Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):834-840
01-11-2020
Thrombocytopenia, defined as platelet count < 150,000mm3, is frequently diagnosed by obstetricians since this parameter is included in routine surveillance during pregnancy, with an incidence of between 7 and 12%. Therefore, decisions regarding subsequent examination and management are primordial. While most of the cases are due to physiological changes, as gestational thrombocytopenia, other causes can be related to severe conditions that can lead to fetal or maternal death. Differentiating these conditions might be challenging: they can be pregnancy-specific (pre-eclampsia/ HELLP syndrome [hemolysis, elevated liver enzymes, low platelets]), or not (immune thrombocytopenia purpura, thrombotic thrombocytopenic purpura or hemolytic uremic syndrome). Understanding the mechanisms and recognition of symptoms and signs is essential to decide an adequate line of investigation. The severity of thrombocytopenia, its etiology and gestational age dictates different treatment regimens.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(10):669-671
12-21-2020
The present report describes the case of a 31-year-old primigravida, with dichorionic twins at 31 weeks. She presented with history of myalgia, jaundice, and abdominal discomfort. No flu-like symptoms as fever or cough. She was not aware of exposure to COVID-19. Normal blood pressure and O2 saturation. Laboratory tests showed platelet count of 218,000 mm3, alanine aminotransferase (ALT) 558 IU and serum creatinine 2.3 mg/dl. Doppler ultrasound in one twin was compatible with brain sparing. Partial hemolysis, elevated liver enzymes, low platelet count (HELLP) syndrome was the hypothesis, and a cesarean section was performed. On day 2, the white-cell count reached 33,730, with decreased consciousness and mild respiratory distress. Tomography revealed both lungs with ground-glass opacities. Swab for COVID-19 polymerase chain reaction (PCR) was positive. Thrombocytopenia in patients with COVID-19 appears to be multifactorial, similar to what occurs in preeclampsia and HELLP syndrome. We assume that the synergism of these pathophysiological mechanisms could accelerate the compromise of maternal conditions and could be a warning to the obstetric practice.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):496-512
09-01-2017
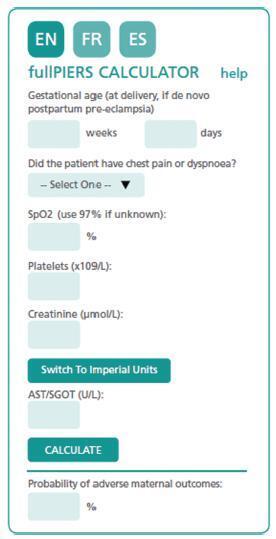
The authors review hypertensive disease during pregnancy with an academic and practical view, and using the best evidence available. This disease, which is the most important clinical disease in Brazilian pregnant women, may have its incidence reduced with prevention through the use of calcium and aspirin in pregnant women at risk. Previously, it was a disease that presented with hypertension with proteinuria, but it has now been classified with new clinical parameters besides proteinuria. Morbidity and mortality should be reduced in a continental country such as Brazil using protocols for the early treatment of complications by calculating severe outcomes in preeclampsia. The early treatment of acute hypertension, use of magnesium sulfate and early hospitalization in cases of preeclampsia are concepts to pursue the reduction of our pregnant women’s mortality.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):195-198
04-01-2017
A pregnancy complicated by typical hemolytic uremic syndrome (HUS) and hemolysis, elevated liver enzymes, low platelets (HELLP) syndrome is reported. At 20 weeks of gestation, a case of HUS was diagnosed, with Shiga toxin-producing Escherichia coli identified. Plasmapheresis allowed continuation of the pregnancy for 5 weeks. Superimposed preeclampsia and HELLP syndrome were diagnosed after the establishment of nephrotic range proteinuria, hypertension and recurrence of hemolysis. This is a singular case, as it demonstrates that HELLP syndrome can superimpose upon HUS, a fact that can impact future research on reproductive immunology. It also reminds clinicians that the overlapping of clinical and laboratory findings in HELLP syndrome makes the diagnosis of other thrombotic microangiopathies during pregnancy a clinical challenge.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(8):406-412
10-16-2008
DOI 10.1590/S0100-72032008000800006
