Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(7):425-431
08-15-2019
To evaluate the relationship between vitamin D receptor (VDR) gene polymorphism (FokI [rs10735810]) and serum vitamin D concentration in gestational diabetes mellitus (GDM).
A prospective case-control study that recruited healthy pregnant women (control group) (n = 78) and women with GDM (GDM group) (n = 79), with no other comorbidities. Peripheral blood samples were collected in the 3rd trimester of gestation, and all of the pregnant women were followed-up until the end of the pregnancy and the postpartum period. Serum vitamin D concentrations were measured by high-performance liquid chromatography (HPLC). For genomic polymorphism analysis, the genomic DNA was extracted by the dodecyltrimethylammonium bromide/ cetyltrimethylammonium bromide (DTAB/CTAB) method, and genotyping was performed by the polymerase chain reaction - restriction fragment length polymorphism (PCR-RFLP) technique, using the restriction enzyme FokI. The Student-t, Mann- Whitney, chi-squared, and Fischer exact tests were used for the analysis of the results.
There was no significant difference between the pregnant women in the control and GDM groups regarding serumvitamin D levels (17.60 ± 8.89 ng/mL versus 23.60 ± 10.68 ng/mL; p = 0.1). Also, no significant difference was detected between the FokI genotypic frequency when the 2 groups were compared with each other (p = 0.41).
There was no association between the FokI polymorphism and the development of GDM, nor was there any change in serum vitamin D levels in patients with GDM.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):298-305
06-27-2019
Gestational diabetes mellitus (GDM) is associated with a higher risk of perinatal morbidity and mortality, and its main complication is the occurrence of large for gestational age (LGA) newborns. The present study aims to characterize pregnant women with GDM and to identify factors associated with the occurrence of LGA newborns in this population.
A cross-sectional study was performed based on medical records of women whose prenatal care and delivery were performed at the Maternal and Child Unit of the HospitalUniversitário of theUniversidade Federal doMaranhão, state of Maranhão, Brazil.A total of 116 pregnant women diagnosed with GDMwere included according to the criteria of the International Association of Diabetes and Pregnancy Study Groups (IADPSG).
The variables associated with LGA newborns after multivariate analysis were: obesity prior to pregnancy (OR = 11.6; 95% CI: 1.40-95.9), previous macrosomia (OR = 34.7; 95% CI: 4.08-295.3), high blood glucose levels in the 3rd trimester (OR = 2,67; 95% CI: 1.01-7.12) and combined change in the oral glucose tolerance test (OGTT) (fasting + postdextrose) (OR = 3.53;95%CI:1.25-14.2) = 1.17-10.6).Otherwise, insufficientweight gain during pregnancy reduced the risk for LGA newborns (OR = 0.04; 95% CI: 0.01-0.32).
Obesity prior to pregnancy, previous macrosomia, high blood glucose levels in the 3rd trimester, and combined change in the OGTT were independent predictive factors for LGA newborns in pregnant women with GDM.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):180-187
04-01-2018
To assess the effectiveness of metformin in the incidence of gestational diabetes mellitus (GDM) in obese pregnant women attending a public maternity hospital in Joinville, Santa Catarina, Brazil.
Randomized clinical trial including obese pregnant women with a body mass index (BMI) ≥ 30 kg/m2, divided into two groups (control and metformin). Both groups received guidance regarding diet and physical exercise. The participants were assessed at two moments, the first at enrollment (gestational age ≤ 20) and the second at gestational weeks 24-28. The outcomes assessed were BMI and gestational diabetes mellitus (GDM) diagnosis. The data distribution was assessed with the Friedman test. For all the analytical models, the p-values were considered significant when lower than 0.05. The absolute risk reduction was also estimated.
Overall, 164 pregnant women were assessed and further divided into 82 participants per group. No significant difference was observed in BMI variation between the control and metformin groups (0.9 ± 1.2 versus 1.0 ± 0.9, respectively, p = 0.63). Gestational diabetes mellitus was diagnosed in 15.9% (n = 13) of the patients allocated to the metformin group and 19.5% (n = 16) of those in the control group (p = 0.683). The absolute risk reduction was 3.6 (95% confidence interval 8.0- 15.32) in the group treated with metformin, which was not significant.
Metformin was not effective in reducing BMI and preventing GDM in obese pregnant women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(6):287-292
06-01-2016
betatrophin has been reported to boost β cell expansion in insulin resistant states. Pregnancy is a well-recognized physiological state of insulin resistance. Betatrophin levels in pregnant women and their relationships with metabolic variables remain to be elucidated.
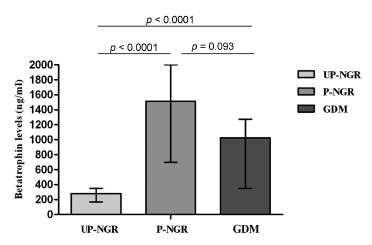
A total of 49 pregnant women and 31 age-matched unpregnant women with normal glucose regulation (UP-NGR) were included. Among these subjects, according to results from 75 g oral glucose tolerance test (OGTT), 22 women were diagnosed as having gestational diabetes mellitus ( GDM ).
Our study found that pregnant women, regardless of their glucose regulation status, had remarkably higher triglycerides (TG), total cholesterol (TC), fasting insulin (FINS), homeostasis model assessment of insulin resistance (HOMA-IR) and homeostasis model assessment of β-cell function (HOMA-β). However, GDM patients had much lower HOMA-β compared with those of pregnant women with normal glucose regulation (P-NGR). Participants of the P-NGR group had almost 4 times higher levels of betatrophin than those of the UP-NGR group. Although betatrophin levels were lower in the GDM group than those of the P-NGR group, the difference did not reach statistical significance. Spearman correlation analysis showed that betatrophin levels were positively and significantly associated with total cholesterol, triglycerides, highdensity lipoprotein cholesterol (HDL-c), FINS and HOMA-β. However, adjustments of TC, TG and HDL-c eliminated the association between HOMA-β and betatrophin.
Pregnant women have significantly higher betatrophin levels in comparison to unpregnant women. Betatrophin levels are positively and significantly associated with β cell function and lipid levels. Furthermore, lipids may contribute to