-
Review Article
The use of phosphodiesterase inhibitors in the treatment of female sexual dysfunction: scoping review
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo49
07-26-2024
Summary
Review ArticleThe use of phosphodiesterase inhibitors in the treatment of female sexual dysfunction: scoping review
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo49
07-26-2024Views121See moreAbstract
Objective
The purpose of this study was to analyze the available evidence regarding the efficacy of iPDE5 in the treatment of female sexual dysfunction (FSD).
Methods
A comprehensive literature search was conducted in March 2023 through the main scientific databases.
Results
A total of 53 articles were identified, out of which, 6 met the predefined inclusion criteria. All of these were randomized controlled trials. Among the included studies, 4 demonstrated the effectiveness of sildenafil in improving sexual response and addressing FSD, while 2 studies failed to establish its efficacy in this context.
Conclusion
Overall, the efficacy of sildenafil in the treatment of FSD remains controversial and inconclusive based on the available evidence. Further research is necessary to clarify the therapeutic potential of iPDE5 in addressing FSD and to better understand the factors that influence treatment outcomes.
-
Review Article
Mental Health Disorders in Circumcised Reproductive-age Women, Legal Dimensions and Prevention Strategies: A Narrative Review
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):281-288
08-07-2023
Summary
Review ArticleMental Health Disorders in Circumcised Reproductive-age Women, Legal Dimensions and Prevention Strategies: A Narrative Review
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):281-288
08-07-2023Views185See moreAbstract
Objective:
Female genital mutilation/cutting (FGM/C) can affect women’s lives through various physical, psychological, social and even sexual mechanisms. According to the World Health Organization guidelines for managing the health effects of FGM/C, further research into its psychological effects and preventative measures is required. In this study, a comprehensive review of the mental health consequences of circumcised women of reproductive age has been conducted with a special focus on providing preventive solutions.
Methods:
A comprehensive search of the Web of Science, PubMed(MEDLINE), Proquest ,Scopus and Google scholar was carried outfrom 2000 to 2022. The second stage of search was conducted in grey literature. To facilitate a systematic approach to search the literature, the PECO framework, was adopted.
Results:
The result of this narrative review study showed that, the most common mental health disorder in reproductive age circumcised women were depression, anxiety and post-traumatic stress disorder. Some studies found a significant relationship between parents’ education level and circumcised girls, so that parents of the circumcised women had a low level of education. Two studies considered religious beliefs, tradition, cleanness, sexual desire control and virginity as the reasons for FGM/C.
Conclusion:
