Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(1):19-25
To explore the experiences of women with obesity regarding self-care and the care provided by their families and health team after childbirth.
A clinical qualitative study performed at the Postnatal Outpatient Clinic of Hospital da Mulher, Universidade Estadual de Campinas, Brazil. The sample was selected using the saturation criteria, with 16 women with obesity up to 6 months after childbirth.
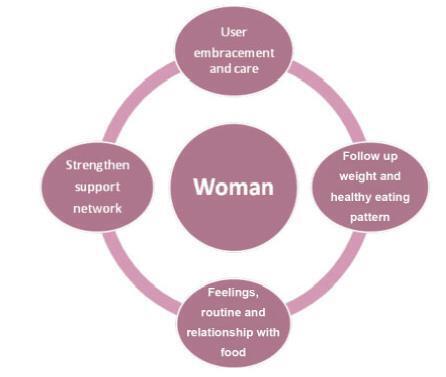
The analysis comprised three categories: 1) postnatal self-care; 2) family support for woman after childbirth; and 3) postnatal health care service for women with obesity.
Women with obesity need support from the health team and from their families after childbirth, when they are overwhelmed by the exhausting care for the newborn. The present study reveals how important it is for health care professionals to broaden their perception and care provided after childbirth for women with obesity so they may experience an improvement in their quality of health and of life.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(9):234-239
DOI 10.1590/S0100-72032011000900003
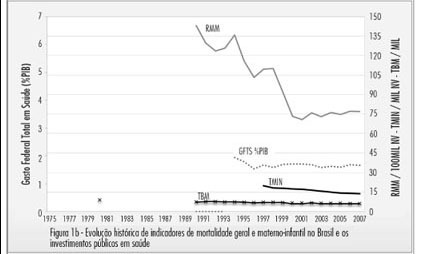
PURPOSE: To analyze comparatively the conditions of birth in Portugal and Brazil from 1975 to 2007. METHODS: Indicators of maternal and child health: rates of maternal death and neonatal mortality, cesarean rate and public spending on health were retrospectively collected from electronic databases of health information from the Unified Health System (DATASUS) and the National Institute of Statistics of Portugal (INE), among others. Their values were descriptively analyzed in terms of trends and the temporal sanitary scenarios were presented and discussed, comparing, when possible, the information from the two countries. RESULTS: Births in Portugal were characterized by lower maternal mortality (12.2x76.2/100.000) and neonatal mortality (2.2x14.6/1000), compared to Brazil, considering the average of the years from 2004 to 2007. The history of the conquest of maternal and child indicators of excellence in Portugal involved a phase that paralleled the significant socio-economic improvements and the increasing contribution of public health, followed by another from the 1990s, involving better equipped health care units. In Brazil, rates of maternal and neonatal mortality are declining, but satisfactory values have not yet been achieved. The historical difference in the amount of social spending on health, both in current and historical values, was a crucial difference between countries. Despite the disparities in maternal and neonatal outcomes, cesarean section rates were equally ascendant (34.5% in Portugal and 45.5% in Brazil), considering the average for the period from 2004 to 2007. CONCLUSION: The indicators of maternal and neonatal death in Portugal and Brazil have aligned themselves to social, economic and contributions of public investments in health. The increasing rates of caesarean section do not explain the discrepancies in maternal and neonatal outcome between countries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(9):258-263
DOI 10.1590/S0100-72032011000900007
PURPOSE: To evaluate the coverage of Pap smear cytology at Basic Family Health Units (BFHU) and to describe the characteristics of non-performance of this test in the last three years. METHODS: A cross-sectional study was conducted in Rio Grande (RS), Brazil, in areas covered by the Family Health Teams Family (FHT). The interviews were conducted by students participating in the Health-PET, at women’s home. Crude analysis was performed using SPSS software to calculate prevalence ratio, 95% confidence intervals and p value. Multivariate analysis was performed by Poisson regression using Stata 9.0 software, which were included the variables with p value of up to 0.20 in the crude analysis. At the first level, the variables were age, having a partner, and literacy. At the second level, the variables were number of visits and offer of a Pap smear. RESULTS: The prevalence of Pap cytology performed 36 months ago or less was 66.3%. In adjusted analysis, women aged 19 years or less (p<0.001), without a partner (p<0.001), illiterate (p= 0.01), who had never consulted at the basic unit (p=0.02) and who had not been offered the examination during the visit (p=0.006), were more likely not to have had a cytopathology exam in the last 36 months. CONCLUSION: The local health proved to be ineffective and inequitable. Ineffective because it covers fewer women than indicated by the World Health Organization and uneven because access to this test varied according to some characteristics of the users.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):563-569
