Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo56
07-26-2024
This study aimed to translate and validate the Estro-Androgenic-Symptom Questionnaire in Women (EASQ-W) into Brazilian Portuguese language, as we hypothesized that this tool would be consistent for addressing the specific context of hormonal symptoms in menopause.
In a cross-sectional study, a total of 119 women with Genitourinary Syndrome of Menopause (GSM) and 119 climacteric women without GSM were included. The EASQ-W was translated, and its psychometric properties were rigorously examined. Participants completed questionnaires covering sociodemographic details, the EASQ-W, and the Menopause Rating Scale (MRS). A subgroup of 173 women was re-invited after 4 weeks for test-retest analysis of the EASQ-W. Additionally, the responsiveness of the questionnaire was evaluated in 30 women who underwent oral hormonal treatment.
The internal consistency of the EASQ-W was found to be satisfactory in both GSM and control groups (Cronbach’s alpha ≥ 0.70). Notably, a floor effect was observed in both groups; however, a ceiling effect was only evident in the sexual domain of the GSM group. Construct validity was established by comparing the EASQ-W with the MRS, yielding statistically significant correlations (0.33831-0.64580, p < 0.001). The test-retest reliability over a 4-week period was demonstrated to be satisfactory in both the GSM and control groups (ICC 0.787-0.977). Furthermore, the EASQ-W exhibited appropriate responsiveness to oral hormonal treatment (p < 0.001).
This study successfully translated and validated the Estro-Androgenic-Symptom Questionnaire in Women (EASQ-W) into Brazilian Portuguese, with satisfactory internal consistency, test-retest reliability, and construct validity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):796-807
01-11-2023
Menopause causes several changes in the body that may affect the response to COVID-19. We aimed to investigate the possible association between menopausal status and incidence and outcomes in COVID-19 patients.
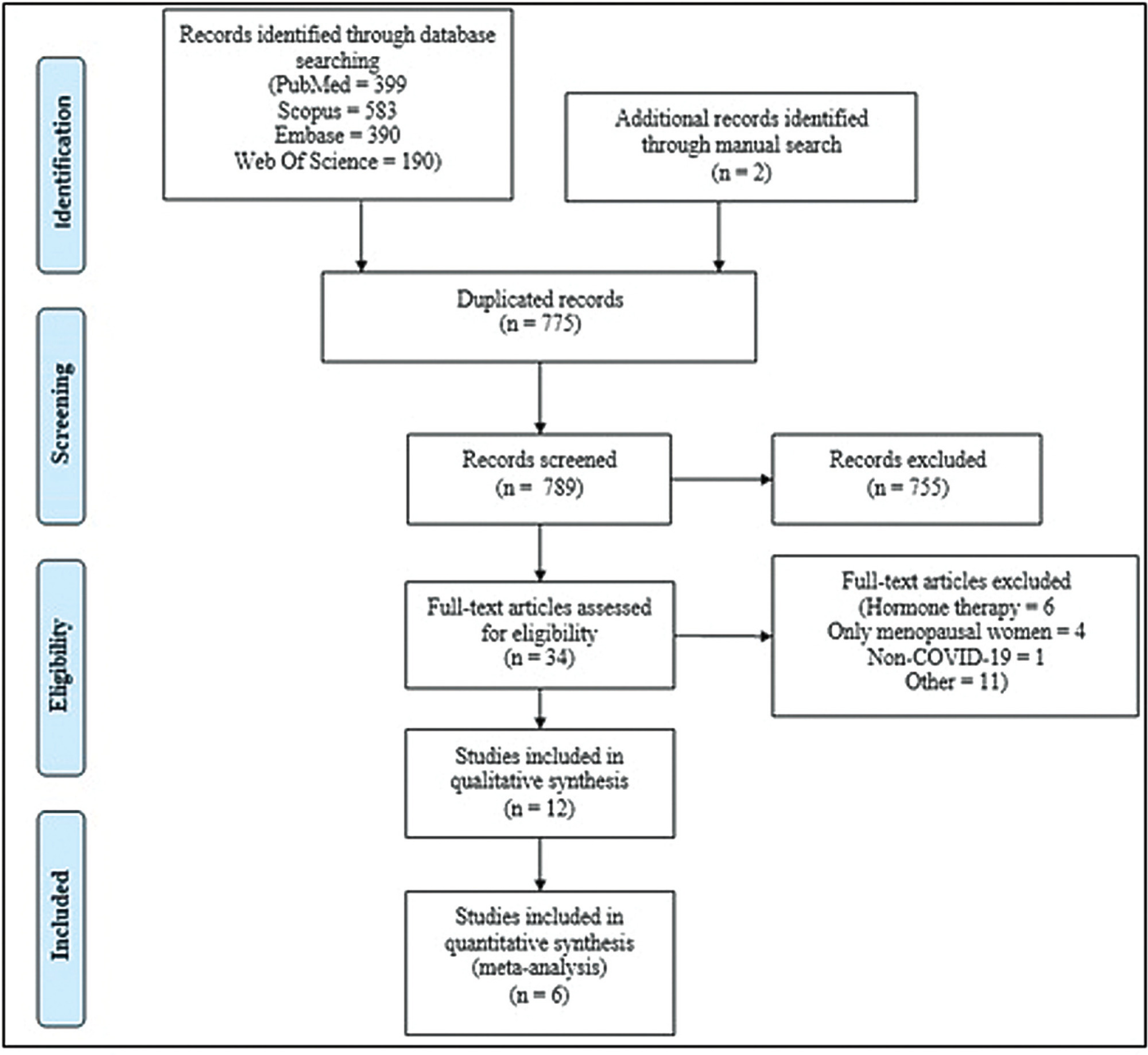
Combinations of keywordsCOVID-19, menopause, and estrogen were used to search the PubMed, Embase, Web-of-Science, and Scopus databases for articles reporting the incidence and outcomes of COVID-19 (discharge, length-of-admission, intensive care, or mortality) in premenopausal women, available through December 29, 2022. Data from studies comparing the incidence of COVID-19 infection with the age-matched male population were pooled and meta-analyzed using a random-effects model.
