-
Review Article
Efficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
04-30-2025
Summary
Review ArticleEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
04-30-2025Views51Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term "tranexamic acid". Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Key-words Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomySee more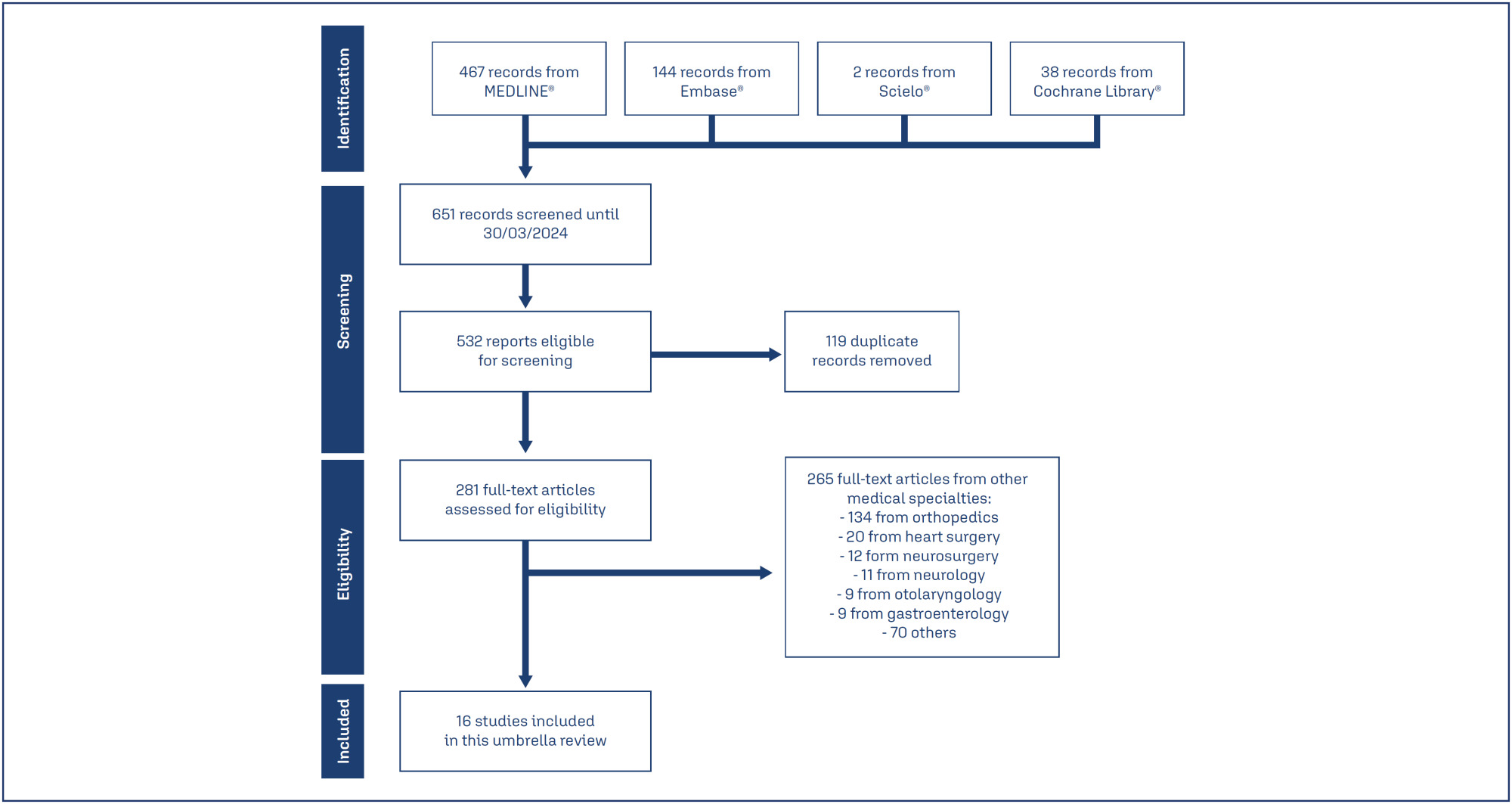
-
Case Report
Refractory Severe Thrombocytopenia during Pregnancy: How to Manage
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):803-807
12-01-2018
Summary
Case ReportRefractory Severe Thrombocytopenia during Pregnancy: How to Manage
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):803-807
12-01-2018Views142Abstract
Thrombocytopenia is the most common hemostatic change in pregnancy, but severe thrombocytopenia is rare. One of the causes, immune thrombocytopenic purpura (ITP), is characterized by increased platelet destruction by immunoglobulin G (IgG) antibodies, presenting a high risk of hemorrhage for the patient, but also for the fetus, since antibodiesmay cross the placenta.We present the case of a 23-year-old pregnant woman with a history of Langerhans cell histiocytosis of the mandible submitted to surgery and chemotherapy when she was 10 years old, with diagnosis of ITP since then. At 28 weeks of gestation, she presented with petechiae, epistaxis, and gingival bleeding, with a platelet count of 3 x 109/L and positive IgG antiplatelet antibodies test. At a multidisciplinary discussion, it was decided to delay a cesarean section, due to the absence of fetal distress and to the high risk of morbidity for the patient. Many therapies were attempted without success. The IgG produced a slight and transient increase in the platelet count. On the 36th week of gestation, an elective cesarean section was performed. The perioperative period transfusions were guided by rotational thromboelastometry (ROTEM) monitoring. The procedure was performed under general anesthesia and videolaryngoscopy-assisted intubation. The patient was hemodynamically stable, without significant bleeding, and was transferred to the intensive care unit. The platelet count eventually decreased and a splenectomy was performed. Regional anesthesia may be contraindicated, and general anesthesia is associated with an increased risk of airway hemorrhage due to traumatic injury during the tracheal intubation and of hemorrhage associated with the surgical procedure. A multidisciplinary approach is essential in high-risk cases.
