Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):541-548
DOI 10.1590/S0100-72032010001100005
PURPOSE: to reassess the adrenal function of patients with PCOS after the introduction of the Rotterdam's criteria. METHODS: descriptive and cross-sectional study including 53 patients 26±5.1 years old. Glucose, glycosylated hemoglobin, lipids, estradiol, progesterone, 17-OHP4, DHEAS, FSH, LH, TSH, PRL, androstenedione, free thyroxine, insulin, total testosterone, SHBG, and free androgen index were measured. Insulin resistance was considered to be present with a homeostatic model assessment index >2.8. The adrenal response to cortrosyn was assessed by the hormonal rise observed at 60 minutes, and by the area under the response curve. RESULTS: biochemical hyperandrogenism was found in 43 of 53 eligible patients (81.1%). Thirty-three women had adrenal hyperandrogenism (62.2%). The weight of these 33 women, aging 25.1±5.0 years, was 74.9±14.9 kg, BMI was 28.8±6.0 and the waist/hip ratio was 0.8±0.1. DHEAS was >6.7 nmol/L in 13 (39.4%) and androstenendione was >8.7 nmol/L in 31 (93.9%). The increments in 17-OHP4, cortisol, A, and progesterone were 163%, 153%, 32%, and 79%, respectively. The homeostatic insulin resistance model was >2.8 in 14 (42.4%). Insulin and estradiol were not correlated with cortisol or androgens. CONCLUSIONS: the use of multiple endocrine parameters showed a high prevalence of biochemical hyperandrogenism in patients with PCOS. Two thirds of the patients had adrenal hyperandrogenism, and estradiol and insulin did not influence adrenal secretion.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):447-453
DOI 10.1590/S0100-72032010000900006
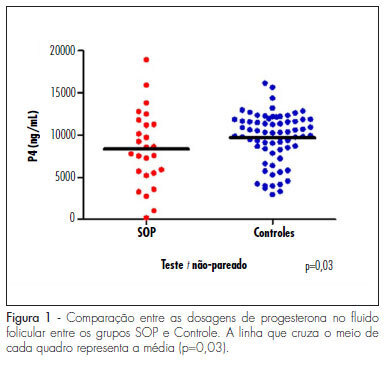
PURPOSE: to evaluate the concentration of steroid hormones in follicular fluid (FF) of small (10-14 mm) and large (> 18 mm) follicles of women with polycystic ovary syndrome (PCOS) submitted to controlled ovarian hyperstimulation (COH) and in vitro fertilization (IVF) cycles. METHODS: a case-control study was conducted on 13 infertile women with PCOS (17 cycles) and 31 infertile women due to male factor - Control Group (31 cycles). FF was aspirated individually and divided into four groups: G1 (FF of small follicles of the Control Group), G2 (FF of small follicles of the PCOS group), G3 (FF of large follicles of the Control Group) and G4 (FF of large follicles of the PCOS group). Estrogen, progesterone and β-hCG were determined by chemiluminescence, and testosterone and androstenedione by radioimmunoassay. The unpaired t-test was used to compare the hormone determinations in the FF of the PCOS and Control Groups, and the four groups were compared by ANOVA. Fisher's exact test was used to compare the pregnancy rates. RESULTS: the small follicles of the two groups had lower progesterone levels (8,435±3,305 ng/mL) than large follicles (10,280±3,475 ng/mL), p-value <0.01. The progesterone levels of all follicles of group PCOS (8,095±4,151 ng/mL) were lower than Control (9,824±3,128 ng/mL), p-value =0.03. Testosterone differed between G1 (326.6±124.4 ng/dL) and G3 (205.8±98.91 ng/dL), p-value <0.001, and between G3 (205.8±98.91 ng/dL) and G4 (351.10±122.1ng/dL), p-value <0.001. Small follicles had higher testosterone levels (508.9±266 ng/dL) than large follicles (245.10±123 ng/dL), p-value <0.0001. The pregnancy rates did not differ between the PCOS (5/13, 38.5%) and the Control groups (9/31, 40.9%), p-value =072. CONCLUSIONS: women with PCOS had high testosterone concentrations in the FF, regardless of the stage of follicle development, and reduced progesterone levels, suggesting that paracrine factors may inhibit the secretion of the latter by follicular cells. The pregnancy rates showed that treatment with COH and IVF is a good option for women with infertility secondary to PCOS.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):334-339
DOI 10.1590/S0100-72032010000700005
PURPOSE: to evaluate clinical and laboratory characteristics of first-degree male relatives of patients with a confirmed diagnosis of polycystic ovary syndrome (PCOS) and to compare the findings with a control group with no family history of PCOS. METHODS: we randomly selected 28 male individuals aged 18 to 65 years who were first-degree relatives of women diagnosed with PCOS and 28 controls matched for age, waist and body mass index (BMI). RESULTS: men with 1st degree kinship with women with PCOS had higher levels of triglycerides (189.6±103.1 versus 99.4±37.1, p<0.0001), Homeostasis Model Assessment (HOMA-IR) (3.5±9.1 versus 1.0±1.0, p=0.0077) and glucose (130.1±81.7 versus 89.5±7.8, p=0.005), and lower levels of sex hormone binding globulin (SHBG) (23.8±13.8 versus 31.1±9.1, p=0.003). SHBG levels correlated independently with triglyceride levels. These individuals also had more clinical signs of hyperandrogenism. CONCLUSIONS: male individuals who are first-degree relatives of patients with PCOS have a higher degree of dyslipidemia and insulin resistance, lower levels of SHBG, and more evident clinical signs of hyperandrogenism. These findings suggest that insulin resistance may be of hereditary origin in individuals with a family history of PCOS regardless of anthropometric parameters.