Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(10):280-285
DOI 10.1590/S0100-72032011001000002
PURPOSE: To analyze the results of assessment of fetal well-being in pregnancies complicated by moderate or severe maternal thrombocytopenia. METHODS: Data from April 2001 to July 2011 of 96 women with a diagnosis of thrombocytopenia in pregnancy were retrospectively analyzed. We analyzed the following tests performed during the antepartum period for fetal assessment: cardiotocography, fetal biophysical profile, amniotic fluid index and umbilical artery Doppler velocimetry. RESULTS: A total of 96 pregnancies with the following diagnoses were analyzed: gestational thrombocytopenia (n=37, 38.5%) hypersplenism (n=32, 33.3%), immune thrombocytopenic purpura (ITP, n=14, 14.6%), secondary immune thrombocytopenia (n=6, 6.3%), bone marrow aplasia (n=3, 3.1%), and others (n=4, 4.1%). Cardiotocography showed normal results in 94% of cases, a fetal biophysical profile with an index of 8 or 10 in 96.9% and an amniotic fluid index >5.0 cm in 89.6%. Doppler umbilical artery velocimetry showed normal results in 96.9% of cases. In the analysis of the major groups of thrombocytopenia, the diagnosis of oligohydramnios was found to be significantly more frequent in the group with ITP (28.6%) compared to the other groups (gestational thrombocytopenia: 5.4% and hypersplenism: 9.4%, p=0.04). CONCLUSIONS: This study indicates that in pregnancies complicated by moderate or severe maternal thrombocytopenia, even though the fetal well-being remains preserved in most cases, fetal surveillance is important in pregnant women with ITP, with emphasis on amniotic fluid volume evaluation due to its association with oligohydramnios.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(8):174-181
DOI 10.1590/S0100-72032011000800002
PURPOSE: To describe the maternal and perinatal outcomes of pregnant women diagnosed with leukemia who were followed up for prenatal care and delivery at a university hospital. METHODS: A retrospective study of the period from 2001 to 2011, which included 16 pregnant women with a diagnosis of leukemia followed by antenatal care specialists in hematological diseases and pregnancy. For acute leukemia diagnosed after the first trimester, the recommendation was to perform chemotherapy despite the current pregnancy. For chronic leukemia, patients who were controlled in hematological terms were maintained without medication during pregnancy, or chemotherapy was introduced after the first trimester. We analyzed the maternal and perinatal outcome. RESULTS: Acute lymphoblastic leukemia (ALL) was diagnosed in five cases (31.3%), acute myeloid leukemia (AML) in two cases (12.5%) and chronic myeloid leukemia (CML) in nine cases (56.3%). Of the cases of acute leukemia, two (28.6%) were diagnosed in the first trimester, two (28.6%) in the second and three (42.9%) in the third. Two patients with ALL diagnosed in the first trimester opted for therapeutic abortion. Four patients with acute leukemia received chemotherapy during pregnancy, with a diagnosis established after the 20th week. In one case of ALL with a late diagnosis (30 weeks), chemotherapy was started after delivery. All pregnant women with acute leukemia developed anemia and thrombocytopenia, and four (57.1%) developed febrile neutropenia. Of nine pregnant women with CML, four were treated with imatinib mesylate when they became pregnant, with treatment being interrupted in the first trimester in three of them and in the second trimester in one. During pregnancy, three patients (33.3%) required no chemotherapy after discontinuation of imatinib, and six (66.7%) were treated with the following drugs: interferon (n=5) and/or hydroxyurea (n=3 ). In the group of pregnant women with CML, anemia occurred in four (44.4%) cases and thrombocytopenia in one (11.1%). The perinatal outcomes of pregnancies complicated by acute leukemia were as follows: mean gestational age at delivery was 32 weeks (standard deviation - SD=4.4) and the mean birth weight was 1476 g (SD=657 g), there were 2 (40.0%) perinatal deaths (a fetal one and a neonatal one). In pregnancies complicated by CML, the mean gestational age at delivery was 37.6 weeks (SD=1.1) and the mean birth weight was 2870 g (SD=516 g). There was no perinatal death and no fetal abnormality was detected. CONCLUSIONS: Maternal and fetal morbidity is high in pregnancies complicated by acute leukemia. Whereas, in pregnancies complicated by CML, the maternal and fetal prognosis appears to be more favorable, with greater ease in management of complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(3):111-117
DOI 10.1590/S0100-72032011000300002
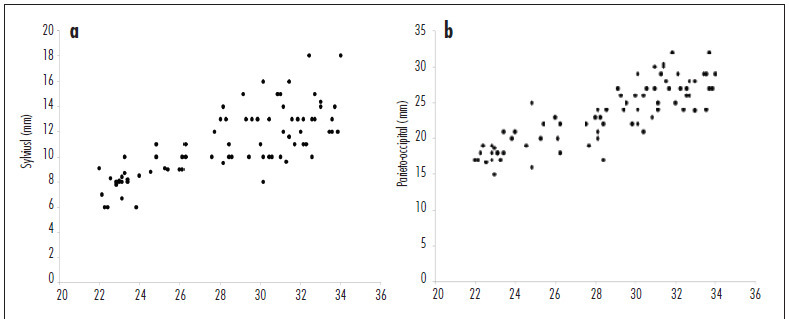
