-
Original Article
Fetal Echocardiography Indications and Lack of Association between Abnormal Exams and Advanced Maternal Age: A Cross-Sectional Study – Fetal Abnormal Echocardiography
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):805-810
01-11-2020
Summary
Original ArticleFetal Echocardiography Indications and Lack of Association between Abnormal Exams and Advanced Maternal Age: A Cross-Sectional Study – Fetal Abnormal Echocardiography
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):805-810
01-11-2020Views125See moreAbstract
Objective
To analyze the most frequent referrals for fetal echocardiography, including advanced maternal age and its association with abnormal results.
Methods
We included all pregnant women referred to perform fetal echocardiography (gestational age 22-32 weeks) in 2 health centers in Rio de Janeiro, from June 2015 to June 2016. Advanced maternal age was considered when age was > 35 years at the time of delivery). Referral reasons and results were recorded, according to the Brazilian Fetal Cardiology Statement. Crude and adjusted prevalence ratios were calculated (Poisson regression). We considered p < 0.05 as significant.
Results
A total of 1,221 tests were analyzed. Abnormal fetal echocardiography was observed in 14.82% of the cases. The most frequent abnormalities were interventricular septal defect (6.39%), septal hypertrophy (3.35%) and atrioventricular septal defect (1.14%). Routine exams were performed in 559 women, 289 were referred for advanced maternal age and 373 were referred according to the Brazilian FetalCardiology Statement criteria. An obstetric ultrasound suggesting fetal cardiacabnormality, maternal diabetes, increased nuchal translucency, and obstetric ultrasound suggesting a noncardiac abnormality were strongly associated with an abnormal fetal echocardiography. Abnormal results were not more frequent in women with advanced maternal age when compared with the rest of the study group.
Conclusions
It was observed that routine exams and advancedmaternal age referrals were very frequent. Those exams were not associated to fetal echocardiography abnormalities. In this scenario, when the obstetric ultrasound suggests a fetal cardiac
-
Original Article
Prevalence and Association of Congenital Anomalies According to the Maternal Body Mass Index: Cross-Sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):280-290
06-27-2019
Summary
Original ArticlePrevalence and Association of Congenital Anomalies According to the Maternal Body Mass Index: Cross-Sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):280-290
06-27-2019Views167See moreAbstract
Objective
To evaluate and compare the prevalence of structural congenital anomalies (CAs) according to maternal body mass index (BMI).
Methods
The present cross-sectional study involved pregnant women with fetuses diagnosed with structural CAs through morphological ultrasonography between November 2014 and January 2016. The nutritional status of the pregnant women was classified according to the gross value of the body mass index. The pregnant women were categorized into four groups: low weight, adequate weight, overweight, and obesity. Statistical analysis was performed using Stata/SE version 12.0 (Stata Corporation, College Station, TX), with values of p ≤ 0.05 considered statistically significant.
Results
A total of 223 pregnant women had fetuses diagnosed with CAs. The prevalence of structural CAs in pregnant women with lowweight was of 20.18%, of 43.50% in pregnant women with adequate weight, of 22.87% in pregnant women with overweight, and of 13.45% in pregnant women with obesity. The prevalence of central nervous system (CNS) anomalies and of genitourinary systemanomalieswas high for the four groups of pregnant women. A positive association was observed between multiple anomalies in pregnant women with adequate weight (prevalence ratio [PR] = 1.65; p ≤ 0.004) and between anomalies of the lymphatic system in obese pregnant women (PR = 4.04, p ≤ 0.000).
Conclusion
The prevalence of CNS and genitourinary systemanomalies was high in all of the BMI categories. Obese pregnancies were associated with lymphatic system anomalies. Therefore, screening and identification of the risk factors for CAs are important, regardless of the maternal BMI. Our findings reinforce the importance of discussing with pregnant women maternal nutrition and its effect on fetal development and on neonatal outcome.
-
Case Reports
Diagnosis of Atelosteogenesis Type I suggested by Fetal Ultrasonography and Atypical Paternal Phenotype with Mosaicism
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):570-575
09-01-2018
Summary
Case ReportsDiagnosis of Atelosteogenesis Type I suggested by Fetal Ultrasonography and Atypical Paternal Phenotype with Mosaicism
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(9):570-575
09-01-2018Views196Abstract
Atelosteogenesis type I (AOI) is an autosomal dominant skeletal dysplasia caused by mutations in the filamin B (FLNB) gene with classic and well-recognizable clinical findings. However, parents affected with a mild phenotype, probably with somatic mosaicism, can generate offspring with a much more severe phenotype of AOI. In the present report, we describe a female newborn with classic AOI leading to early neonatal death, whose diagnostic was based on prenatal radiological findings and on the physical examination of the father. Since her father had limb deformities and corporal asymmetry, suggesting somatic mosaicism, his biological samples were analyzed through a gene panel for skeletal dysplasias. A missense mutation not previously described in the literature was detected in the FLNB gene, affecting ~ 20% of the evaluated cells and, therefore, confirming the diagnosis ofmosaic AOI in the father. The molecular analysis of the father was crucial to suggest the diagnosis of AOI in the newborn, since she died early and there were no biological samples available.