All forms of FGM/C may be harmful to one’s health. Women, who have undergone widespread forms of circumcision, are more likely to develop mental disorders. As the psychosocial effects of circumcision can affect the sexual experience of circumcised women, addressing this issue, emphasizing its legal aspects, and providing preventative solutions can improve physical, mental, social, and even sexual health in circumcised women.
-
Original Article
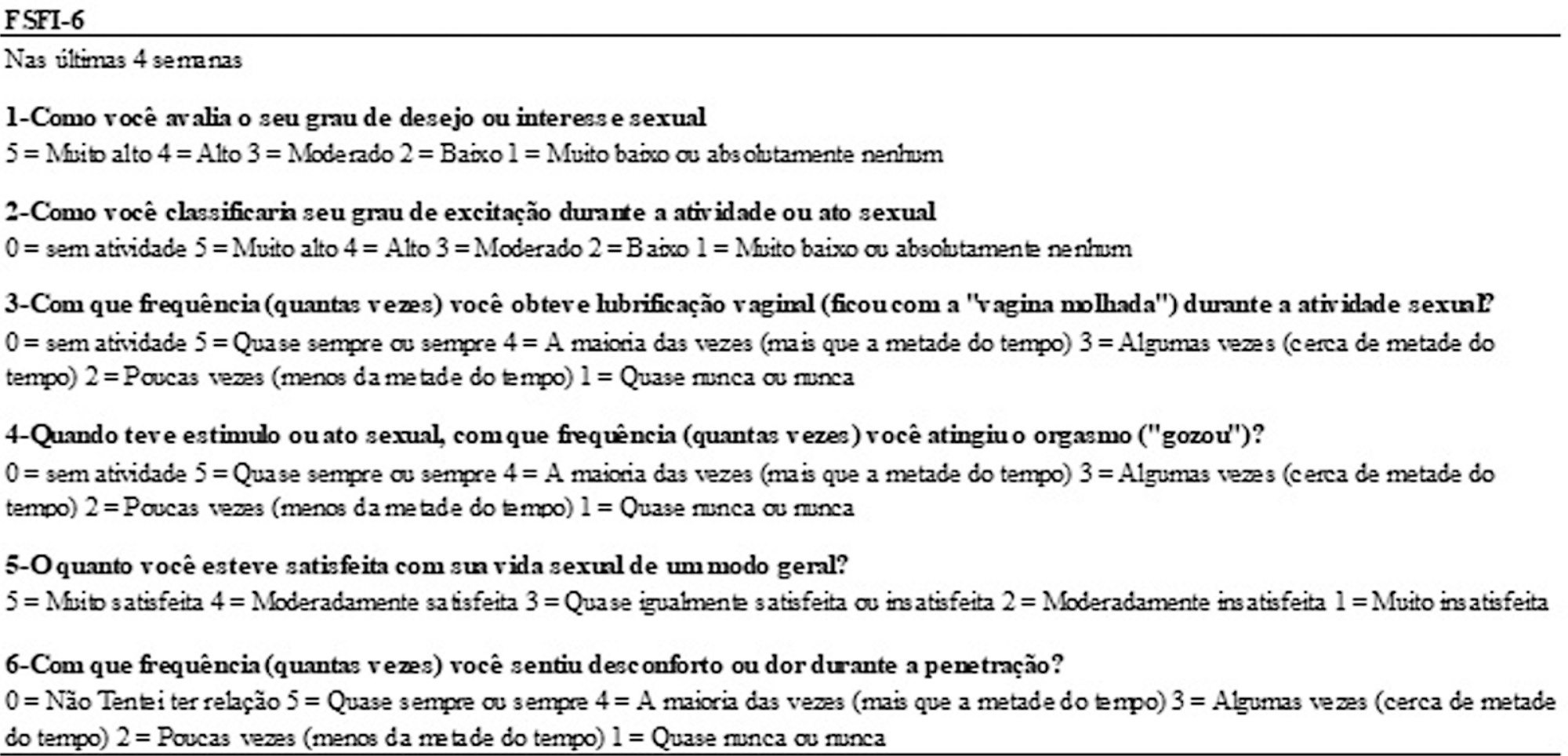
Analysis of the Measurement Properties of the Female Sexual Function Index 6-item Version (FSFI-6) in a Postpartum Brazilian Population
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):089-095
07-10-2023
Summary
Original ArticleAnalysis of the Measurement Properties of the Female Sexual Function Index 6-item Version (FSFI-6) in a Postpartum Brazilian Population
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):089-095
07-10-2023Views155See moreAbstract
Objective
We evaluated internal consistency, test-retest reliability, and criterion validity of the Brazilian Portuguese version of the Female Sexual Function Index 6-item Version (FSFI-6) for postpartum women.
Methods
Therefore, questionnaires were applied to 100 sexually active women in the postpartum period. The Cronbach α coefficient was used to evaluate the internal consistency. Test-retest reliability was analyzed by Kappa for each item of the questionnaire and by the Wilcoxon parametric test, comparing the total scores of each evaluation. For the assessment of criterion validity, the FSFI was used as the gold standard and the receiver operating characteristic (ROC) curve was constructed. Statistical analysis was performed using IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA). It was found that the internal consistency of the FSFI-6 questionnaire was considerably high (0.839).
Results
The test-retest reliability results were satisfactory. It can also be stated that the FSFI-6 questionnaire presented excellent discriminant validity (area under the curve [AUC] = 0.926). Women may be considered as having sexual dysfunction if the overall FSFI-6 score is < 21, with 85.5% sensitivity, 82.2% specificity, positive likelihood ratio of 4.81 and negative likelihood ratio of 0.18.
Conclusion
We conclude that the Brazilian Portuguese version of FSFI-6 is valid for use in postpartum women.
-
Original Article
Applicability, Safety, and Efficiency of Salpingectomy versus Electrocoagulation and Laparoscopic Tubal Section in Ambulatory
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):866-870
08-29-2022
Summary
Original ArticleApplicability, Safety, and Efficiency of Salpingectomy versus Electrocoagulation and Laparoscopic Tubal Section in Ambulatory
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):866-870
08-29-2022Views112See moreAbstract
Objective
Female sterilization is a surgical procedure that aims women to permanently stop the use of conception. The benefits, risks and cost-effectiveness are important issues. The purpose of this study was comparing the applicability, complications and efficacy of salpingectomy versus electrocoagulation and tubal occlusion by laparoscopy in the Ambulatory Surgery Unit.
