-
Review Article
Efficacy of vitamin C supplementation during pregnancy in the prevention of preterm birth: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo1
03-18-2025
Summary
Review ArticleEfficacy of vitamin C supplementation during pregnancy in the prevention of preterm birth: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo1
03-18-2025Views60Abstract
Objective:
Preterm birth is a leading global cause of neonatal mortality and morbidity, with oxidative stress playing a role in its pathogenesis. Vitamin C, a powerful antioxidant, may help reduce this risk. This study assessed the effectiveness of vitamin C supplementation, both alone and with vitamin E, in preventing preterm birth compared to a placebo.
Data source:
Databases were systematically searched in PubMed, Cochrane and Embase in December 2023 and updated in May 2024.
Study Selection:
Included RCTs evaluated vitamin C's effect on preterm birth and related neonatal outcomes.
Data collect:
Statistical analyses used a random-effects model for pooled risk ratios (RR) and 95% confidence intervals (CI). Heterogeneity was assessed with the I² statistic.
Data synthesis:
Seventeen RCTs (21,567 patients) were analyzed. Vitamin C supplementation showed no significant difference compared to placebo for preterm birth (RR 1.04; 95% CI 0.96, 1.14). No significant differences were observed for neonatal death (RR 0.77; 95% CI 0.55, 1.08), NICU admission (RR 1.03; 95% CI 0.95, 1.13), preterm PROM (RR 1.04; 95% CI 0.63, 1.71), or birth weight (MD 52.41; 95% CI −19.65, 124.47). A slight decrease in gestational age was observed (MD 0.26; 95% CI −0.02, 0.55).
Conclusion:
Vitamin C supplementation alone or in combination with vitamin E does not significantly prevent preterm birth or improve related neonatal outcomes.
Key-words Ascorbic acidFetal membranes, premature ruptureGestational ageIntensive care units, neonatalPregnancyPremature birthVitamin C supplementationVitamin ESee more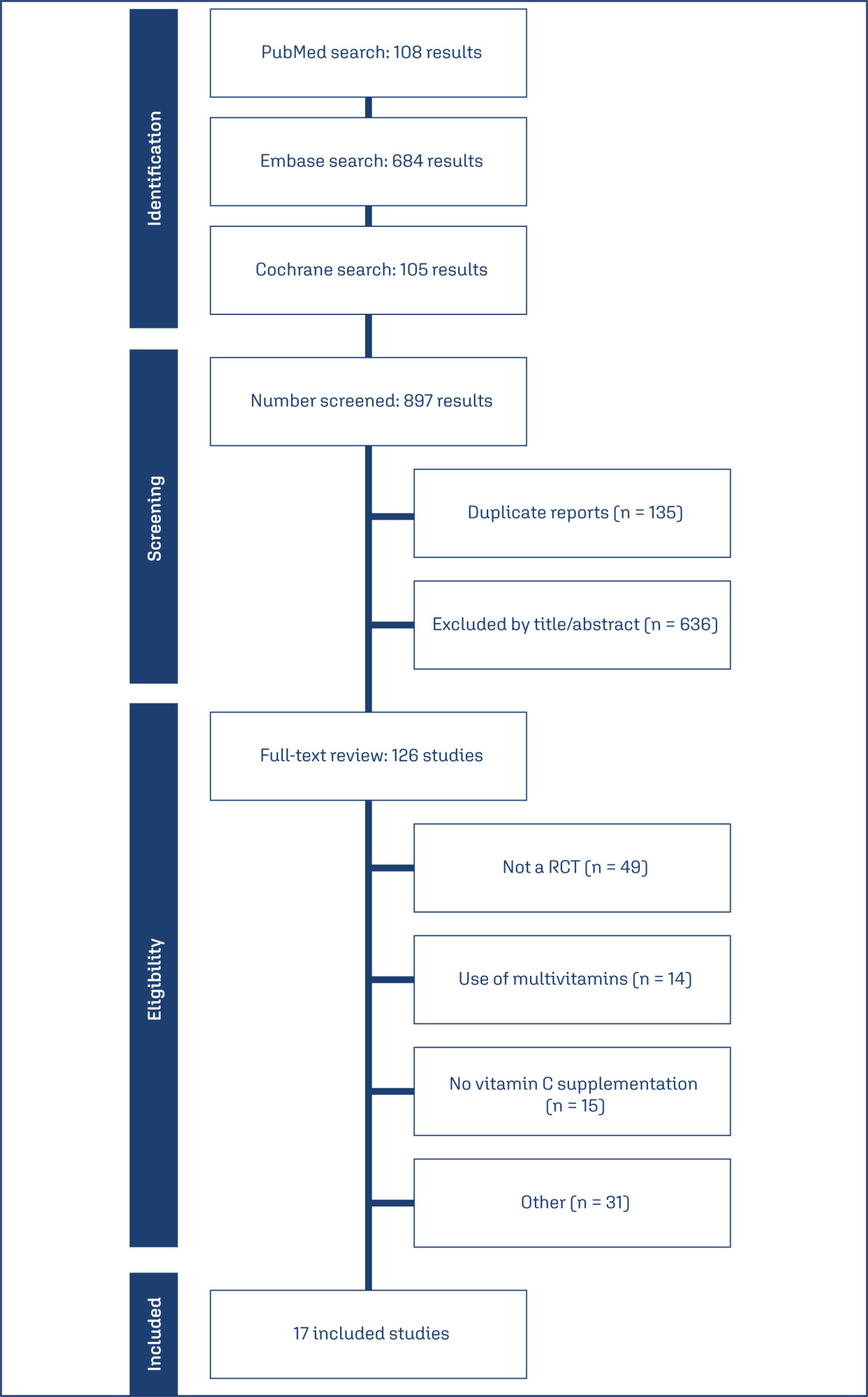
-
Artigos Originais
