Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):455-459
DOI 10.1590/SO100-720320150005271
To analyze the obstetrical and neonatal outcomes of pregnancies with small for gestation age fetuses after 35 weeks based on umbilical cord nucleated red blood cells count (NRBC).
NRBC per 100 white blood cells were analyzed in 61 pregnancies with small for gestation age fetuses and normal Doppler findings for the umbilical artery. The pregnancies were assigned to 2 groups: NRBC≥10 (study group, n=18) and NRBC<10 (control group, n=43). Obstetrical and neonatal outcomes were compared between these groups. The χ2 test or Student's t-test was applied for statistical analysis. The level of significance was set at 5%.
The mean±standard deviation for NRBC per 100 white blood cells was 25.0±13.5 for the study group and 3.9±2.2 for the control group. The NRBC≥10 group and NRBC<10 group were not significantly different in relation to maternal age (24.0 versus 26.0), primiparity (55.8 versus 50%), comorbidities (39.5 versus55.6%) and gestational age at birth (37.4 versus 37.0 weeks). The NRBC≥10 group showed higher rate of caesarean delivery (83.3 versus 48.8%, p=0.02), fetal distress (60 versus 0%, p<0.001) and pH<7.20 (42.9 versus 11.8%, p<0.001). The birth weight and percentile of birth weight for gestational age were significantly lower on NRBC≥10 group (2,013 versus 2,309 g; p<0.001 and 3.8 versus 5.1; p=0.004; respectively). There was no case described of 5th minute Apgar score below 7.
An NRBC higher than 10 per 100 white blood cells in umbilical cord was able to identify higher risk for caesarean delivery, fetal distress and acidosis on birth in small for gestational age fetuses with normal Doppler findings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):264-268
DOI 10.1590/S0100-720320140004935
The aim of this study was to analize and describe some characteristics related to a false diagnosis of intrauterine growth restriction (IUGR).
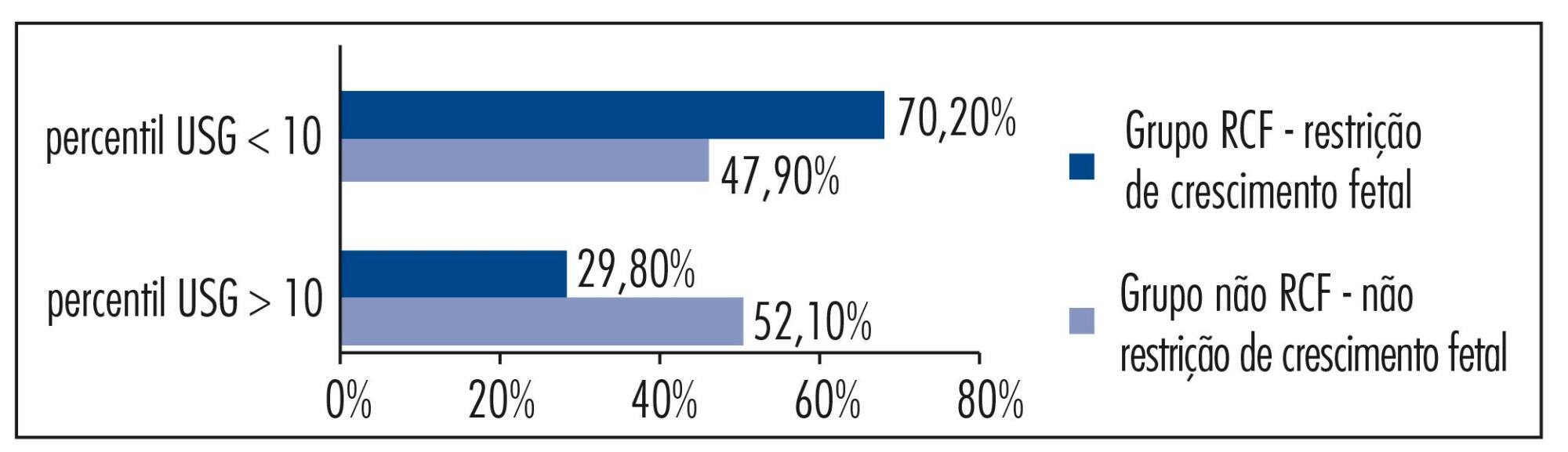
We retrospectively included 48 pregnant women referred to our service with a suspected diagnosis of IUGR that was not confirmed after birth and we compared them to another group with confirmed IUGR. We then analyzed the characteristics of the false-positive results. The results of the study were divided into continuous and categorical variables for analysis. The χ2test or Fisher exact test was applied to compare proportions. The level of significance was set at p<0.05 for all tests.
