some women need treatment for various gynecological diseases that cannot be postponed. The purpose of this article is to present recommendations on surgical treatment during the COVID-19 pandemic.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(6):325-332
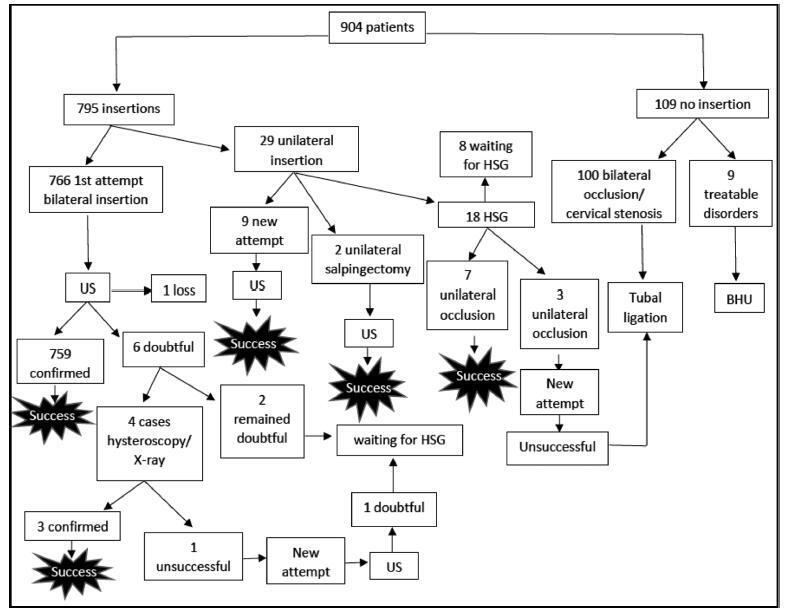
To evaluate the insertion of the hysteroscopic intratubal sterilization device for female sterilization concerning the technique and the feasibility.
Retrospective study with data collection of medical records of 904 patients who underwent device insertion between January and September 2016 in a public hospital in Rio de Janeiro (Brazil) with data analysis and descriptive statistics.
In 85.8% of the cases, the uterine cavity was normal, and themost commonlydescribed findings upon hysteroscopy were synechiae (9.5%). The procedure lasted an average of 3.56minutes (range: 1 to 10minutes), and the pain was considered inexistent or mild in 58,6% of the cases, mild or moderate in 32,8%, and severe or agonizing in less than 1% (0.8%) of the cases, based on a verbal scale ranging from 0 to 10. The rate of successful insertions was of 85.0%, and successful tubal placement was achieved in 99.5% of the cases. There were no severe complications related to the procedure, but transient vasovagal reactions occurred in 5 women (0.6%).
Female sterilization performed by hysteroscopy is a safe, feasible, fast, and well-tolerated procedure. The rates of successful insertions and tubal placements were high. There were few and mild adverse effects during the procedure, and there were no severe complications on the short term.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):409-411
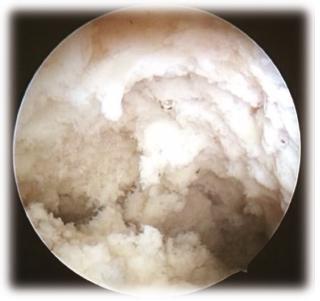
Endometrial tuberculosis is a rare diagnosis in the postmenopausal period, and it can mimic a carcinoma. The present article describes the case of a 54-year-old female patient with weight loss, abdominal pain, and ascites. An ultrasonography showed endometrial thickening, and a video hysteroscopy revealed a uterine cavity with formations with cotton aspect covering the entire endometrial surface and the tubal ostia. An anatomopathological evaluation diagnosed endometrial tuberculosis. The treatment was with a standardized therapeutic scheme (ethambutol, isoniazid, pyrazinamide and rifampicin), and the patient evolved with clinical improvement and normal uterine cavity at hysteroscopy. Considering the lack of pathognomonic hysteroscopic findings of the disorder, it is important to disclose the images of the case.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):44-52
The aim of the present study was to perform a comprehensive review of the literature to provide a complete and clear picture of isthmocele-a hypoechoic area within themyometriumat the site of the uterine scar of a previous cesarean section-by exploring in depth every aspect of this condition.
A comprehensive review of the literature was performed to identify the most relevant studies about this topic.
Every aspect of isthmocele has been studied and described: pathophysiology, clinical symptoms, classification, and diagnosis. Its treatment, both medical and surgical, has also been reported according to the actual literature data.
Cesarean section is the most common surgical procedure performed worldwide, and one of the consequences of this technique is isthmocele. A single and systematic classification of isthmocele is needed to improve its diagnosis and management. Further studies should be performed to better understand its pathogenesis.