Methods
We performed a retrospective and observational study that included women undergoing laparoscopic sterilization procedures at our Ambulatory Surgery Unit, during three years. Statistical analysis was performed using SPSS, applying the Fisher exact test, the Mann-Whitney test, and Linear Regression.
Results
Two hundred and twenty-one laparoscopic surgical procedures were performed, including 79 (35.7%) bilateral total salpingectomies and 142 (64.3%) electrocoagulation and bilateral tubal occlusion procedures. The majority of the procedures were performed by a resident (n = 162; 73.3%), with 40% (n = 33) of salpingectomies. The surgical time, independently the type of surgeon, was significantly shorter in the tubal occlusion (42.2 vs. 52.7 min, p < 0.001). Safety and efficacy endpoints were not significantly different between the two groups, with a case of pregnancy in tubal occlusion group.
Conclusion
Salpingectomy is a safe and effective alternative comparing with electrocoagulation and tubal occlusion.
-
Original Articles
Sexual dysfunction in obese women is more affected by psychological domains than that of non-obese
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(12):552-558
12-01-2015
Summary
Original ArticlesSexual dysfunction in obese women is more affected by psychological domains than that of non-obese
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(12):552-558
12-01-2015DOI 10.1590/SO100-720320155443
Views74See moreAbstract
PURPOSE:
To compare differences in the occurrence and changed domains of sexual dysfunction in obese and non-obese Brazilian women.
METHODS:
Female Sexual Function Index, based on six domains, to investigate 31 sexual dysfunction incidence for obese compared to 32 non-obese women, was used. Statistical analysis using ANOVA and MANOVA were performed to compare total scores of Female Sexual Function Index among groups and to identify the differences among domains, Student t -test was used. Statistical significant level was established for all tests for p<0.05.
RESULTS:
No difference in female sexual dysfunction frequency between obese (25.8%) and non-obese women (22.5%) was found. However, an important distinction in which aspects of sexual life were affected was found. While the obese group was impaired in three domains of sexual life (desire, orgasm, and arousal), in the control group five aspects were dysfunctional (desire, orgasm, arousal, pain and lubrication). Future research exploring psychological outcomes in obese females, such as body image and measures of positive and negative effect, might better characterize the female sexual dysfunction in this group.
CONCLUSIONS:
Obesity does not appear to be an independent factor for allow quality of female sexual life. However, disturbance associated to obesity indicates a low frequency of disorder in physical domains, suggesting that psychological factors seem to be mainly involved in the sexual dysfunction in obese women.
-
Artigos Originais
Correlation between age and antral follicles count in infertile women
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):184-188
05-11-2012
Summary
Artigos OriginaisCorrelation between age and antral follicles count in infertile women
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):184-188
05-11-2012DOI 10.1590/S0100-72032012000400008
Views121PURPOSE: To produce age-related nomograms for ovarian antral follicle count (AFC) in infertile women. METHODS: It was done a cross-sectional study of patients attended in the center of assisted reproduction Fêmina, from March 2010 to October 2011. The patients were submitted to transvaginal ultrasonography from day 2 to day 4 of their menstrual period. Patients included were between 21 to 45 years old, with regular menses, two healthy ovaries, without any evidence of endocrinopathies and who gave written informed consent. Patients excluded were smokers, with galactosemia or ovarian cysts, with antecedents of liver disease, ovarian surgeries or who were treated with chemotherapy or radiotherapy. In order to check the evolution of the AFC in relation to patient age, we used the 5th, 25th, 50th, 75th and 95th percentiles. Linear regression was carried out using these percentiles, permitting us to determine the effect of age on the CFA. RESULTS: A total of 172 patients with a mean age of 32.7 years were included in the trial. The male and tubal factors were the main causes of infertility, accounting for 65% of cases. The age-related nomogram for the 5th, 25th, 50th, 75th and 95th percentiles of AFC revealed that changes were best fitted by a linear function. The percentiles that showed the highest correlations were 25 (r=-0.9; p<0.001), 50 (r=-0.9; p<0.001) and 75 (r=-0.9; p<0.001). CONCLUSION: A nomogram was constructed correlating age with the different AFC percentiles in infertile women without endocrinopathies. This showed a linear pattern of decline in AFC with age in all percentiles. These nomograms could provide a reference guide for the clinician. However, future validation, with longitudinal data, still is needed.