Premature labour with or without preterm premature rupture of membranes: maternal, obstetric and neonatal features
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(9):428-433
09-01-2015
Summary
Artigos OriginaisPremature labour with or without preterm premature rupture of membranes: maternal, obstetric and neonatal features
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(9):428-433
09-01-2015DOI 10.1590/SO100-720320150005283
Views133PURPOSE:
Evaluation of maternal, obstetrics e neonatal features in both spontaneous preterm births (PTB) with or without preterm premature rupture of membranes (PPROM).
METHODS:
Retrospective study of single fetus pregnancies with PTB between 2003 and 2012. Inclusion criteria: PTB associated with ou without PPROM. Exclusion criterias: PTB by medical indication due to fetal/maternal disease and all non accessible or incomplete clinical files. Different characteristics were compared between two groups of PTB: spontaneous PTB without PPROM (sPTB) versus PPROM. Kolmogorov-Smirnov, Levene, χ2, t Student and Mann-Withney tests were used for statistical analysis.
RESULTS:
From 2,393 PTB of single fetus, 1,432 files were analysed, from which 596 were sPTB and 836 PPROM. The socioeconomic conditions were similar in both groups. Multiparity (50.7versus 40.3%), personal history of previous PTB (20.8 versus 10.2%), cervical length (18.2 versus 27.2 mm), lower body index mass (23.4 versus 24.3 kg/m2) and higher infectious parameters (Protein C Reactive: 2.2 versus 1.2 mg/L; Leukocytes: 13.3 versus 12.4x109) were more frequent in PBTs (p<0,001). Neonatal outcomes, specially neurologic outcomes (4.7 versus 2.8%, p<0,001), were worst in PBTs.
CONCLUSION:
PTB with or without PPROM has a complex etiology. From all evaluated features in our study, only maternal thinness, multiparity with a previous PTB, the cervical length and worst systemic infections parameters were significant in sPTB. This group also showed worst neonatal outcomes, specially on neurological outcomes.