Overall, 1,564 studies were retrieved, of which 12 were finally included in the systematic review to compare disease outcomes, and 6 were meta-analyzed for the incidence of COVID-19 in premenopausal and postmenopausal women. All studies reported better COVID-19-associated outcomes in premenopausal women compared with postmenopausal women. After adjusting for confounding factors, three studies found better outcomes in postmenopausal women, and two found no association between menopausal status and COVID-19 outcomes. Our meta-analysis found a higher incidence of COVID-19 infection among premenopausal women than postmenopausal women, when compared with age-matched men (odds ratio = 1.270; 95% confidence interval: 1.086–1.486; p = 0.003).
The incidence of COVID-19 was significantly higher in premenopausal women than in postmenopausal women when compared with age-matched men. Although premenopausal women may have more favorable COVID-19-associated outcomes, the presumed preventive effect of estrogens on the incidence and related outcomes of COVID-19 in premenopausal women cannot be proven at present. Further longitudinal studies comparing pre- and post-menopausal women are required to provide further insight into this matter.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):676-682
12-05-2023
Recurrent miscarriage has been linked to hormonal disturbance due to dysregulation of its receptors rather than to the availability of the hormone. We aimed to investigate endometrial expression of progesterone and estrogen receptors in relation to serum and endometrial hormonal levels in unexplained recurrent miscarriage.
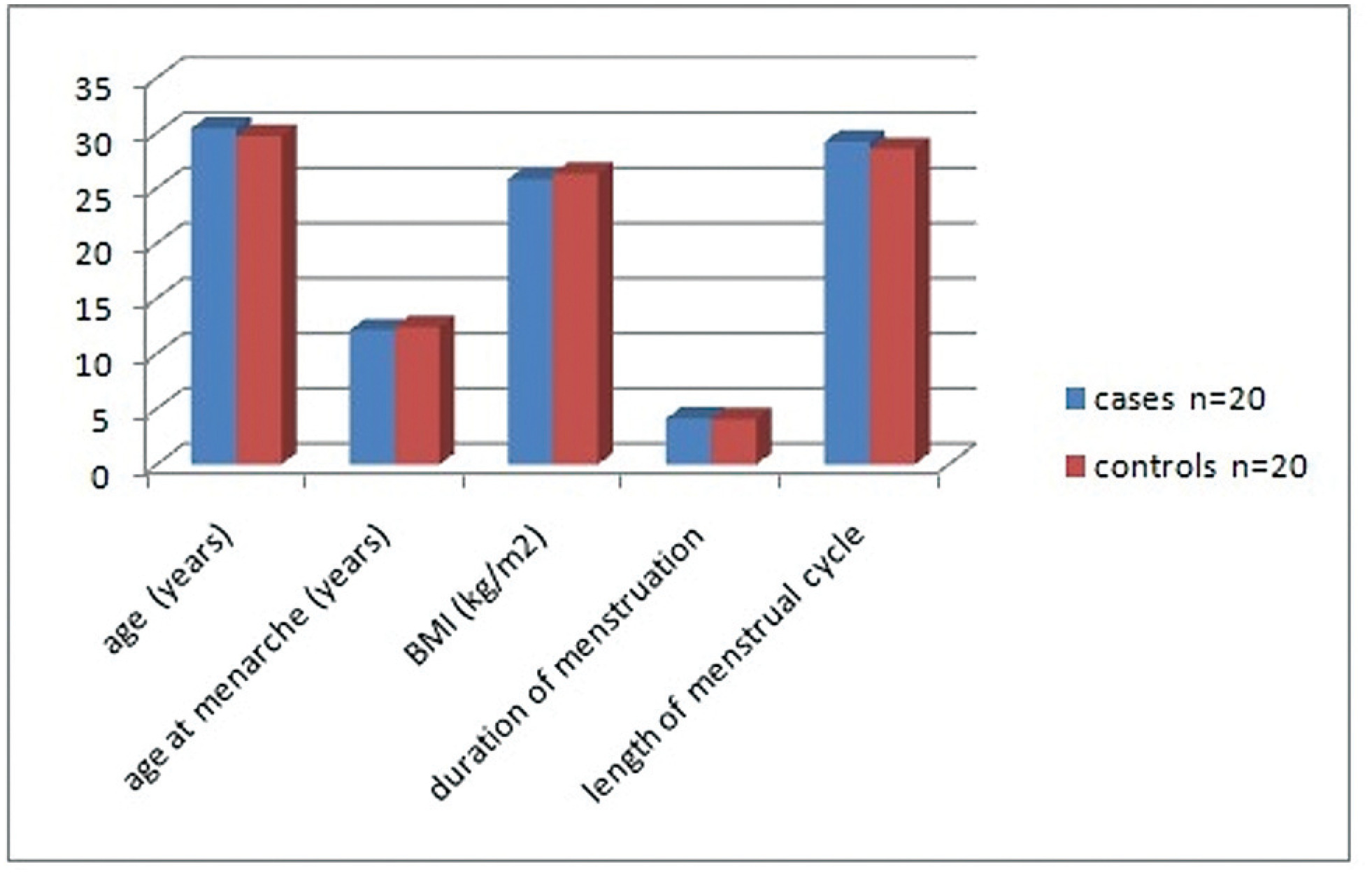
The present case control study included 20 cases with unexplained recurrent miscarriage and 20 parous women as controls. Ovulation was confirmed using an ovulation kit and 10 to 12 days after detecting the urinary luteinizing hormone surge, all women were subjected to a blood sample and to an endometrial biopsy. Progesterone and estrogen levels were measured in serum and in endometrial tissue and receptor concentrations were in the endometrial sample.