Key-words Age factorsfemaleFollicle stimulating hormoneInfertilityNomogramsOvarian follicleUltrasonographySee more -
Artigos Originais
Controlled ovarian stimulation and intrauterine insemination: an actual therapy?
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):341-347
01-23-2011
Summary
Artigos OriginaisControlled ovarian stimulation and intrauterine insemination: an actual therapy?
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):341-347
01-23-2011DOI 10.1590/S0100-72032011001100004
Views142PURPOSE: To evaluate the pregnancy rate in intrauterine insemination (IUI), and to determine possible prognostic factors of successful pregnancy. METHODS: A retrospective study of IUI cycles performed in the Reproductive Medicine Unit of Vila Nova de Gaia Hospital, between January 2007 and July 2010. The IUI cycles were preceded by ovarian stimulation and monitored by vaginal ultrasound. Clinical pregnancy rates were analyzed according to the woman’s age, type and duration of infertility, spermatozoa parameters assessed in the spermogram, number of mature follicles and the drug used for ovarian stimulation. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS17), with the level of significance set at p<0.05. RESULTS: The study comprised 139 couples who underwent 220 IUI cycles. The absolute pregnancy rate per cycle was 18.6%. Of the 41 clinical pregnancies, 5 were twin pregnancies (12.1%). The pregnancy rate was higher at ages <30 years (28.5 vs 15.7%; p=0.024), duration of infertility <3 years (23.8 vs 13.9%; p=0.05), normal sperm motility (23.2 vs 10.3%; p=0.01) and with two follicles at the time of insemination (27.7 vs 14.2% for monofollicular growth; p=0.030). The pregnancy rates obtained with clomiphene citrate, gonadotropins and combined clomiphene citrate/gonadotropin were 13.0, 26.1 and 28.6%, respectively, with a statistically significant difference in clinical pregnancy rate between clomiphene citrate and gonadotropin. CONCLUSIONS: IUI remains a natural starting point for conveniently selected couples with infertility. Younger age and normal sperm motility are good prognostic factors. Gonadotrophin stimulation seems to be an important tool for improving the pregnancy rate of IUI.
Key-words Chorionic gonadotropinClomiphene citratefemaleFertility agentsInseminationOvulation InductionPregnancyPrognosisSee more -
Artigos Originais
Obesity as a risk factor to Burch surgery failure
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(4):182-188
06-29-2009
Summary
Artigos OriginaisObesity as a risk factor to Burch surgery failure
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(4):182-188
06-29-2009DOI 10.1590/S0100-72032009000400005
Views115PURPOSE: to observe the impact of obesity and other risk factors on the rate of failure in patients submitted to Burch's surgery for the treatment of urinary incontinence. METHODS: cases study of patients submitted to Burch's surgery, from 1992 to 2003. Patients were evaluated at the second post-surgery appointment (average 66 days) and after one-year follow-up, and classified in two groups: Continent and Non-continent. Variables analyzed were: age, parity, body mass index (BMI), menopause duration, duration of hormonal therapy, urodynamic evaluation, history of urinary tract infection, previous urinary incontinence surgery, diabetes, cystocele and uterine prolapse, time spent in hospital, necessity of self-probing, post-surgical spontaneous micturition, and surgical wound. Data were analyzed with the Statistical Package for Social Sciences 14.0 statistical package. For the comparison of continuous variables, Student's t-test or Mann-Whitney test were used, and Fisher exact and χ2 tests, for the categorical variables (p<0.05). RESULTS: at the second post-surgical evaluation, there was no significant difference between the two groups, concerning the variables analyzed. After one-year follow-up, from a total of 97 patients, 81 were continent and 16, non-continent, BMI and height being different between the groups. In the continent group, average BMI was 27.1 and height, 1.57 m, and, among the non-continent, 30.8 (p=0.02) and 1.52 m (p=0.01). The BMI>30 Odds Ratio was 3.7 (CI95%=1.2-11.5). CONCLUSIONS: obesity has shown to be an important risk factor for the surgery failure in the first follow-up year. Results show that patients with BMI>30 have 3.7 times more chance of being non-continent one-year after Burch's surgery than non-obese patients.
Key-words femaleObesityPostoperative complicationsUrinary incontinence, stressUrological surgical proceduresSee more