DOI 10.1590/S0100-72032010001100008
PURPOSE: to evaluate the evolution of adequacy of the care process among pregnant users of the Brazilian Single Health System (SUS, acronym in Portuguese) and to consolidate a methodology for monitoring the prenatal care. METHODS: this is a multiple time series study with auditing of prenatal cards of pregnant women who were attended for prenatal care in a city of the Brazilian Southeast (Juiz de Fora, Minas Gerais) in the initial semesters of 2002 and 2004 (370 and 1,200 cards, respectively) and gave birth using SUS services in term pregnancies (p < 0.05). A three complementary level sequence was respected: utilization of prenatal care (beginning and number of visits) at level 1; utilization of prenatal care and obligatory clinical-obstetric procedures during prenatal visits (assessment of blood pressure (BP), weight, uterine fundal height (FH), gestational age (GA), fetal heart rate (FHR) and fetal presentation) at level 2; and utilization of prenatal care, obligatory clinical-obstetric procedures and basic laboratory tests, according to the Humanization Program of Prenatal Care and Birth (PHPN, acronym in Portuguese) (ABO/Rh, hemoglobin/hematocrit (Hb/Htc), VDRL, glycemia and urinalisys) at level 3. RESULTS: it was confirmed the high prenatal care coverage (99%), the increased mean number of visits per pregnant woman (6.4 versus 7.2%) and the decreased gestational age at the time of the first visit (17.4 versus 15.7 weeks). The proper registration of procedures and exams (exceptions: fetal presentation and blood typing) has significantly increased: BP (77.8 versus 83.9%); weight (75.4 versus 83.5%); FH (72.7 versus 81.3%); GA (58.1 versus 71.5%); FHR (79.5 versus 86.7%); Hb/Htc (14.9 versus 29%), VDRL (11.1 versus 20.7%), glycemia (16.5 versus 29%) and urinalisys (13.8 versus 29.8%). As a result, there was significant (p < 0.001) improvement of the adequacy between 2002 and 2004: 27.6 versus 44.8% (level 1); 7.8 versus 15.4% (level 2); 1.1 versus 4.5% (level 3). This trend was also noted in care provided by the majority of the municipal services/teams. CONCLUSIONS: the persistence of low adequacy, despite good coverage and PHPN implementation, confirmed the need to increase health managers, professionals and users' compliance with the rules and routines of care, including the institutionalization of a monitoring program of prenatal care.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(8):402-407
DOI 10.1590/S0100-72032007000800004
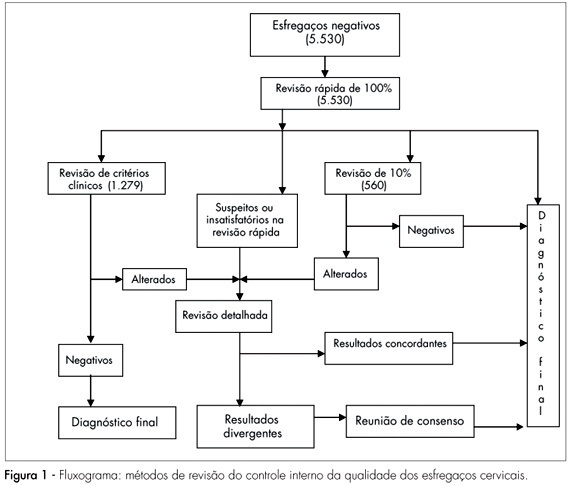
PURPOSE: to evaluate the efficiency of the 100% rapid rescreening in the detection of false-negative results and to verify whether the results vary according to the adequacy of the sample and the woman’s age group. METHODS: to evaluate the efficiency of the rapid rescreening, the 5,530 smears classified as negative by the routine screening, after being submitted to the rapid rescreening of 100%, were compared with the rescreening of the smears on the basis of clinical criteria and 10% random rescreening. For statistical analysis, the variables were evaluated descriptively and the c² test and the Cochran-Armitage test were applied to compare results. RESULTS: of the 141 smears identified as suspicious according to the rapid rescreening method, 84 (59.6%) cases were confirmed in the final diagnosis, of which 36 (25.5%) were classified as atypical squamous cells of undetermined significance, five (3.5%) as atypical squamous cells that cannot exclude high-grade squamous intraepithelial lesion, 34 (24.1%) as low-grade squamous intraepithelial lesion, six (4.3%) as high-grade squamous intraepithelial lesion, and three (2.1%) as atypical glandular cells. Of the 84 suspect smears confirmed in the final diagnosis, 62 (73.8%) smears were classified as adequate and 22 (26.2%) as adequate but with some limitation, but no significant difference was observed with the woman’s age. CONCLUSIONS: the results of this study show that rapid rescreening is an efficient option for internal quality control for the detection of false-negative cervical smear results. In addition, it should be noted that rapid rescreening performed better when the sample was classified as adequate for analysis; however, it did not vary according to the woman’s age group.