PURPOSE: to evaluate the significance of schizocytes presence in peripheral blood smear of pregnant women with pre-eclampsia, identifying and correlating them with other markers of hemolysis and of the disease severity. METHODS: Seventh six glass slides of peripheral blood smear of pregnant women with pre-eclampsia have been evaluated. After the smear, the slides have been stained with Leishman's dye and stored till they were examined with a Leica, model DLMB microscope, provided with the Qwin Lite 2.5 software that made it possible to record the images of selected fields in CD-ROM. Ten fields with approximately 100 erythrocytes were counted in each glass slide. Schizocytes (irregular fragment or helmet-shaped, bite-shaped or triangular) were considered as present, when their percentage was equal or higher than 0.2%, their presence being correlated with other hemolysis markers (hemoglobin, total bilirubin, lactic desidrogenasis and reticulocytes), pre-eclampsia markers (proteinuria and platelet number). The Statistical Package in Social Science for Windows (SPSS), 10.0 version has been used for statistical analysis, at p<0.05. RESULTS: schizocytes have been present in 31.6% of the pregnant women with pre-eclampsia. In most (75%) of the blood smears there have been three or four schizocytes. There has been no correlation between schizocyte presence and any other hemolysis marker, any pre-eclampsia marker or disease severity. CONCLUSIONS: schizocytes have been identified in a small number and in less than a third of the pregnant women with pre-eclampsia. There has been no correlation with other hemolysis marker parameters or with the disease severity. This way, the presence of schizocytes is not a marker of the clinical evolution of pre-eclampsia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(2):80-86
06-03-2008
DOI 10.1590/S0100-72032008000200006
PURPOSE: to describe the clinical and laboratorial profile of HELLP syndrome patients admitted at an Obstetric Intensive Care Unit (ICU) and included in a randomized clinical trial to evaluate the efficacy of dexamethasone in this clinical setting. METHODS: the present study is a secondary analysis of a randomized clinical trial design to evaluate the efficacy of dexamethasone in patients with HELLP syndrome. This sample of patients was composed of patients in the puerperium, with the diagnosis of HELLP syndrome (diagnosis made before or after delivery) who were not chronic corticosteroid users and not carriers of any chronic disease which could modify HELLP syndrome's laboratorial parameters. Patients who were too critical or whose condition did not allow them to consent to participate were not included. Data were extracted from the records used in the randomized clinical trial. Age, parity, gestational age at admission and delivery, time of diagnosis (before or after delivery), HELLP syndrome classification (partial or complete), arterial blood pressure, and diuresis at admission were considered for analysis. Among laboratorial findings, hemoglobin, platelet count, liver enzymes, LDH, and serum bilirubin were analyzed. Complications presented by the patients were also analyzed as well as need of blood transfusions and duration of hospitalization. Analysis was made by the Epi-Info 3.3.2 program. RESULTS: one hundred and five patients were analyzed. Age varied from 14 to 49 years (means of 26.7). Regarding parity, 56 patients (53.8%) were primiparas. Analyzing the timing of the diagnosis, 47 patients (45.2%) had the diagnosis before delivery. The mean gestational age in these patients was 32.4 weeks. Hemorrhagic manifestations were observed in 36 patients (34.3%), oliguria was present in 49 patients (46.7%) and criteria for acute renal failure were seen in 21 (20%) of the cases. Hemotransfusions were necessary in 35 (33.3%) patients. Seven patients (6.7%) had pulmonary edema and four patients died, corresponding to 3.8% of the cases. The mean time from diagnosis of HELLP syndrome to discharge or death was 10.3 days, varying from 1 to 33 days. CONCLUSIONS: HELLP syndrome is an ominous diagnosis, which implicates in elevated maternal morbimortality. Among complications, oliguria and hemorrhagic manifestations were the most common findings and hemotransfusions were frequently required. Lethality reached 3.8%.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(3):165-167
04-10-1998
DOI 10.1590/S0100-72031998000300008
HELLP syndrome is a severe complication of preeclampsia that increases maternal and perinatal morbidity and mortality. Two cases of recurrent HELLP syndrome are described, maternal death occurring in one of the cases. This study is a warning about the increased risk of HELLP syndrome in the next pregnancy.