Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo30
To evaluate the mode of delivery according to Robson classification (RC) and the perinatal outcomes in fetal growth restriction (FGR) and small for gestational age (SGA) fetuses.
Retrospective cohort study by analyzing medical records of singleton pregnancies from two consecutive years (2018 and 2019). FGR was defined according to Delphi Consensus. The Robson groups were divided into two intervals (1–5.1 and 5.2–10).
Total of 852 cases were included: FGR (n = 85), SGA (n = 20) and control (n=747). FGR showed higher percentages of newborns < 1,500 grams (p<0.001) and higher overall cesarean section (CS) rates (p<0.001). FGR had the highest rates of neonatal resuscitation and neonatal intensive care unit admission (p<0.001). SGA and control presented higher percentage of patients classified in 1 - 5.1 RC groups, while FGR had higher percentage in 5.2 - 10 RC groups (p<0.001). FGR, SGA and control did not differ in the mode of delivery in the 1-5.1 RC groups as all groups showed a higher percentage of vaginal deliveries (p=0.476).
Fetuses with FGR had higher CS rates and worse perinatal outcomes than SGA and control fetuses. Most FGR fetuses were delivered by cesarean section and were allocated in 5.2 to 10 RC groups, while most SGA and control fetuses were allocated in 1 to 5.1 RC groups. Vaginal delivery occurred in nearly 60% of FGR allocated in 1-5.1 RC groups without a significant increase in perinatal morbidity. Therefore, the vaginal route should be considered in FGR fetuses.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(1):9-13
To evaluate the prevalence of hypertrophic cardiomyopathy (HCM) in fetuses of pregnant women with gestational diabetes mellitus (GDM) in the beginning of the treatment.
A cross-sectional study was performed between July 1, 2013, and Decem-ber 20, 2013, in a public maternity clinic in southern Brazil. The subjects were 63 fetuses of mothers with gestational diabetes, with a single pregnancy and no other associated pathologies. We diagnosed HCM through a fetal echocardiography before treatment and evaluated the maternal and fetal characteristics.
The average age of the pregnant women was 32.32 (±6.2) years, and the average gestational age at the time of the evaluation was 30.59 (±2.27) weeks. The interventricular septum thickness showed a standard deviation of more than two in 50.8% of the fetuses (95% confidence interval [95%CI]: 38.1-63.5%). The left ventricular wall thickness showed a standard deviation of more than 2 in 13 (20.6%) fetuses (95%CI: 11.1-30.2%). The HCM was confirmed in 54% of the fetuses (95%CI: 41.3-65.1%). The fetal abdominal circumference was normal in 46 (73%) fetuses, and 50% of these fetuses had HCM.
The prevalence of hypertrophic cardiomyopathy in fetuses of pregnant women with GDM before treatment was of 54% (95%CI: 41.3-65.1%).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):436-442
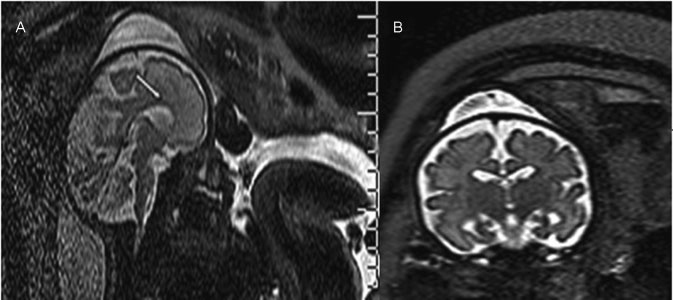
Ventriculomegaly (VM) is one the most frequent anomalies detected on prenatal ultrasound. Magnetic resonance imaging (MRI) may enhance diagnostic accuracy and prediction of developmental outcome in newborns.
The aim of this study was to assess the correlation between ultrasound and MRI in fetuses with isolated mild and moderate VM. The secondary aim was to report the neurodevelopmental outcome at 4 years of age.
Fetuses with a prenatal ultrasound (brain scan) diagnosis of VM were identified over a 4-year period. Ventriculomegaly was defined as an atrial width of 10- 15 mm that was further divided as mild (10.1-12.0 mm) and moderate (12.1-15.0 mm). Fetuses with VM underwent antenatal as well as postnatal follow-ups by brain scan and MRI. Neurodevelopmental outcome was performed using the Griffiths Mental Development Scales and conducted, where indicated, until 4 years into the postnatal period.