Women with recurrent miscarriage showed significantly lower concentration of receptors in both the cytoplasm and the nucleus of endometrial tissue compared with controls. The nuclear/cytoplasm ratio of progesterone receptor was significantly higher in cases compared with controls, implicating that recurrent miscarriage is probably linked to nongenomic activity of the hormone; this was also significant for estrogen receptor. Serum progesterone and estrogen hormonal levels were comparable between groups while both hormones were significantly reduced in the endometrium of recurrent miscarriage cases. Receptors significantly correlated with endometrial hormonal level but not to serum level.
Recurrent miscarriage might be linked to reduced endometrial progesterone and estrogen receptors and appears to be more related to nongenomic activity of progesterone. Endometrial receptors expression correlates to tissue hormonal level rather than to serum hormonal level.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(7):449-453
08-15-2019
To analyze the effects of estrogen alone or in combination with progestogens and tibolone (TIB) on the expression of the extracellular matrix metalloproteinases 2 and 9 (MMP-2 and MMP-9), of perlecan, and of heparanase (HPSE) of the vascular walls of the carotid arteries.
A total of 30 250-day-old ovariectomized Wistar rats were orally treated for 5 weeks with: a) 1 mg/kg of estradiol benzoate (EB); b) EB + 0.2 mg/kg of medroxyprogesterone acetate (MPA); c) EB + 0.2mg/kg of norethisterone acetate (NETA); d) EB + 2 mg/kg of dydrogesterone (DI); e) 1 mg/kg of TIB; f) placebo (CTR). Following treatment, the expression of mRNA for MMP-2, MMP-9, and HPSE was analyzed by realtime polymerase chain-reaction (PCR), and the expression of MMP-2, of MMP-9, of tissue inhibitor of metalloproteinase 2 (TIMP-2), and of perlecan was quantified by immunohistochemistry in the carotid arteries.
The groups showed significant differences on mRNA HPSE expression (p = 0.048), which was higher in the EB, EB + MPA, and TIB groups. There was no statistically significant difference in mRNA MMP-2 or MMP-9 expression. The immunohistochemical expression of MMP-2, of TIMP-2, of MMP-9, of HPSE, and of perlecan showed no differences between groups.