PURPOSE: to assess the distance of the fetal cerebral fissures from the inner edge of the skull by three-dimensional ultrasonography (3DUS). METHODS: this cross-sectional study included 80 women with normal pregnancies between 21st and 34th weeks. The distances between the Sylvian, parieto-occiptal, hippocampus and calcarine fissures and the internal surface of the fetal skull were measured. For the evaluation of the distance of the first three fissures, an axial three-dimensional scan was obtained (at the level of the lateral ventricles). To obtain the calcarine fissure measurement, a coronal scan was used (at the level of the occipital lobes). First degree regressions were performed to assess the correlation between fissure measurements and gestational age, using the determination coefficient (R²) for adjustment. The 5th, 50th and 95th percentiles were calculated for each fissure measurement. Pearson's correlation coefficient (r) was used to assess the correlation between fissure measurements and the biparietal diameter (BPD) and head circumference (HC). RESULTS: all fissure measurements were linearly correlated with gestational age (Sylvian: R²=0.5; parieto-occiptal: R²= 0.7; hippocampus: R²= 0.3 and calcarine: R²= 0.3). Mean fissure measurement ranged from 7.0 to 14.0 mm, 15.9 to 28.7 mm, 15.4 to 25.4 mm and 15.7 to 24.8 mm for the Sylvian, parieto-occiptal, hippocampus and calcarine fissures, respectively. The Sylvian and parieto-occiptal fissure measurements had the highest correlations with the BPD (r=0.8 and 0.7, respectively) and HC (r=0.7 and 0.8, respectively). CONCLUSION: the distance from the fetal cerebral fissures to the inner edge of the skull measured by 3DUS was positively correlated with gestational age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(12):573-578
DOI 10.1590/S0100-72032010001200002
PURPOSE: to establish reference values for the length and area of the fetal corpus callosum between the 20th and 33rd weeks of gestation using three-dimensional ultrasound (3DUS). METHODS: this cross-sectional study involved 70 normal pregnancies with gestational age between 20 and 33 weeks. An Accuvix XQ instrument with a convex volumetric transducer (3 to 5 MHz) was used. To assess the corpus callosum, a transfrontal plane was obtained using the metopic suture as an acoustic window. Length was obtained by measuring the distance between the proximal and distal extremities of the corpus callosum. Area was obtained by manual tracing of the external corpus callosum surface. The means, medians, standard deviations, and maximum and minimum values were calculated for the corpus callosum length and area. Scatter graphs were created to analyze the correlation between corpus callosum length and area and gestational age and biparietal diameter, the quality adjustments was verified according to the determination coefficient (R²). The intraclass correlation coefficient (ICC) was used to assess the intraobserver variability. RESULTS: mean corpus callosum length increased from 21.7 (18.6 - 25.2 mm) to 38.7 mm (32.6 - 43.3 mm) between 20 and 33 weeks of pregnancy, respectively. Mean corpus callosum area increased from 55.2 (41.0 - 80.0 mm²) to 142.2 mm² (114.0 - 160.0 mm²), between 20 to 33 weeks of pregnancy, respectively. There was a strong correlation between corpus callosum length and area and gestational age (R² = 0.7 and 0.7, respectively) and biparietal diameter (R² = 0.7 and 0.6, respectively). Intraobserver variability was appropriate, with an ICC of 0.9 and 0.9 for length and area, respectively. CONCLUSIONS: reference values for corpus callosum length and area were established for fetuses between 20 and 33 weeks gestation. Intraobserver variability was appropriate.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(8):405-411
DOI 10.1590/S0100-72032010000800008
PURPOSE: the aim of this study was to describe perinatal and maternal outcomes of pregnancies complicated by sickle cell disease (SCD), comparing to pregnancies of women with sickle cell trait (SCT). METHODS: this was a retrospective cohort study, covering the period from March 2001 to April 2008, which included all pregnant women with SCD (n=42) followed up at a university hospital in the Southeast region of Brazil. The maternal and perinatal outcomes were compared to those of pregnant women with SCT (n=56) who were followed up at the same service. RESULTS:SCD-SS was diagnosed in 42 (82.4%) pregnant women and SC in 9 (17.6%). Mean (±SD) maternal age was significantly lower in the SCD group (26.0 years) compared to SCT women (28.7±7.1 years; p=0.018). The following maternal complications were more common among women with SCD in comparison to SCT: urinary tract infection (25.5 versus 8.9%; p=0.04), pneumonia (23.5 versus 1.8%; p=0.002), pulmonary hypertension (15.7 versus 0%; p=0.002), and blood transfusion during delivery or postpartum (33.3 versus 5.4%; p=0.001). Adverse perinatal outcome was more frequent in the SCD group compared to the SCT group: prematurity (49 versus 25%, p=0.01); mean gestational age at delivery (35.2 versus 37.9 weeks, p<0.001); fetal distress (56.9 versus 28.6%, p=0.006); birth weight <2,500 g (62.7 versus 17.9%, p<0.001); mean birth weight (2,183 versus 2,923 g, p<0.001), and small for gestational age infants (29.4 versus 10.7%, p=0.029). Two maternal deaths (3.9%) occurred in the group with SCD. CONCLUSION: Pregnant women with SCD are at greater risk for maternal morbidity and for adverse perinatal outcomes than women with SCT.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(7):366-371