Sixty-two fetuses were identified. Ventriculomegaly was bilateral in 58% of cases. A stable dilatation was seen in 45% of cases, progression was seen in 13%, and regression of VM was seen in 4.5% respectively. Fetal MRI was performed in 54 fetuses and was concordant with brain scan findings in 85% of cases. Abnormal neurodevelopmental outcomes were seen in 9.6% of cases.
Fetuses in whom a progression of VM is seen are at a higher risk of developing an abnormal neurodevelopmental outcome. Although brain scan and MRI are substantially in agreement in defining the grade of ventricular dilatation, a low correlation was seen in the evaluation of VM associated with central nervous system (CNS) or non-CNS abnormalities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):428-435
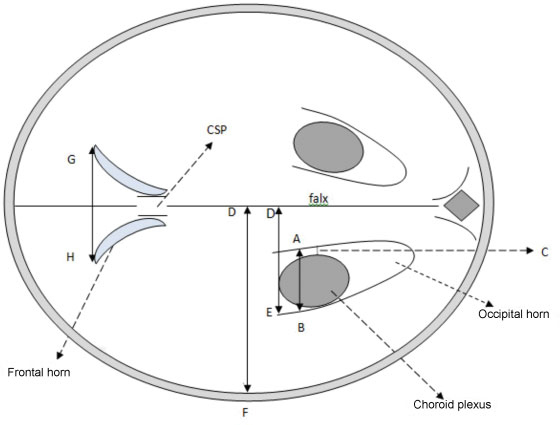
This study was done to evaluate the normal fetal cerebral lateral ventricle dimensions with transabdominal ultrasonography. The atrial width (AW), ventricle-tochoroid measurement (V-C), ventricle-to-hemisphere ratio (VHR), and combined anterior horn measurement (CAHM) were taken.
This was a cross-sectional study involving 400 normal singleton pregnant subjects whose gestational ages were between 14 and 40 weeks. Transabdominal sonography was performed to obtain the values of the fetal cerebral lateral ventricle (FCLV) parameters. Data were reported as mean standard deviation (SD) for continuous variables. The degrees of correlation between FCLV parameters and the estimated gestational age (EGA) were obtained using Pearson's correlation. Regression equations were used to generate the reference limits for the FCLV measurements.
The values of AW, V-C measurements and CAHM increased with advancing gestation. The mean values of the AW, V-C and CAHM from 14 to 40 weeks increased from 6.60 0.94 mm to 9.75 0.07 mm (R2 = 0.114), 0.80 0.00 mm to 1.90 0.14 mm (R2= 0.266), and 6.95 0.06 mm to 23.07 4.02 mm (R2= 0.692) respectively, while the mean VHR decreased from 61.20 1.60% to 42.84 2.91% (R2 = 0.706) over the same period.
The AW, V-C, and CAHM increase, while VHR decreases with advancing gestation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):120-126
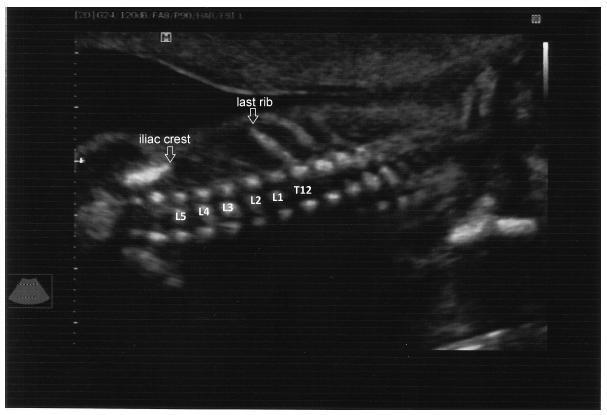
To evaluate the precision of both two- and three-dimensional ultrasonography in determining vertebral lesion level (the first open vertebra) in patients with spina bifida.
This was a prospective longitudinal study comprising of fetuses with open spina bifida who were treated in the fetal medicine division of the department of obstetrics of Hospital das Clínicas of the Universidade de São Paulo between 2004 and 2013. Vertebral lesion level was established by using both two- and three-dimensional ultrasonography in 50 fetuses (two examiners in each method). The lesion level in the neonatal period was established by radiological assessment of the spine. All pregnancies were followed in our hospital prenatally, and delivery was scheduled to allow immediate postnatal surgical correction.