Key-words Adrenal cortex hormones/therapeutic useFetal membranes, premature ruptureInfant, prematureObstetric labor, prematureSee more -
Artigos Originais
Perinatal morbidity and mortality in pregnancies that progressed with ruptured membranes at a public hospital in Northern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):442-448
10-01-2014
Summary
Artigos OriginaisPerinatal morbidity and mortality in pregnancies that progressed with ruptured membranes at a public hospital in Northern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):442-448
10-01-2014DOI 10.1590/SO100-720320140004941
Views91PURPOSE:
To identify obstetric and perinatal factors associated with perinatal morbidity and mortality in pregnancies that progressed with ruptured membranes.
METHODS:
A cross-sectional hospital-based study with secondary data from records of patients (n=87) that evolved with the premature rupture of membranes between 24 and 42 weeks of gestation, admitted from January to April 2013 to a public hospital in Acre State, North of Brazil. Data were subjected to bivariate analysis for selection of variables to be used in a multiple regression model according to Poisson logistic regression with robust error.
RESULTS:
The prevalence of perinatal morbidity-mortality was 51.4%, including a 2.3% death rate (2 cases) and a 9.2% fetal neonatal death rate (8 cases). The variables associated with mortality in the final multiple model were: number of prenatal consultations ≥6, with a prevalence ratio (PR) of 0.5 and a 95% confidence interval (95%CI) of 0.3-0.9, gestational age ≥30 weeks (PR=0.6; 95%CI 0.4-0.8), low birth weight (PR=2.9; 95%CI 1.5-5.4), and mechanical ventilation (PR=3.8; 95%CI 2.0-7.2).
CONCLUSION:
Perinatal morbidity and mortality were high among cases of ruptured membranes. Morbidity and mortality were associated with factors such as fewer prenatal visits, extreme prematurity and low birth weight in this group.
Key-words ChorioamnionitisFetal membranes, premature ruptureInfant, low birth weightInfant, prematureMorbiditySee more -
Artigos Originais
Amniotic fluid volume and maternal outcomes in women with preterm premature rupture of membranes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(4):146-151
03-25-2014
Summary
Artigos OriginaisAmniotic fluid volume and maternal outcomes in women with preterm premature rupture of membranes
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(4):146-151
03-25-2014DOI 10.1590/S0100-720320140050.0003
Views123See morePURPOSE:
To describe the potential influence of amniotic fluid on the maternal outcome of preterm premature rupture of membranes (PROM).
METHODS:
An observational, retrospective cohort study was conducted between December 2012 and January 2008 on 86 pregnant women with preterm PROM and a gestational age (GA) of 24 to 35 weeks. The amniotic fluid index (AFI) was used to measure aminiotic fluid volume. Pregnant women were compared at two cut-off points: those with AFI <5.0 and ≥5.0 cm and AFI <3.0 and ≥3.0 cm. We excluded women with hypertensive disorders, diabetesmellitus, fetal malformations and a diagnosis of infections at admission. For statistical analysis, we used the χ2test or Fisher's exact test, when appropriate, and simple linear regression analysis, with the level of significance set at 5%. We calculated the Risk Ratio (RR) and its 95% confidence interval (95%CI).
RESULTS:
When maternal outcomes were assessed by comparing ILA ≥5.0versus <5.0 cm, no significant differences were detected. However, when considering ILA <3.0 and ≥3.0 cm, there was an increased risk of chorioamnionitis (36.7 versus10.7%, RR: 3.4, 95%CI 1.4 -8.3, p=0.004), with no significant differences for the other variables. There was also a statistically significant positive correlation between AFI and gestational age at delivery (R2=0.78, p<0.0001).
CONCLUSIONS:
AFI <3.0 cm causes a three-fold increase in the risk for chorioamnionitis; also, the higher the ILA, the higher the gestational age at delivery.
