-
Original Article01-23-2025
Maternal erythrocytosis as a risk factor for small for gestational age at term in high altitude
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo98
Abstract
Original ArticleMaternal erythrocytosis as a risk factor for small for gestational age at term in high altitude
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo98
Views271Abstract
Objective
To determine if maternal erythrocytosis is a risk factor for small-for-gestational age at term at 3,400-m altitude in pregnant women without intercurrent disease.
Methods
Analytical study of retrospective cohorts at Cusco, a city at 3,400-m altitude. Our participants were 224 and 483 pregnant women with and without exposure to maternal erythrocytosis, respectively. A logistic regression with the goodness of fit to the proposed model was also performed with the Hosmer and Lemeshow test, evaluating the small-for-gestational-age results with or without exposure to hemoglobin >14.5 g/dl.
Results
The incidence of small-for-gestational-age was 6.9% for this entire cohort. The maternal erythrocytosis during gestation without any maternal morbidity at 3,400-m altitude has an ORa=0.691 (p=0.271) for small-for-gestational-age at term. Inadequate prenatal control has an ORa=2.115 (p=0.016) for small-for-gestational-age compared to adequate prenatal control.
Conclusion
Maternal erythrocytosis in pregnant women without any morbidity is not a risk factor for small-for-gestational-age at 3,400 m-altitude.
Key-words AltitudeFetal growth retardationGestational agehemoglobinHypoxiaMorbidityNeonatal mortalityPolycythemiaPregnancyPregnant womenRisk factorssmall for gestational ageSee more -
Original Article07-26-2024
Mode of delivery according to Robson classification and perinatal outcomes in restricted and small for gestational age fetuses
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo30
Abstract
Original ArticleMode of delivery according to Robson classification and perinatal outcomes in restricted and small for gestational age fetuses
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo30
Views202Abstract
Objective
To evaluate the mode of delivery according to Robson classification (RC) and the perinatal outcomes in fetal growth restriction (FGR) and small for gestational age (SGA) fetuses.
Methods
Retrospective cohort study by analyzing medical records of singleton pregnancies from two consecutive years (2018 and 2019). FGR was defined according to Delphi Consensus. The Robson groups were divided into two intervals (1–5.1 and 5.2–10).
Results
Total of 852 cases were included: FGR (n = 85), SGA (n = 20) and control (n=747). FGR showed higher percentages of newborns < 1,500 grams (p<0.001) and higher overall cesarean section (CS) rates (p<0.001). FGR had the highest rates of neonatal resuscitation and neonatal intensive care unit admission (p<0.001). SGA and control presented higher percentage of patients classified in 1 - 5.1 RC groups, while FGR had higher percentage in 5.2 - 10 RC groups (p<0.001). FGR, SGA and control did not differ in the mode of delivery in the 1-5.1 RC groups as all groups showed a higher percentage of vaginal deliveries (p=0.476).
Conclusion
Fetuses with FGR had higher CS rates and worse perinatal outcomes than SGA and control fetuses. Most FGR fetuses were delivered by cesarean section and were allocated in 5.2 to 10 RC groups, while most SGA and control fetuses were allocated in 1 to 5.1 RC groups. Vaginal delivery occurred in nearly 60% of FGR allocated in 1-5.1 RC groups without a significant increase in perinatal morbidity. Therefore, the vaginal route should be considered in FGR fetuses.
Key-words Cesarean sectionFetal growth retardationFetusGestational ageInfant, newbornInfant, small for gestational agePregnancy outcomerobson classificationSee more -
Original Article08-07-2023
Prediction of Perinatal and Neurodevelopmental Outcomes in Newborns with a Birth Weight below the 3rd Percentile: Performance of Two International Curves – Prospective Cohort from a Brazilian City
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):225-234
Abstract
Original ArticlePrediction of Perinatal and Neurodevelopmental Outcomes in Newborns with a Birth Weight below the 3rd Percentile: Performance of Two International Curves – Prospective Cohort from a Brazilian City
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):225-234
Views116See moreAbstract
Objectives
To evaluate the performance of Intergrowth-21 st (INT) and Fetal Medicine Foundation (FMF) curves in predicting perinatal and neurodevelopmental outcomes in newborns weighing below the 3rd percentile.