Two-dimensional sonography precisely estimated the spina bifida level in 53% of the cases. The estimate error was within one vertebra in 80% of the cases, in up to two vertebrae in 89%, and in up to three vertebrae in 100%, showing a good interobserver agreement. Three-dimensional ultrasonography precisely estimated the lesion level in 50% of the cases. The estimate error was within one vertebra in 82% of the cases, in up to two vertebrae in 90%, and in up to three vertebrae in 100%, also showing good interobserver agreement. Whenever an estimate error was observed, both two- and three-dimensional ultrasonography scans tended to underestimate the true lesion level (55.3% and 62% of the cases, respectively).
No relevant difference in diagnostic performance was observed between the two- and three-dimensional ultrasonography. The use of three-dimensional ultrasonography showed no additional benefit in diagnosing the lesion level in the fetuses with spina bifida. Errors in both methods showed a tendency to underestimate lesion level.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(3):133-139
DOI 10.1590/SO100-720320150005132
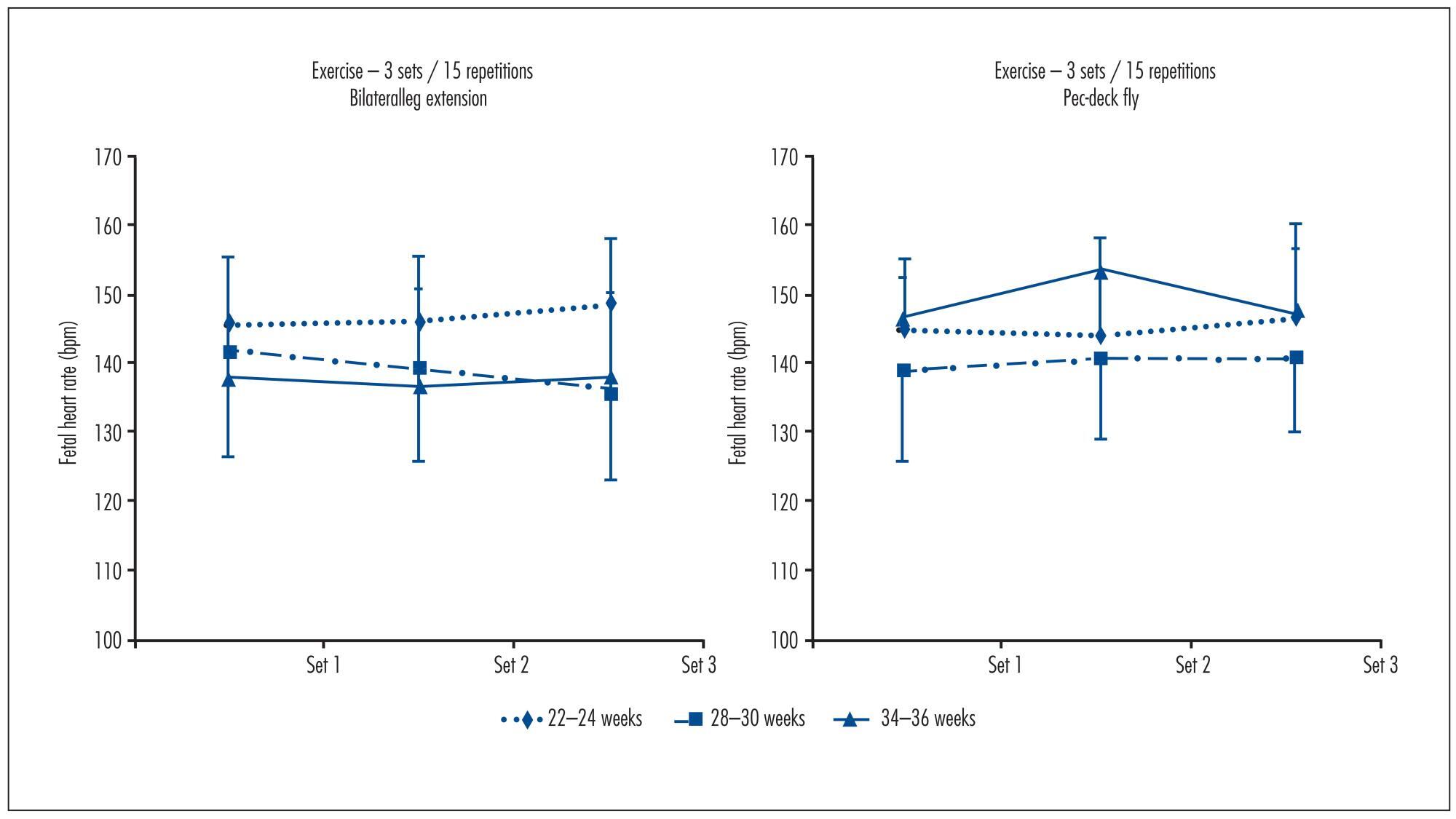
To determine fetal heart rate (FHR) responses to maternal resistance exercise for the upper and lower body at two different volumes, and after 25 minutes post-exercise.