Estradiol alone or associated with MPA and TIB treatment can increase mRNA HSPE expression of the walls of the carotid arteries in ovariectomized rats.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(5):248-252
10-05-2007
DOI 10.1590/S0100-72032007000500005
PURPOSE: to analyze the isoflavone and estrogen effects on the postmenopausal quality of life. METHODS: this is a randomized and double-blind study with 79 postmenopausal patients, 12 months of amenorrhea, 40 years old or more and body mass index (BMI) above 30 kg/m². The participants were randomly divided into two treatment groups: GECP received orally two capsules, every 12 hours, one contained 0.625 mg conjugated equine estrogen and another placebo (n=33); GECS received two capsules of 150 mg extract of soy, with 60 mg isoflavone (n=32). Both treatments were administered for six months. The Quality Menopause Specific Questionnaire of Life was applied before and after one, three and six months of treatment. The parameters of gynecological cancer risk were evaluated. ANOVA and the Tukey test were used for data analysis. RESULTS: there was a reduction in the values of the vasomotor parameters after six months of treatment, 1.6±0.8 and 2.4±1.6, compared to before therapy, 4.0±2.2 and 4.2±2.3 in GECP and GECS, respectively. The psychological aspects showed reduction in values after six months of therapy, 2.5±1.2 and 2.9±1.4, compared to before treatment, 3.6±1.6 and 4.1±1.9 in GECP and GECS, respectively. Similar results were obtained on the physical aspects and in the sexual symptoms. CONCLUSIONS: isoflavones may positively act on life quality of postmenopausal women. This effect was similar to conjugated equine estrogen.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(5):267-271
04-12-1998
DOI 10.1590/S0100-72031998000500006
Objective:To analyze the levels of endogenous sexual steroids and gonadotrophin in women with and without endometrial cancer. Methodology:We developed a clinical comparative study on 20 postmenopausal women with endometrial cancer and 20 postmenopausal women without endometrial cancer. The age, the postmenopausal time and the index of body mass were used as matching variables. The plasma levels of the endogenous sexual steroids were measured using radioimmunoassay and immunoenzymatic methods. For the statistic analysis we used the Student's t test. Results: The levels of androstenedione (A), total testosterone (t) and free testosterone (TL) were higher in the women with endometrial cancer, and those of the luteinic hormone (LH) were significantly lower values in these women. We also observed that the ratio (E1/A) showed significantly lower in the group of women with cancer, while the ratio (E2/E1) did not present any differences between groups. Conclusions: We emphasize the potentiality of sexual steroids and gonadotrophins in the genesis of endometrial adenocarcinoma in postmenopausal women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(5):273-280
04-12-1998
DOI 10.1590/S0100-72031998000500007
An open-label comparative study was conducted in nine centers in Brazil to evaluate the tolerability and cycle control of two low-dose oral contraceptives containing 20 mg ethynylestradiol/75 mg gestodene and 20 mg ethynylestradiol/150 mg desogestrel, during six treatment cycles. A total of 167 healthy sexually active women were enrolled (77 in the gestodene group and 90 in the desogestrel group) and 138 completed the six-cycle treatment period. A lipid and hemostatic profile was performed for a subgroup of first users. A total of 867 cycles were evaluated. Irregular bleeding did not occur in 95.4% of the cycles evaluated with gestodene and in 91.9% with desogestrel. Tolerability was good with both preparations but there was significantly more nausea in the desogestrel group. Cycle control was good with both preparations with a significantly lower incidence of irregular bleeding with gestodene when all cycles were considered. There were no clinically significant changes in the hemostatic profile. Lipid profile showed a trend to be more favorable after six cycles of treatment with both preparations. Women in the gestodene group did not present changes in the mean weight; in the desogestrel group there was a significant mean weight increase of 1 kg after six cycles of treatment. Compliance with treatment was good with both preparations. Results of this study demonstrated that low-dose preparations containing gestodene or desogestrel combined with 20 mg of ethynylestradiol are well-tolerated oral contraceptives that provide good cycle control.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(5):292-297
08-28-2006
DOI 10.1590/S0100-72032006000500005
PURPOSE: to verify if there is a relationship between the clinical periodontal parameters and estrogen levels and bone mineral density (BMD). METHODS: forty-six post-menopausal women aged 44 to 68 years (52.2±4.8) and 15 women aged 35 to 54 years (44.7±7.5) were evaluated. Periodontal parameters like probing depth (PD), clinical attachment loss (CAL), and missing teeth (MT) were compared with estrogen levels (sufficient and insufficient) and BMD (normal, osteopenic and osteoporotic). Data of the mean difference between the groups were compared by the Aspin-Welch test. RESULTS: the means of PD, CAL and MT, when associated with the normal (2.1±0.5; 2.9±1.4 and 10.6±5.0), osteopenic (2.3±0.7; 3.0±1.1 and 12.8±5.1) and osteoporotic BMD (2.4±0.6; 2.7±0.9 and 14.3±5.7), did not show statistical difference (p>0.05). A significant difference was found between the control group and postmenopausal women for CAL and MT. When compared with the estrogen levels the results did not show a difference regarding the periodontal parameters. CONCLUSION: although some studies showed a positive correlation with osteoporosis and estrogen level, in this population of menopausal women these findings were not confirmed.