-
Original Article
Sacral neuromodulation therapy for urinary and defecatory disorders: experience in a Latin American public hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo11
00-00-2024
Summary
Original ArticleSacral neuromodulation therapy for urinary and defecatory disorders: experience in a Latin American public hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo11
00-00-2024Views520Abstract
Objective:
To show the experience of a Latin American public hospital, with SNM in the management of either OAB, NOUR or FI, reporting feasibility, short to medium-term success rates, and complications.
Methods:
A retrospective cohort was conducted using data collected prospectively from patients with urogynecological conditions and referred from colorectal surgery and urology services between 2015 and 2022.
Results:
Advanced or basic trial phases were performed on 35 patients, 33 (94%) of which were successful and opted to move on Implantable Pulse Generator (GG) implantation. The average follow-up time after definitive implantation was 82 months (SD 59). Of the 33 patients undergoing, 27 (81%)reported an improvement of 50% or more in their symptoms at last follow-up. Moreover, 30 patients (90%) with a definitive implant reported subjective improvement, with an average PGI-I "much better" and 9 of them reporting to be "excellent" on PGI-I.
Conclusion:
SNM is a feasible and effective treatment for pelvic floor dysfunction. Its implementation requires highly trained groups and innovative leadership. At a nation-wide level, greater diffusion of this therapy among professionals is needed to achieve timely referral of patients who require it.
Key-words Electric stimulation therapyfecal incontinenceIncontinenceNon-obstructive urinary retentionoveractiveSacral neuromodulationUrinary bladderSee more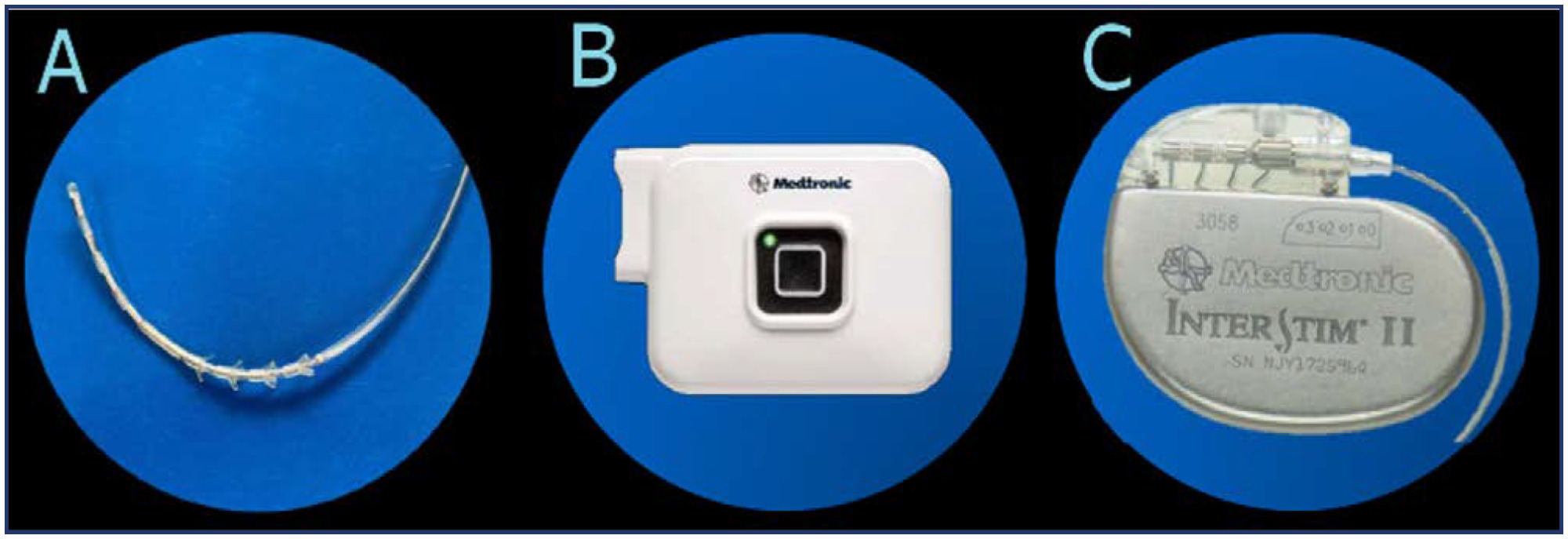
-
Review
Effect of Surgical Treatment for Deep Infiltrating Endometriosis on Pelvic Floor Disorders: A Systematic Review with Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):503-510
02-17-2022
Summary
ReviewEffect of Surgical Treatment for Deep Infiltrating Endometriosis on Pelvic Floor Disorders: A Systematic Review with Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):503-510
02-17-2022Views178See moreAbstract
Objectives
To evaluate the impact of surgical treatment of deep infiltrative endometriosis (DIE) on pelvic floor dysfunction (urinary incontinence [UI], pelvic organ prolapse [POP], fecal incontinence [FI)] or constipation, and sexual function [dyspareunia]).
