Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):456-464
09-01-2016
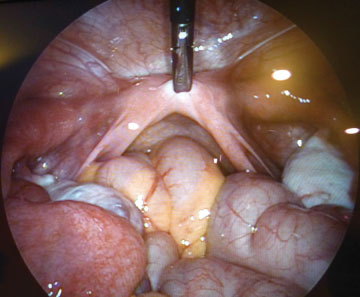
To evaluate the anatomic and functional results of a laparoscopic modified Vecchietti technique for the creation of a neovagina in patients with congenital vaginal aplasia.
Retrospective study of nine patients with congenital vaginal aplasia submitted to the laparoscopic Vecchietti procedure, in our department, between 2006 and 2013. The anatomical results were evaluated by assessing the length, width and epithelialization of the neovagina at the postoperative visits. The functional outcome was evaluated using the Rosen Female Sexual Function Index (FSFI) questionnaire and comparing the patients' results to those of a control group of 20 healthy women. The statistical analysis was performed using SPSS Statistics version 19.0 (IBM, Armonk, NY, USA), Student t-test, Mann-Whitney U test and Fisher exact test.
The condition underlying the vaginal aplasia was Mayer-Rokitansky-KüsterHauser syndrome in eight cases, and androgen insensitivity syndrome in one case. The average preoperative vaginal length was 2.9 cm. At surgery, the mean age of the patients was 22.2 years. The surgery was performed successfully in all patients and no intra or postoperative complications were recorded. At the first postoperative visit (6 to 8 weeks after surgery), the mean vaginal length was 8.1 cm. In all cases, the neovagina was epithelialized and had an appropriate width. The mean FSFI total and single domain scores did not differ significantly from those of the control group: 27.5 vs. 30.6 ( total); 4.0 vs. 4.2 (desire); 4.4 vs. 5.2 (arousal); 5.2 vs. 5.3 (lubrication); 4.2 vs. 5.0 ( orgasm); 5.3 vs. 5.5 (satisfaction) and 4.4 vs. 5.4 ( comfort ).
This modified laparoscopic Vecchietti technique is a simple, safe and effective procedure, which allows patients with congenital vaginal aplasia to have a satisfactory sexual activity, comparable to that of normal controls.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(4):225-228
10-13-2000
DOI 10.1590/S0100-72032000000400006
Purpose: to analyze the frequency of glove perforation during gynecologic surgeries. Methods: a prospective study of 454 gloves used in 65 surgeries by the water pressure method. Results: of a total of 454 gloves, 54 (11.9%) had perforations. Comparison with the control group showed p<0.05 (chi² test), 1 (1.7%) perforation in 60 gloves tested. Of the total of gloves used in 65 surgeries, 29 (44.6%) had perforations, 44 (81%) had one perforation and 10 (19%) had more than one perforation. The two most common sites of perforations were the index finger, 20 (29.5%) and the thumb, 14 (25.9%). Perforation was predominant in the left hand (72.1%). The surgeons were the members of the team with the greatest number of glove perforations. Total hysterectomy was the most frequent surgery in which glove perforations occurred (50% of the cases). Conclusion: the glove perforations occurred with relatively high frequency during gynecologic surgeries. The index finger of the left hand proved to be the most affected region. Among the members of the team, the highest percentage of glove perforations occurred in those of the surgeons. Total hysterectomy had the highest perforation rate.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(3):169-176
09-08-2003
DOI 10.1590/S0100-72032003000300005
PURPOSE: to compare intra- and postoperative results of vaginal hysterectomy with those of abdominal hysterectomy in women without genital prolapse or adnexal pathology. METHODS: a randomized, open clinical trial was conducted, involving 35 patients without genital prolapse scheduled for total hysterectomy due to benign disease, at IMIP, Recife, Brazil. These patients were randomly assigned to vaginal hysterectomy (19 patients) or abdominal hysterectomy (16 patients). Main outcome measures included estimated blood loss, rate of blood transfusion, duration of surgery, postoperative pain (intensity and analgesic requirement), time in hospital, postoperative complications, recovery time and patient satisfaction. Statistical analysis was performed using chi2, exact Fisher and Mann-Whitney tests at a 5% level of significance. RESULTS: estimated blood losses were significantly lower in vaginal hysterectomy (median of 520 mL) than in abdominal hysterectomy (median 902 mL). There was no blood transfusion among patients of the vaginal hysterectomy group, in contrast to 19% of the abdominal hysterectomy group. Duration of surgery was similar (median of 120 min in both groups). Postoperative pain, as measured by visual analog scale and analgesic requirement, was lower for vaginal hysterectomy than for abdominal hysterectomy. There was no statistically significant difference regarding frequency of postoperative complications. There was one case of infection in each group and one case of thrombosis in the vaginal hysterectomy group. Postoperative hospital stay was shorter in the vaginal group. Recovery time was significantly shorter in the vaginal group (median of 35 days) versus the abdominal group (median 40 days). Overall patient satisfaction with the operation was similar in the two groups. CONCLUSIONS: patients without genital prolapse submitted to vaginal hysterectomy for treatment of benign diseases had some advantages in relation to those submitted to abdominal hysterectomy: lower intraoperative blood loss, lower postoperative pain and faster recovery time. Vaginal hysterectomy may replace abdominal hysterectomy in most patients who require hysterectomy.