In our sample, pregnant women with a false diagnosis of IUGR had the following characteristics: they were referred earlier (mean gestational age of 32.8 weeks); were submitted to 2 to 6 ultrasound examinations before been registered in our service; in 25% of cases ultrasound examination was performed before 12 weeks; in 66.7% of cases the symphysis-fundal height measurement was normal; in 52.1% of cases they had at least 1 sonographic exam above the 10th percentile; on average, the last ultrasound examination (performed on average at 36 weeks) was above the 18th percentile; the women were submitted to a mean number of 5 ultrasound examinations and to a mean number of 4.6 vitality exams.
The false diagnosis of IUGR involves high hospital costs and higher demand for specialists. The symphysis-fundal height measurement must be valued, and the diagnosis of IUGR must be confirmed with ultrasonography in the last weeks of pregnancy before any obstetric management is taken.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):420-425
DOI 10.1590/S0100-72032010000900002
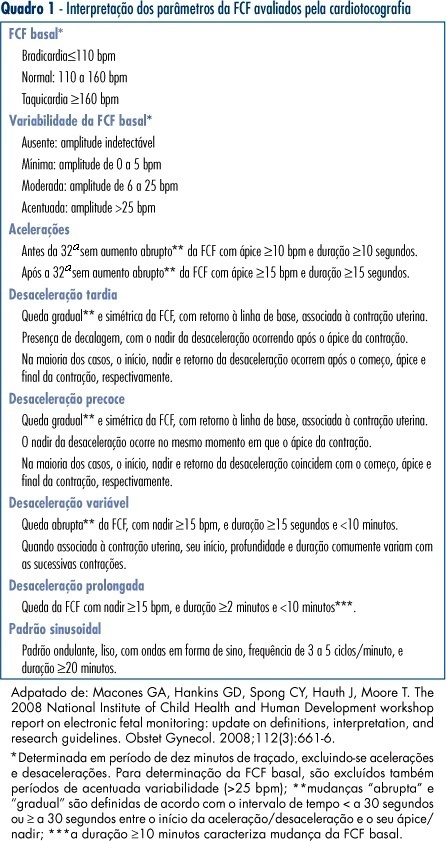
PURPOSE: to compare the patterns of fetal heart rate (FHR) in the second and third trimesters of pregnancy. METHODS: a prospective and comparative study performed between January 2008 and July 2009. The inclusion criteria were: singleton pregnancy, live fetus, pregnant women without clinical or obstetrical complications, no fetal malformation, gestational age between 24 and 27 weeks (2nd trimester - 2T) or between 36 and 40 weeks (3rd trimester - 3T). Computerized cardiotocography (System 8002 - Sonicaid) was performed for 30 minutes and the fetal biophysical profile was obtained. System 8002 analyzes the FHR tracings for periods of 3.75 seconds (1/16 minutes). During each period, the mean duration of the time intervals between successive fetal heart beats is determined in milliseconds (ms); the mean FHR and also the differences between adjacent periods are calculated for each period. The parameters included: basal FHR, FHR accelerations, duration of high variation episodes, duration of low variation episodes and short-term variation. The dataset was analyzed by the Student t test, chi-square test and Fisher's exact test. Statistical significance was set at p<0.05. RESULTS: eighteen pregnancies on the second trimester were compared to 25 pregnancies on the third trimester. There was a significant difference in the FHR parameters evaluated by computerized cardiotocography between the 2T and 3T groups, regarding the following results: mean basal FHR (mean, 143.8 bpm versus 134.0 bpm, p=0.009), mean number of transitory FHR accelerations > 10 bpm (3.7 bpm versus 8.4 bpm, p <0.001) and >15 bpm (mean, 0.9 bpm versus 5.4 bpm, p <0.001), mean duration of high variation episodes (8.4 min versus 15.4 min, p=0.008) and mean short - term variation (8.0 ms versus 10.9 ms, p=0.01). The fetal biophysical profile showed normal results in all pregnancies. CONCLUSION: the present study shows significant differences in the FHR characteristics when the 2nd and 3rd trimesters of pregnancy are compared and confirms the influence of autonomic nervous system maturation on FHR regulation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(10):513-526
DOI 10.1590/S0100-72032009001000008