Data Source
The present systematic review was performed in the PubMed database. For the selection of studies, articles should be published by January 5, 2021, without language restriction.
Study Selection
Six randomized controlled studies that evaluated surgical treatment for DIE and the comparison of different surgical techniques were included.
Data Collection
The studies were selected independently by title and abstract by two authors. Disagreements were resolved by a third author. All included studies were also evaluated according to the Cochrane risk of bias tool and the quality of the evidence was analyzed using the GRADE criteria. Subgroup analysis by different treatments and follow-up periods was also performed.
Results
Six studies were included in the quantitative analysis. The risk of bias between studies showed an uncertain risk of bias for most studies, with concealment of allocation being the least reported category. The quality of the evidence was considered low. High heterogeneity was found between the studies. No study has evaluated UI or POP comparatively before and after surgery.
Conclusion
Dyspareunia and FI have improved after the surgical procedure, but it was not possible to demonstratewhich surgical technique was related to these outcomes as there was surgical heterogeneity. This diversity was found across data, with the recommendation of future prospective studies addressing pelvic floor disorders withDIE.
-
Review Article
Quality of Life in Women with Defecatory Dysfunctions: Systematic Review of Questionnaires Validated in the Portuguese Language
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(3):191-198
03-01-2019
Summary
Review ArticleQuality of Life in Women with Defecatory Dysfunctions: Systematic Review of Questionnaires Validated in the Portuguese Language
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(3):191-198
03-01-2019Views187See moreAbstract
Objective
To identify the quality of life (QoL) assessment instruments related to the health of women with fecal incontinence (FI) or anal incontinence (AI).
Data Sources
Systematic review conducted in the Virtual Health Library (VHL), PubMed and Cochrane Library databases. The descriptors used were: Questionnaire, Questionnaires, Quality of life, validation, validation Studies, anal incontinence, fecal incontinence and constipation. The search was performed between December 26, 2017 and the beginning of January 2018. The limits used were female gender.
Selection of Studies
Initially, 5,143 articles were obtained in the search. The articles of validation for Portuguese of questionnaires for the evaluation of the impact of FI/AI on the QoL of women were considered eligible.
Data Collection
The article search was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) guidelines.
Data Synthesis
Of the 5,143 articles, only 2 fulfilled the inclusion and exclusion criteria: Fecal Incontinence Quality of Life (FIQL) and the Wexner scale (WS). The FIQL evaluates the QoL related to FI, not covering flatus incontinence. The WS assesses flatus incontinence and the severity of the AI. The WS obtained an interclass correlation coefficient (ICC) of 0.932 and a Cronbach α coefficient > 0.90. The FIQL obtained intraexaminer and interexaminer reproducibility ranging from 0.929 to 0.957 and from 0.944 to 0.969, respectively.
Conclusions
The WS and the FIQL have satisfactory reliability and validity for use during gynecological consultations.