Key-words Hemorrhageidiopathic thrombocytopenic purpuraPregnant womanThrombocytopeniathromboelastometrySee more -
Relato de Caso
Complete Mole in Twin Pregnancy: a Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(7):415-419
04-09-1998
Summary
Relato de CasoComplete Mole in Twin Pregnancy: a Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(7):415-419
04-09-1998DOI 10.1590/S0100-72031998000700008
Views74Twin pregnancy in which a normal fetus and a complete mole develop at the same time is a rare event. Clinical complications and malignancy are frequent in this type of disease.This report is about a case of a late diagnosis due to the presence of the fetus. The diagnosis was made when the pregnancy was interrupted and then confirmed by histopathological study and flow cytometry. The pregnancy was terminated transpelvically due to massive uterine hemorrhage. The post-molar follow-up showed the persistence of high levels of bhCG. The patient's complete recovery was achieved after the administration of methotrexate. The diagnosis, natural history, and procedures for this rare disease are discussed in view of this case.
Key-words ChemotherapyComplete hydatidiform moleGestational trophoblastic diseaseHemorrhagePregnancy complicationsTwin pregnancyUltrasonographySee more -
Artigos Originais
Maternal mortality: 75 years of observations in a teaching maternity hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):380-387
12-06-2006
Summary
Artigos OriginaisMaternal mortality: 75 years of observations in a teaching maternity hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):380-387
12-06-2006DOI 10.1590/S0100-72032006000700002
Views56PURPOSE: to evaluate all maternal deaths that occurred between 1927 and 2001, among 164,161 patients admitted to the Maternidade Therezinha de Jesus, the obstetrical service of the "Universidade Federal de Juiz de Fora", Brazil. METHODS: a retrospective study of 144 maternal deaths that occurred in the maternity hospital in 75 years, with 131,048 live births in the same period of time, analyzing all patients's records regarding their clinical history and data from death certificates. Autopsies were not performed. Data obtained were age, parity, gestation length, complications, moment, and causes of death. The index of maternal mortality (IMM) period 100 thousand live births was utilized. For statistical analysis the chi2 test and the exponential smoothing technique were used (alpha=0.05). RESULTS: IMM decreased from 1544 in the period 1927-1941 to 314 (p<0.001) between 1942 and 1956 and from 1957 to 1971 it was reduced to 76.4 per 100 thousand live births (p<0.001). Nevertheless, since 1972 there was no further significant improvement (IMM=46 in the last 15 years, p=0.139). Maternal mortality was more frequent in the 15 to 39 years age group, in nulliparous patients with term pregnancies and mostly in the immediate postpartum period (53%). Direct obstetric causes occurred in 79.3% and indirect causes in 20.7% of the cases. Analyzing the evolution of the causes of death, it was found that in the first period of time the most frequent direct obstetric causes in descending order were puerperal infection, eclampsia and uterine rupture, while in the second period they were prepartum hemorrhage and eclampsia, and from 1977 to 2001 hemorrhage, abortion and preeclampsia. Analysis of the past 15 years showed the absence of maternal deaths by either preeclampsia or puerperal infection and the main causes were peripartum hemorrhage, abortion and indirect obstetrical causes. Relating maternal mortality to the type of delivery by the relative risk between cesarean section and vaginal delivery, it was found that when the indication of cesarean section is inevitable its risk is lower (relative risk = 0.6) than through vaginal delivery. CONCLUSIONS: despite the reduction along the 75 years of study, maternal mortality of 46 per 100,000 live births is still very high, and there was no significant decrease since 1972. Many deaths are avoidable. Hemorrhage is at present the most frequent cause of maternal death, the decision to intervene should be fast, and a proper indication for a cesarean section is a safe option. Maternal mortality caused by abortion is increasing alarmingly and family planning is essential.
Key-words AbortionEclampsiaHemorrhageMaternal mortalityPreeclampsiaPuerperal infectionRetrospective studiesSee more -
Revisão
Endometrial polyps
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(5):289-292
08-26-2005
Summary
RevisãoEndometrial polyps
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(5):289-292
08-26-2005DOI 10.1590/S0100-72032005000500010
Views62See moreEndometrial polyps are benign lesions, with a low potential of malignancy. In the reproductive period their diagnosis is established in symptomatic patients with abnormal uterine bleeding or infertility. Postmenopausal women are mostly asymptomatic but in approximately one third of the cases there is an association with abnormal bleeding. They are more frequent after the menopause and risk factors of cancer of the endometrium have not been associated in the same way as risk for endometrial polyps, although they are hormone-dependent as in patients in use of tamoxifen, for instance. Their definitive diagnosis is established by hysteroscopy-guided biopsy and their most effective treatment is hysteroscopic resection. Polyps may recur after treatment. Polypectomy is highly satisfactory after the menopause, is less successful in symptomatic women in the reproductive period and improves fertility rates in infertile women.