Methods
Pregnant women with a single fetus aged less than 20 weeks from a general population in non-hospital health units were included. Their children were evaluated at birth and in the second or third years of life. Newborns (NB) had their weight percentiles calculated for both curves. Sensitivity, specificity, positive (PPV) and negative predictive value (NPV), and area under the ROC curve (ROC-AUC) for perinatal outcomes and neurodevelopmental delay were calculated using birth weight < 3rd percentile as the cutoff.
Results
A total of 967 children were evaluated. Gestational age at birth was 39.3 (± 3.6) weeks and birth weight was 3,215.0 (± 588.0) g. INT and FMF classified 19 (2.4%) and 49 (5.7%) newborns below the 3rd percentile, respectively. The prevalence of preterm birth, tracheal intubation >24 hours in the first three months of life, 5th minute Apgar <7, admission to a neonatal care unit (NICU admission), cesarean section rate, and the neurodevelopmental delay was 9.3%, 3.3%, 1.3%, 5.9%, 38.9%, and 7.3% respectively. In general, the 3rd percentile of both curves showed low sensitivity and PPV and high specificity and NPV. The 3rd percentile of FMF showed superior sensitivity for preterm birth, NICU admission, and cesarean section rate. INT was more specific for all outcomes and presented a higher PPV for the neurodevelopmental delay. However, except for a slight difference in the prediction of preterm birth in favor of INT, the ROC curves showed no differences in the prediction of perinatal and neurodevelopmental outcomes.
Conclusion
Birth weight below the 3rd percentile according to INT or FMF alone was insufficient for a good diagnostic performance of perinatal and neurodevelopmental outcomes. The analyzes performed could not show that one curve is better than the other in our population. INT may have an advantage in resource contingency scenarios as it discriminates fewer NB below the 3rd percentile without increasing adverse outcomes.
-
Original Article10-01-2018
Analysis of the Performance of 11 Formulae for Fetal Weight Estimation in Preterm Fetuses with Abnormal Doppler Velocimetry – A Retrospective Multicenter Study
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):580-586
Abstract
Original ArticleAnalysis of the Performance of 11 Formulae for Fetal Weight Estimation in Preterm Fetuses with Abnormal Doppler Velocimetry – A Retrospective Multicenter Study
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):580-586
Views174Abstract
Objective
To assess 11 formulae commonly used to estimate fetal weight in a population of premature fetuses who had abnormal Doppler velocimetry due to early-onset placental insufficiency. The performance of each formula was evaluated in subgroups of fetuses with expected growth and intrauterine growth restriction.
Methods
Data were collected fromfetuses andmothers who delivered at three Brazilian hospitals between November 2002 and December 2013.We used the following formulae: Campbell; Hadlock I, II, III, IV and V; Shepard; Warsof; Weiner I and II; and Woo III.
Results
We analyzed 194 fetuses. Of these, 116 (59.8%) were considered appropriate for gestational age (AGA), and 103 (53.1%) were male. The amniotic fluid volume was reduced in 87 (44.8%) fetuses, and the umbilical artery Doppler revealed absence or inversion of diastolic flow in 122 (62.9%) cases, and the analysis of the ductus venosus revealed abnormal flow in 60 (34.8%) fetuses. The Hadlock formulae using three or four fetal biometric parameters had low absolute percentage error in the estimated fetal weight among preterm fetuses with abnormal Doppler studies who were born within 5 days of the ultrasound evaluation. The results were not influenced by the clinical and ultrasound parameters often found in early-onset placental insufficiency.
Conclusion
In this study, the formulae with the best performance for fetal weight estimation in the analyzed population were Hadlock I and IV, which use four and three fetal biometric parameters respectively to estimate the weight of preterm fetuses with abnormal Doppler studies.