Ten pregnant women (22-24 weeks gestation, 25.2±4.4 years of age, 69.8±9.5 kg, 161.6±5.2 cm tall) performed, at 22-24, 28-32 and 34-36 weeks, the following experimental sessions: Session 1 was a familiarization with the equipment and the determination of one estimated maximum repetition. For sessions 2, 3, 4 and 5,FHR was determined during the execution of resistance exercise on bilateral leg extension and pec-deck fly machines, with 1 and 3 sets of 15 repetitions; 50% of the weight load and an estimated repetition maximum. FHR was assessed with a portable digital cardiotocograph. Results were analyzed using Student's t test, ANOVA with repeated measures and Bonferroni (α=0.05; SPSS 17.0).
FHR showed no significant differences between the exercises at 22-24 weeks (bilateral leg extension=143.8±9.4 bpm, pec-deck fly=140.2±10.2 bpm, p=0.34), 28-30 weeks (bilateral leg extension=138.4±12.2 bpm, pec-deck fly=137.6±14.0 bpm, p=0.75) and 34-36 weeks (bilateral leg extension=135.7±5.8 bpm, pec-deck fly=139.7±13.3 bpm, p=0.38), between the volumes(bilateral leg extension at 22-24 weeks: p=0.36, at 28-30 weeks: p=0.19 and at 34-36 weeks: p=0.87; pec-deck fly at 22-24 weeks: p=0.43, at 28-30 weeks: p=0.61 and at 34-36 weeks: p=0.49) and after 25 minutes post-exercise.
Results of this pilot study would suggest that maternal resistance exercise is safe for the fetus.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(2):55-59
DOI 10.1590/S0100-72032013000200003
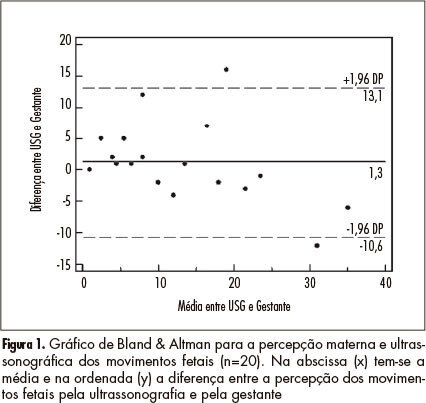
PURPOSE: To determine the agreement between maternal perception of fetal movements and the movements recorded simultaneously by ultrasound in low-risk pregnancies. METHODS: Twenty pregnant women were evaluated with the following inclusion criteria: single pregnancy, alive fetus, maternal age between 18 and 35 years; between 36 and 40 weeks gestation; normal fetal morphology at ultrasound, and absence of maternal comorbidities. The pregnant women were evaluated for 10 minutes, during which cardiotocography was used to record fetal movements triggered with the event marker, with the paper speed set at 3 cm/min. At the same time, fetal movements were observed by ultrasonography. RESULTS: The kappa index for interobserver agreement analysis was 0.62, showing good agreement (95%CI 0.45 - 0.79). The intraclass correlation coefficient was 0.82 (95%CI 0.61 - 0.92). Analysis by the Bland & Altman graph indicated good agreement. A linear regression analysis showed a significant correlation between maternal perception (x) and ultrasound (y) observation (r²=0.71, p<0.001; equation: y=5.31+0.66x). CONCLUSIONS: The agreement between ultrasound and maternal perception of fetal movement is good, allowing the use of fetal movement counting in the assessment of fetal wellbeing.