-
Artigos Originais
Maternal and perinatal outcomes in women with decreased amniotic fluid
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):342-348
10-10-2013
Summary
Artigos OriginaisMaternal and perinatal outcomes in women with decreased amniotic fluid
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):342-348
10-10-2013DOI 10.1590/S0100-72032013000800002
Views103PURPOSE: To determine maternal and perinatal outcomes in pregnant women with low amniotic fluid, according to the amniotic fluid index (AFI). METHODS: A cohort study conducted on 176 patients admitted to the high risk ward of Instituto de Medicina Integral Prof. Fernando Figueira (IMIP), in Recife, Pernambuco, Brazil. Amniotic fluid was measured by the amniotic fluid index, and classified as low when between 5.1 and 7.9 cm, moderate oligohydramnios between 3.1 and 5.0 cm, and severe oligohydramnios when less than or equal to 3.0 cm. To determine the difference between the three groups of categorical variables studied the chi-square and Fisher exact tests were used, when applicable, and for the numerical variables the Mann-Whitney test was applied, with the level of significance set at 5%. RESULTS: Fetal malformation more frequently occurred when oligohydramnios was severe. Hypertensive disorders, however, were associated with moderate oligohydramnios. There was similarity between the three groups in relation to premature rupture of membranes and other causes. Low amniotic fluid was more frequently diagnosed when tested at the gestational age of 32 weeks or earlier. Regarding the perinatal outcomes, the incidence of Apgar score <7 in the 1st and 5th minutes, perinatal death, neonatal jaundice and pulmonary hypoplasia was higher when oligohydramnios was moderate to severe. CONCLUSIONS: Maternal and perinatal causes and outcomes in pregnant women with low amniotic fluid vary with respect to their AFI, severe oligohydramnios being associated with fetal malformation and other adverse perinatal outcomes.
Key-words Amniotic fluidFetal membranes, premature ruptureHypertensionOligohydramniosPrenatal ultrasonographySee more -
Artigos Originais
Cervical length as a predictor of the latent period and infection in preterm premature membranes rupture
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):158-163
05-11-2012
Summary
Artigos OriginaisCervical length as a predictor of the latent period and infection in preterm premature membranes rupture
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):158-163
05-11-2012DOI 10.1590/S0100-72032012000400004
Views48See morePURPOSE: To verify cervical length using transvaginal ultrasonography in pregnant women between 28 and 34 weeks of gestation, correlating it with the latent period and the risk of maternal and neonatal infections. METHODS: 39 pregnant women were evaluated and divided into groups based on their cervical length, using 15, 20 and 25 mm as cut-off points. The latency periods evaluated were three and seven days. Included were pregnant women with live fetuses and gestational age between 28 and 34 weeks, with a confirmed diagnosis on admission of premature rupture of membranes. Patients with chorioamnionitis, multiple gestation, fetal abnormalities, uterine malformations (bicornus septate and didelphic uterus), history of previous surgery on the cervix (conization and cerclage) and cervical dilation greater than 2 cm in nulliparous women and 3 cm in multiparae were excluded from the study. RESULTS: A <15 mm cervical length was found to be highly related to a latency period of up to 72 hours (p=0.008). A <20 mm cervical length was also associated with a less than 72 hour latency period (p=0.04). A <25 mm cervical length was not found to be statistically associated with a 72 hour latency period (p=0,12). There was also no significant correlation between cervical length and latency period and maternal and neonatal infection. CONCLUSION: The presence of a short cervix (<15 mm) was found to be related to a latency period of less than 72 hours, but not to maternal or neonatal infections.