Key-words Birth weightDoppler ultrasoundFetal growth retardationFetal weightPlacental insufficiencyPremature birthprenatal ultrasoundultrasoundSee more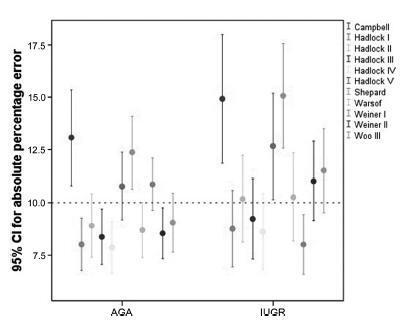
-
Original Article08-21-2015
Relation between nucleated red blood cell count in umbilical cord and the obstetric and neonatal outcomes in small for gestational age fetuses and with normal dopplervelocimetry of umbilical artery
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):455-459
Abstract
Original ArticleRelation between nucleated red blood cell count in umbilical cord and the obstetric and neonatal outcomes in small for gestational age fetuses and with normal dopplervelocimetry of umbilical artery
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):455-459
DOI 10.1590/SO100-720320150005271
Views119PURPOSE:
To analyze the obstetrical and neonatal outcomes of pregnancies with small for gestation age fetuses after 35 weeks based on umbilical cord nucleated red blood cells count (NRBC).
METHODS:
NRBC per 100 white blood cells were analyzed in 61 pregnancies with small for gestation age fetuses and normal Doppler findings for the umbilical artery. The pregnancies were assigned to 2 groups: NRBC≥10 (study group, n=18) and NRBC<10 (control group, n=43). Obstetrical and neonatal outcomes were compared between these groups. The χ2 test or Student's t-test was applied for statistical analysis. The level of significance was set at 5%.
RESULTS:
The mean±standard deviation for NRBC per 100 white blood cells was 25.0±13.5 for the study group and 3.9±2.2 for the control group. The NRBC≥10 group and NRBC<10 group were not significantly different in relation to maternal age (24.0 versus 26.0), primiparity (55.8 versus 50%), comorbidities (39.5 versus55.6%) and gestational age at birth (37.4 versus 37.0 weeks). The NRBC≥10 group showed higher rate of caesarean delivery (83.3 versus 48.8%, p=0.02), fetal distress (60 versus 0%, p<0.001) and pH<7.20 (42.9 versus 11.8%, p<0.001). The birth weight and percentile of birth weight for gestational age were significantly lower on NRBC≥10 group (2,013 versus 2,309 g; p<0.001 and 3.8 versus 5.1; p=0.004; respectively). There was no case described of 5th minute Apgar score below 7.
CONCLUSION:
An NRBC higher than 10 per 100 white blood cells in umbilical cord was able to identify higher risk for caesarean delivery, fetal distress and acidosis on birth in small for gestational age fetuses with normal Doppler findings.
Key-words Diagnostic techniques, obstetrical and gynecologicalErythrocyte countFetal growth retardationFetal hypoxiaFetal monitoringFetal weightPlacental function testsUltrasonography, prenatalSee more -
Original Article02-06-2015
Comparison between two growth curves for small for gestational age diagnosis
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):59-63
Abstract
Original ArticleComparison between two growth curves for small for gestational age diagnosis
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(2):59-63
DOI 10.1590/SO100-720320140005180
Views74See morePURPOSE:
It was to compare the use of two growth curves for the diagnosis of small-for-gestational-age (SGA) infants, having the 10thpercentile as reference.
METHODS:
In a retrospective study, data of 20,567 singleton live births from January 2003 to June 2014 were analyzed, and divided according to gestational age: (a) 23 to 26, (b) 26 to 29, (c) 29 to 32, (d) 32 to 35, (e) 35 to 38, (f) 38 to 41 and (g) >41 weeks. Data were paired and analyzed using the McNemar test, with the level of significance set at 0.05.
RESULTS:
The curve designed by Alexander indicated a higher percentage of diagnosis of SGA than the curve constructed by Fenton for every category of gestational age up to 41 weeks, more markedly in the 32-35 week group (18.5%). Between 37 and 40 weeks of gestational age, Alexander's curve exceeded Fenton's curve in 9.1% of the cases in the diagnosis of SGA.