Key-words atelosteogenesisexome-target sequencingFetal ultrasonographyFLNBskeletal dysplasiasomatic mosaicismSee more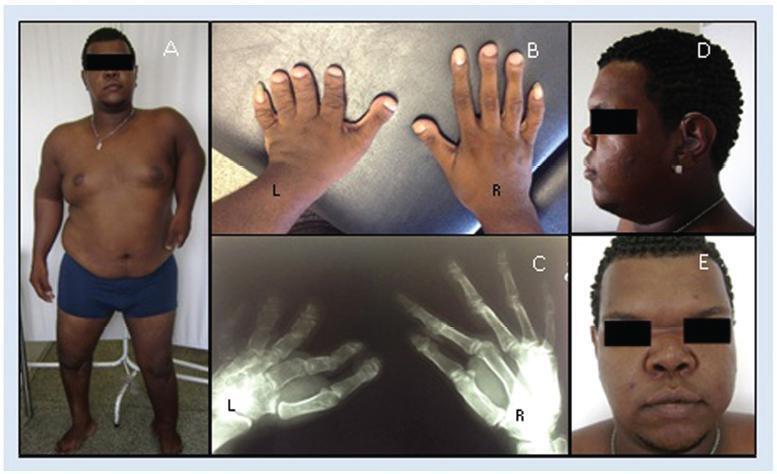
-
Trabalhos Originais
Diagnosis of fetal growth restriction by transverse cerebellar diameter/abdominal circumference ratio
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):535-541
10-14-2004
Summary
Trabalhos OriginaisDiagnosis of fetal growth restriction by transverse cerebellar diameter/abdominal circumference ratio
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):535-541
10-14-2004DOI 10.1590/S0100-72032004000700005
Views90PURPOSE: to evaluate the validity of transverse cerebellar diameter (TCD)/abdominal circumference (AC) ratio in the diagnosis of fetal growth restriction (FGR), determining its best cutoff value and accuracy in symmetric and asymmetric FGR. METHOD: a prospective cross-sectional study, carried out in 250 pregnant women with singleton pregnancies, gestational age between 20 and 42 weeks, with ultrasound confirmation. The TCD measurement was obtained by placing the calipers at the outer margins of the cerebellum, after its localization in the posterior fossa, and slightly rotating the transducer below the plane of the thalami. The abdominal circumference was measured at the on junction of the left portal and umbilical veins. The best TCD/AC cutoff ratio was established by the receiver operator characteristic (ROC) curve. Neonates with TCD/AC ratio greater than the cutoff value were diagnosed as having FGR. We classified as gold standard for FGR the newborn infants who presented birth weight below the 10th percentile. Neonates showing FGR and Rohrer ponderal index between 2.2 and 3 were labeled as symmetric and below 2.2, asymmetric. RESULTS: the cutoff value calculated by the ROC curve for TCD/AC ratio was 16.15. The sensitivity, specificity, accuracy, positive and negative predictive values, and likelihood ratio for positive and negative tests were 77.4, 82.6, 38.7, 96.3, 82, 4.5 and 3.7%, respectively. In the symmetric FGR, sensitivity and specificity were 80.8 and 81.7%, respectively. In the asymmetric FGR, sensitivity and specificity were 60 and 75%, respectively. CONCLUSION: TCD/AC ratio is an effective method in symmetric and asymmetric FGR diagnosis.
Key-words Abdominal circumferenceFetal growth restrictionFetal ultrasonographyTransverse cerebellar diameterSee more -
Trabalhos Originais
Identification of Fetal Gender by Ultrasound at 11th to 14th Weeks of Gestation
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(4):247-251
06-27-2001
Summary
Trabalhos OriginaisIdentification of Fetal Gender by Ultrasound at 11th to 14th Weeks of Gestation
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(4):247-251
06-27-2001DOI 10.1590/S0100-72032001000400008
Views124See morePurpose: to determine the feasibility of early ultrasonographic identification of fetal gender. Methods: a prospective study in a University Department of Obstetrics and Gynecology. A total of 592 women underwent ultrasonography at 11-14 weeks of gestation. Fetal gender was identified according to genital tubercle position (vertical or horizontal) at sagittal plane and confirmed at birth or by karyotype analysis. Results: the overall accuracy of correctly assigning fetal gender was 84%. The success of identification increased with gestational age, being 72%, 85% and 89% at 11, 12 and 13 weeks, respectively. The accuracy of correctly identifying fetal sex significantly changed with operator training, being 83.5% at the beginning and 93.6% at the end of the study. Conclusion: ultrasound determination of fetal gender is feasible, with good accuracy and may be of potential use to avoid invasive testing in family histories of X-linked disorders.