-
Artigos Originais
Group B streptococcus maternal and neonatal colonization in preterm rupture of membranes and preterm labor
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(8):397-403
10-09-2009
Summary
Artigos OriginaisGroup B streptococcus maternal and neonatal colonization in preterm rupture of membranes and preterm labor
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(8):397-403
10-09-2009DOI 10.1590/S0100-72032009000800005
Views46PURPOSE: to indentify the prevalence and risk factors of maternal colonization by group B streptococcus (GBS) in pregnant women with premature labor (PL) and/or premature membrane rupture (PMR). METHODS: two anal and two vaginal swabs were collected from 203 pregnant women with diagnosis of PL or PMR assisted at the practice along one year. Pregnant women with imminent labor at admission were excluded. One swab of each source was placed in a transfer milieu and sent for culture in blood-agar plates; the two remaining swabs were incubated for 24 hours in Todd-Hewitt milieu for further sowing in blood-agar plates. Risk factors were analyzed by the chi-square test, Student's t-test (p-value set at 0.05 and 95% confidence interval) and logistic regression. The following variables were analyzed: age, race, parity and mother schooling; culture results by source and type of culture; admission diagnosis; gestational age at admission; asymptomatic bacteriuria; gestational age at delivery; type of delivery; neonatal GBS colonization rate and immediate neonatal condition. RESULTS: prevalence of maternal GBS colonization was 27.6% (56 cases). The colonization rates according to gestational complications were 30% for PMR, 25.2% for PL and 17.8% for PL + PMR. Univariate analysis has shown that the variables Caucasian race, low level of schooling and bacteriuria were associated with higher colonization rates. Multivariate analysis showed that the presence of urinary infection was the only variable associated with maternal colonization. The GBS detection rate was significantly higher with the use of a selective milieu and collection from both anal and vaginal sources. The neonatal colonization rate was 3.1%. Two cases of early sepsis by GBS occurred in the sample, with prevalence of 10.8 cases per one thousand live births and 50% mortality rate. CONCLUSION: the studied sample showed high maternal colonization rates by Streptococcus agalactiae. To increase GBS detection rate, it is necessary to use a selective culture milieu and to combine anal-rectal and vaginal cultures. There was a high incidence of early neonatal sepsis.
Key-words Fetal membranes, premature ruptureObstetric labor, prematurePregnancy complicationsStreptococcus agalactiaeSee more -
Artigos Originais
Local expression of tumor necrosis factor-alpha on premature rupture of membranes
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):249-253
07-29-2009
Summary
Artigos OriginaisLocal expression of tumor necrosis factor-alpha on premature rupture of membranes
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):249-253
07-29-2009DOI 10.1590/S0100-72032009000500008
Views71PURPOSE: to compare the expression of tumor necrosis factor-alpha (TNF-α) in ovular membranes with premature rupture (MPR) and with opportune rupture; to verify the association between the expression of the TNF-α in ovular membranes and the degree of chorioamnionitis, correlating the expression of the TNF-α and the membranes' time of rupture. METHODS: ovular membranes from 31 parturients with MPR, with gestational ages over 34 weeks, and from parturients with opportune membranes' rupture, with gestational ages equal or over 37 weeks. Chorioamnionitis detection has been done by histopathological analysis. The evaluation of the TNF-α expression has been done by immune-histochemical technique, using the labile streptavidin-biotin-peroxidase (LSAB) method. RESULTS: the average rupture time was 16.6 hours. The ratio of the TNF-α expression in the Control and Study Groups did not show a significant difference (χ2=6.6; p=0.08). In the Study Group, there was no correlation between the degree of chorioamnionitis and the intensity of TNF-α expression (Spearman's coefficient (Rs)=0.4; p=0.02). CONCLUSIONS: there was no significant difference between the TNF-α expression in ovular membranes with premature or opportune rupture; in the Study Group, there was significant association between TNF-α expression and the degree of chorioamnionitis, and there was no association between rupture time and the intensity of TNF-α expression.
Key-words ChorioamnionitisCytokinesFetal membranes, premature ruptureImmune systemPregnancyTumor necrosis factor-alphaSee more