CONCLUSIONS:
The Fenton curve provides a more accurate evaluation of an infant's growth since it is gender-specific and allows measurement of three parameters. It has also been constructed with newer data and more sophisticated statistical tools.
-
Original Article11-21-2014
Maternal age and adverse perinatal outcomes in a birth cohort (BRISA) from a Northeastern Brazilian city
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):562-568
Abstract
Original ArticleMaternal age and adverse perinatal outcomes in a birth cohort (BRISA) from a Northeastern Brazilian city
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):562-568
DOI 10.1590/SO100-720320140005161
Views123PURPOSE:
To verify the existence of associations between different maternal ages and the perinatal outcomes of preterm birth and intrauterine growth restriction in the city of São Luís, Maranhão, Northeastern Brazil.
METHODS:
A cross-sectional study using a sample of 5,063 hospital births was conducted in São Luís, from January to December 2010. The participants comprise the birth cohort for the study "Etiological factors of preterm birth and consequences of perinatal factors for infant health: birth cohorts from two Brazilian cities" (BRISA). Frequencies and 95% confidence intervals were used to describe the results. Multiple logistic regression models were applied to assess the adjusted odds ratio (OR) of maternal age associated with the following outcomes: preterm birth and intrauterine growth restriction.
RESULTS:
The percentage of early teenage pregnancy (12–15 years old) was 2.2%, and of late (16–19 years old) was 16.4%, while pregnancy at an advanced maternal age (>35 years) was 5.9%. Multivariate analyses showed a statistically significant increase in preterm births among females aged 12–15 years old (OR=1.6; p=0.04) compared with those aged 20–35 years. There was also a higher rate in preterm births among females aged 16–19 years old (OR=1.3; p=0.01). Among those with advanced maternal age (>35 years old), the increase in the prevalence of preterm birth had only borderline statistical significance (OR=1.4; p=0.05). There was no statistically significant association between maternal age and increased prevalence of intrauterine growth restriction.
Key-words Fetal growth retardationGestational ageMaternal agePregnancy outcomePremature birth/etiologySee more -
Original Article06-01-2014
Factors associated with false diagnosis of fetal growth restriction
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):264-268
Abstract
Original ArticleFactors associated with false diagnosis of fetal growth restriction
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):264-268
DOI 10.1590/S0100-720320140004935
Views133PURPOSE:
The aim of this study was to analize and describe some characteristics related to a false diagnosis of intrauterine growth restriction (IUGR).
METHODS:
We retrospectively included 48 pregnant women referred to our service with a suspected diagnosis of IUGR that was not confirmed after birth and we compared them to another group with confirmed IUGR. We then analyzed the characteristics of the false-positive results. The results of the study were divided into continuous and categorical variables for analysis. The χ2test or Fisher exact test was applied to compare proportions. The level of significance was set at p<0.05 for all tests.
RESULTS:
In our sample, pregnant women with a false diagnosis of IUGR had the following characteristics: they were referred earlier (mean gestational age of 32.8 weeks); were submitted to 2 to 6 ultrasound examinations before been registered in our service; in 25% of cases ultrasound examination was performed before 12 weeks; in 66.7% of cases the symphysis-fundal height measurement was normal; in 52.1% of cases they had at least 1 sonographic exam above the 10th percentile; on average, the last ultrasound examination (performed on average at 36 weeks) was above the 18th percentile; the women were submitted to a mean number of 5 ultrasound examinations and to a mean number of 4.6 vitality exams.
CONCLUSION:
The false diagnosis of IUGR involves high hospital costs and higher demand for specialists. The symphysis-fundal height measurement must be valued, and the diagnosis of IUGR must be confirmed with ultrasonography in the last weeks of pregnancy before any obstetric management is taken.
Key-words Diagnostic errorsDiagnostic techniques, obstetrical and gynecologicalFetal growth retardationFetal monitoringFetal weightPlacental function testsUltrasonography, prenatalSee more