The present context of medical practice demands from the obstetrician and gynecologist broad understanding of the scientific and technological advances of the area. The main purpose of prenatal evaluation is to identify fetuses at risk for adverse events or death, for preventive action to avoid mishappenings. The determination of fetal biophysical profile reaches its maximum efficiency when applied within the clinical context of each case. In high risk gestations, the Doppler velocimetry of the umbilical artery has shown to be useful to improve perinatal outcome. In the fetal growth deficit, due to severe placentary insufficiency, Doppler velocimetry of the venous duct has been showing to be an important tool in handling of the cases before the 34th week of gestation. Although no test itself is considered the best to evaluate the fetus's prenatal vitality, the joint analysis of all methods may lead to a better understanding of the fetal response to hypoxia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(7):352-357
DOI 10.1590/S0100-72032007000700005
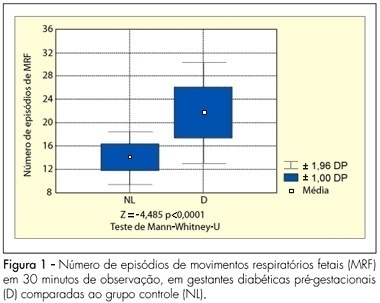
PURPOSE: to analyze the pattern of fetal breathing movements (FBM) in diabetic pregnant women in the third trimester of pregnancy. METHODS: sixteen pregestational diabetic and 16 nondiabetic (control group) pregnant subjects were included fulfilling the following criteria: singleton, between 36-40 weeks of gestation, absence of other maternal diseases and absence of fetal anomalies. The fetal biophysical profile (FBP) was performed to evaluate the following parameters: fetal heart rate, FBM, fetal body movements, fetal tone and amniotic fluid index. The FBM was evaluated for 30 minutes, period when the examination was integrally recorded in VHS video for posterior analysis of the number of FBM episodes, the duration of each episode and the fetal breathing movements index (BMI). The BMI was calculated by the formula: (interval of time with FBM/total time of observation) x 100. At the beginning and in the end of the FBP maternal glucose levels were checked. The results were analyzed by the Mann-Whitney U-test and the Fisher exact test, adopting a level of significance of 5%. RESULTS: the glucose levels demonstrated significantly superior average in the diabetic group (113.3±35.3 g/dL) in relation to the normal group (78.2±14.8 g/dL, p<0.001). The average of the amniotic fluid index was higher in the group of the diabetic cases (15.5±6.4 cm) when compared with controls (10.6±2.0 cm; p=0.01). The average of the number of FBM episodes was superior in the diabetic ones (22.6±4.4) in relation to controls (14.8±2.3; p<0.0001). The average of the BMI in the diabetic patients (54.6±14.8%) was significantly higher than that in the control group (30.5±7.4%, p<0.0001). CONCLUSIONS: the elevated blood glucose levels can be associated with a different pattern in the FBM of diabetic mothers. The use of this parameter of the FBP, in the obstetric practice, must be considered with concern in diabetic pregnancies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(2):77-81
DOI 10.1590/S0100-72031998000200004
