Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):455-459
DOI 10.1590/SO100-720320150005271
To analyze the obstetrical and neonatal outcomes of pregnancies with small for gestation age fetuses after 35 weeks based on umbilical cord nucleated red blood cells count (NRBC).
NRBC per 100 white blood cells were analyzed in 61 pregnancies with small for gestation age fetuses and normal Doppler findings for the umbilical artery. The pregnancies were assigned to 2 groups: NRBC≥10 (study group, n=18) and NRBC<10 (control group, n=43). Obstetrical and neonatal outcomes were compared between these groups. The χ2 test or Student's t-test was applied for statistical analysis. The level of significance was set at 5%.
The mean±standard deviation for NRBC per 100 white blood cells was 25.0±13.5 for the study group and 3.9±2.2 for the control group. The NRBC≥10 group and NRBC<10 group were not significantly different in relation to maternal age (24.0 versus 26.0), primiparity (55.8 versus 50%), comorbidities (39.5 versus55.6%) and gestational age at birth (37.4 versus 37.0 weeks). The NRBC≥10 group showed higher rate of caesarean delivery (83.3 versus 48.8%, p=0.02), fetal distress (60 versus 0%, p<0.001) and pH<7.20 (42.9 versus 11.8%, p<0.001). The birth weight and percentile of birth weight for gestational age were significantly lower on NRBC≥10 group (2,013 versus 2,309 g; p<0.001 and 3.8 versus 5.1; p=0.004; respectively). There was no case described of 5th minute Apgar score below 7.
An NRBC higher than 10 per 100 white blood cells in umbilical cord was able to identify higher risk for caesarean delivery, fetal distress and acidosis on birth in small for gestational age fetuses with normal Doppler findings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(10):510-515
DOI 10.1590/S0100-72032010001000007
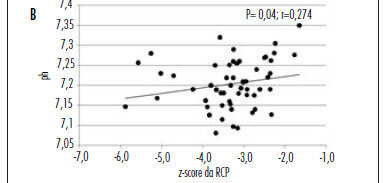
PURPOSE: to evaluate the hypothesis that the fetal cerebroplacental ratio (CPR) is related to acidemia at birth in pregnancies complicated by placental insufficiency detected before 34 weeks of gestation. METHODS: this is a prospective cohort study of 55 patients between 26 and 34 weeks of gestation with a diagnosis of placental insufficiency characterized by abnormal umbilical artery Doppler (pulsatility index>95p). Fetal assessment was performed for each patient by dopplervelocimetry of the umbilical artery, middle cerebral artery and ductus venosus, and by the fetal biophysical profile. CPR was calculated using the ratio between middle cerebral artery pulsatility index and umbilical artery pulsatility index, and the z-score was obtained (number of standard deviations of the mean value at each gestational age). Acidemia at birth was characterized when pH<7.2. RESULTS: of 55 patients, 29 (52.7%) presented acidemia at birth. In the group of fetal acidemia, when compared with the group with pH>7.2, a significant association was observed with CPR values (median 0.47 versus 0.58; p=0.009), pulsatility index of the umbilical artery (median 2.45 versus 1.93; p=0.003), ductus venosus pulsatility index for veins (PIV) (median 1.08 versus 0.85; p=0.034) and suspected or abnormal fetal biophysical profile (37 versus 8%; p=0.031). CPR analysis by z-score showed a negative tendency, but was not statistically significant (p=0.080). Significant correlations were found between pH at birth and CPR (r=0.45; p<0.01), z-score of CPR (r=0.27; p<0.05) and ductus venosus PIV (r=-0.35 p<0.01). CONCLUSION: CPR is associated with the presence of acidemia at birth in pregnancies with placental insufficiency detected before 34 weeks of gestation and this parameter could potentially represent a factor for assessing the severity of fetal involvement.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(10):513-526
DOI 10.1590/S0100-72032009001000008
The present context of medical practice demands from the obstetrician and gynecologist broad understanding of the scientific and technological advances of the area. The main purpose of prenatal evaluation is to identify fetuses at risk for adverse events or death, for preventive action to avoid mishappenings. The determination of fetal biophysical profile reaches its maximum efficiency when applied within the clinical context of each case. In high risk gestations, the Doppler velocimetry of the umbilical artery has shown to be useful to improve perinatal outcome. In the fetal growth deficit, due to severe placentary insufficiency, Doppler velocimetry of the venous duct has been showing to be an important tool in handling of the cases before the 34th week of gestation. Although no test itself is considered the best to evaluate the fetus's prenatal vitality, the joint analysis of all methods may lead to a better understanding of the fetal response to hypoxia.