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):310-315
DOI 10.1590/S0100-72032012000700004
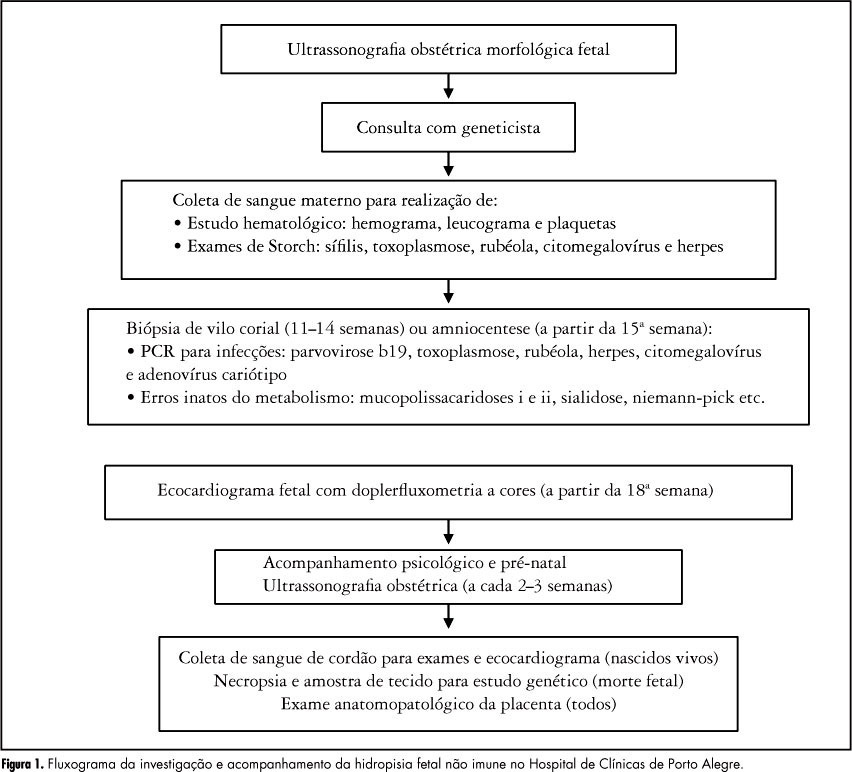
PURPOSE: To identify the etiology of nonimmune hydrops fetalis cases in pregnant women diagnosed and referred for prenatal care. METHODS: Retrospective analysis of cases with nonimmune hydrops fetalis that were monitored between March 1992 and December 2011. Diagnosis was confirmed by the presence of fetal subcutaneous edema (≥5 mm) with effusion in at least one serous cavity using obstetric ultrasound, and etiological investigation was conducted with cytogenetic (karyotype), infectious (syphilis, parvovirus B19, toxoplasmosis, rubella, cytomegalovirus, adenovirus and herpes simplex), hematologic and metabolic (inborn errors) analysis and fetal echocardiography. Twin pregnancies were excluded. Statistical analysis was performed using the χ² test for adhesion (software R 2.11.1). RESULTS: We included 116 patients with nonimmune hydrops fetalis; the etiology was elucidated in 91 cases (78.5%), while 25 cases (21.5%) were classified as idiopathic. Most cases had a chromosomal etiology, for a total of 26 cases (22.4%), followed by lymphatic etiology with 15 cases (12.9% with 11 cases of cystic hygroma), and cardiovascular and infectious etiology with 14 cases each (12.1%). In the remaining cases, the etiology was thoracic in 6.9% (eight cases), malformation syndromes in 4.3% (five cases), extrathoracic tumors in 3.4% (four cases), metabolic in 1.7% (two cases), and hematologic, gastrointestinal and genitourinary in 0.9% (one case each). During the postnatal period, 104 cases were followed up until the 40th day of life, and 12 cases had intrauterine fetal death. The survival rate of these 104 newborns was 23.1% (24 survived). CONCLUSION: An attempt should be made to clarify the etiology of hydrops diagnosed during pregnancy since the condition is associated with a wide spectrum of diseases. It is especially important to determine whether a potentially treatable condition is present and to identify disease at risk for recurrence in future pregnancies for adequate pre-conception counseling.