Electronic fetal heart rate monitoring (EFM) is the most widely used method of direct fetal surveillance especially during labor. In an attempt to elucidate the effect of EFM on cesarean section (CS) rates, a retrospective study was performed at the University Hospital of Santa Maria (HUSM). We studied two groups of patients, consisting of 2114 pregnant women: EFM group (n=517) and intermittent auscultation (IA) group (n=1597). In the EFM group we observed 38.0% of CS vs. 27.2% in the IA group. For all patients, the CS rate was 29.9%. Fetal distress was the most common indication for CS in the EFM group (40.6%), while previous CS was the third cause (10.1%). On the IA group, fetal distress was the third cause in CS (14.3%), while previous CS was the most common cause (32.4%). On the basis of this study, we believe that EFM has no effect in itself on cesarean section rates considering overall deliveries at HUSM. With proper education of the clinician and correct interpretation of the findings, EFM would not increase cesarean section rates, but rather should allow for a more accurate description of intrapartum fetal well-being.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(3):141-146
DOI 10.1590/S0100-72031999000300004
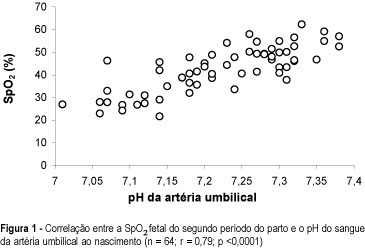
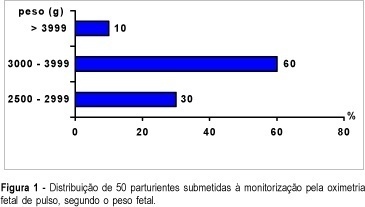
Purpose: to study fetal oxygen saturation (SpO2) levels during labor by continuous pulse oximetry tecnique, and its relation to umbilical artery (UA) pH. Patients and Methods: fetal SpO2 levels were measured during labor by the pulse oximetry technique in 50 subjects. Average values of SpO2 were compared between the first and second stage of labor, with the first stage further subdivided into phases, according to cervical dilatation of (<=4 cm, 5-7 cm and 8-9 cm). SpO2 values were studied in relation to umbilical artery pH at birth ( > or = 7.20 and <7.20). SpO2 > or = 30.0% was considered normal. Results: fetal SpO2 averages during the first stage were 53.0 ± 7.3% and 44.2 ± 6.8% (UA pH > or = 7.20 and <7.20, respectively; p<0.01). When the first stage was subdivided, the fetal SpO2 averages (UA pH > or = 7.20) were 55.1 ± 5.1% (<=4 cm), 52.3 ± 4.6% (5-7 cm) and 51.5 ± 7.2% (8-9 cm); for UA pH <7.20, the fetal SpO2 averages were 46.3 ± 5.1% (<=4 cm), 43.6 ± 6.7% (5-7 cm) and 42.8 ± 5.8% (8-9 cm). Considering the UA pH, these differences were statistically significant (p<0.01). Conclusion: a significant decrease of oxygen saturation values was observed during labor when fetal pulse oximetry was used.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(7):381-384
DOI 10.1590/S0100-72031999000700003
Purpose: to study the correlation between fetal oxygen saturation measured by pulse oximetry during second stage of labor and umbilical artery pH at birth. Patients and Methods: fetal oxygen saturation (FSpO2) was monitored by pulse oximetry during the second stage of labor in 64 singleton pregnancies at term, with vertex presentation. Umbilical blood was sampled immediately after delivery for subsequent measurement of venous and arterial blood gases and pH. All fetuses maintained FSpO2 > or = 30% through the first stage of labor, until the start of second stage. Results: the mean FSpO2 at the second stage of labor correlated significantly with umbilical artery pH at birth (n = 64, r = 0.79, p <0.001). There was no significant corre-lation between FSpO2 at the second stage of labor and umbilical artery oxygen saturation at birth. Conclusion: fetal oxygen saturation measured by pulse oximetry during second stage of labor has a good correlation with umbilical artery pH at birth.