DOI 10.1590/S0100-72032008000700008
The application and development of obstetric Dopplervelocimetry provide a basis for the investigation of placental insufficiency and demonstrate the dynamic behavior of fetal circulation during hypoxia. In clinical practice, assessing hemodynamics in three vascular regions involved in pregnancy, namely the uterine, umbilical and middle cerebral arteries, has become routine. Roughly, the cerebral artery expresses the balance between uterine artery oxygen supply and umbilical artery oxygen uptake. Currently, when such balance is unfavorable, the fetal cardiac reserve is investigated by assessing the venous duct. However, determining and interpreting vascular resistance indexes is not an easy task. The starting point is to know the physiopathology of placental insufficiency and fetal circulatory adaptation through which Doppler confirmed its role in the assessment of fetal well-being.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(1):47-54
DOI 10.1590/S0100-72032010000100008
ABSTRACT About 1% of all pregnancies present structural anomalies. During the last three decades, various experimental studies in large animals, associated with the technological advance of diagnostic imaging and fetoscopy equipment, have led to great progress in the knowledge of the pathophysiology of various congenital defects. Such knowledge applied to intrauterine correction of abnormalities has transformed the natural history of several previously fatal diseases, leading to a considerable number of survivors. Fetal intervention, such as open fetal surgery, may be indicated in meningomyelocele or in congenital cystic adenomatoid malformation, and in sacrococcygeal teratoma, which lead to secondary fetal hydropsy. Besides, minimally invasive procedures using fetoscopy may have application in congenital diaphragmatic hernia, in feto-fetal transfusion, in twin pregnancies with an acardiac fetus, in the posterior urethral valve, and in hypoplasia of the cardiac chambers, with good results. Even though open fetal surgery and minimally invasive procedures are still experimental and still need to be fully validated, a correct echographic diagnosis and the patient's referral to tertiary centers providing multidisciplinary fetal care contribute to the survival of fetuses with congenital diseases of usually fatal evolution.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(6):285-292
DOI 10.1590/S0100-72032009000600004
PURPOSE: to investigate the main factors associated with fetal death in the city of Recife, Pernambuco, Brazil. METHODS: an observational, case-control study, including cases attended from June 1st 2004 to 31st March 2005. A number of 116 stillbirth cases and 472 live birth controls, with deliveries assisted at the service, were included. The cases were identified in the record book from the delivery room. The puerperium women were identified by the name and register number at a puerperium infirmary. The controls were selected, using the puerperium infirmary neighborhood criterion, identifying the beds with numbers immediately lower (two patients) and higher (two patients) than the patient's, as far as they had delivered live babies. In case they did not agree to participate in the research, the next beds with numbers consecutively lower or higher were approached. The χ2 association and Fisher's exact tests were used when necessary to test the association between the independent (predictive) and dependent (stillborn) variables, considering 5% as the significance level. To determine the association strength, the estimate of relative risk for case-control cases, Odds Ratio (OR) was used, with 95% as the confidence interval (CI). Logistic regression analysis according to the hierarchy model was done to control confounding factors. RESULTS: the fetal mortality rate corresponded to 24.4 by 1,000 births. After the multivariate analysis, the variables which kept significantly associated with fetal death were: malformation (OR=7.5; CI=3.2-17.4), number of pre-natal appointments lower than six (OR=4.4; CI=2.5-7.5), hemorrhagic syndromes (OR=2.9; CI=1.4-5.7), attendance in another hospital unit along the 24 hours which preceded the patient's admission in the institution (OR=2.9; CI=1.8-4.6), mothers' age over or equal to 35 years old (OR=2.2; CI=1.0-4.9) and schooling lower than eight years (OR=1.6; CI=1.02-2.6). CONCLUSIONS: it was found a high fetal mortality coefficient, the main factors associated with death were: malformation, number of pre-natal appointments lower than six, hemorrhagic syndromes, history of attendance previous to the hospital admission, mothers' age over or equal to 35 and schooling lower than eight years.