Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1047-1051
01-23-2022
The use of granulocyte macrophage colony-stimulating factor (GM-CSF)-containing medium, which is a commercial medium that is used for cultivation of embryos in in vitro fertilization (IVF) treatments, has been suggested to increase the efficiency of this procedure in patients with previous multiple unsuccessful attempts. In this retrospective study, we analyzed GM-CSF-containing embryo culture media compared with traditional culture media in terms of development of embryos, pregnancy, and ongoing pregnancy success and live birth rates.
This is a prospective case control study conducted in a single center. A total of 131 unexplained infertility patients were included in the study. A cohort of 69 patients whose embryos were cultured in GM-CSF-containing medium and a control group of 62 age-matched patients whose embryos were cultured in conventional Sage One Step medium were included in the study. The major study outcomes were achievement of pregnancy and ongoing pregnancy rate at 12 weeks of gestation.
The pregnancy and ongoing pregnancy rates of the patients whose embryos were cultured in GM-CSF-containing medium were 39.13% and 36.23%, respectively. These were higher than the rates of the control group, which were 30.65% and 29.03%, respectively, although this difference was not statistically significant. In addition, the 5th-day embryo transfer percentage in the GM-CSF group was higher than in the control group (34.78% versus 27.4%).
The main findings of our study were that there was no difference between the GM-CSF-enhanced medium and the control group in terms of our major study outcomes. However, blastomere inequality rate and embryo fragmentation rates were lower in the GM-CSF group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):19-24
02-28-2022
To evaluate whether there is an effect of the physician who transfers the embryos on pregnancy rates in in vitro fertilization-intracytoplasmic sperm injection (IVF-ICSI) treatment.
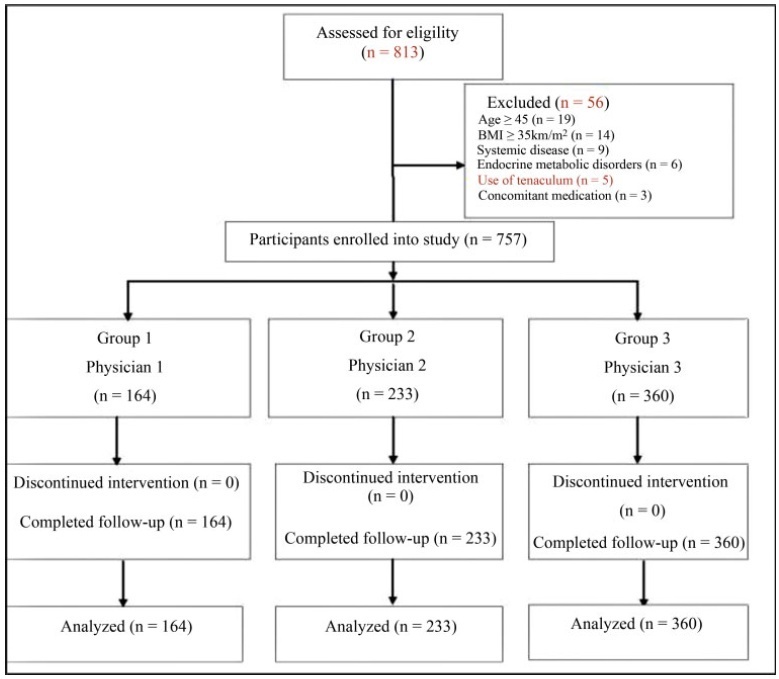
A total of 757 participants were analyzed between 2012 and 2017. Participants were classified according to 3 physicians who transferred the embryos: ([group 1=164 patients]; [group 2=233 patients]; [group 3=360 patients]). Baseline parameters and IVF-ICSI outcomes were compared between the groups.
No differences were determined between the groups regarding the baseline parameters (age, age subgroups [20-29, 30-39, and ≥ 40 years old)], body mass index (BMI), smoking status, infertility period, cause of infertility, baseline follicle stimulating hormone, luteinizing hormone, estradiol (E2), thyroid stimulating hormone, prolactin levels, antral follicle count, duration of stimulation, stimulation protocol, gonadotropin dose required, maximum E2 levels, progesterone levels, endometrial thickness on human chorionic gonadotropin (hCG) administration and transfer days (p>0.05). The numbers of oocytes retrieved,metaphase II (MII), 2 pronucleus (2PN), transferred embryo, fertilization rate, day ofembryo transfer, the catheter effect and embryo transfer technique, and clinical pregnancy rates (CPRs) were also comparable between the groups (p>0.05).
Our data suggests that the physician who transfers the embryos has no impact on CPRs in patients who have undergone IVF-ICSI, but further studies with more participants are required to elucidate this situation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(11):533-546
11-01-2015
DOI 10.1590/SO100-720320150005330
In order to increase the success rate of in vitro fertilization cycles, several studies have focused on the identification of the embryo with higher implantation potential. Despite recent advances in the reproductive medicine, based on the OMICs technology, routinely applicable methodologies are still needed. Thus, in most fertilization centers embryo selection for transfer is still based on morphological parameters evaluated under light microscopy. Several morphological parameters may be evaluated, ranging from the pronuclear to blastocyst stage. In general, despite the day of transfer, some criteria are suggested to present a predictive value for embryo viability when analyzed independently or combined. However, the subjectivity of morphological evaluation, as well as the wide diversity of embryo classification systems used by different fertilization centers shows contrasting results, making the implementation of a consensus regarding different morphological criteria and their predictive value a difficult task. The optimization of embryo selection represents a large potential to increase treatment success rates, allowing the transfer of a reduced number of embryos and inimizing the risks of multiple pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(9):393-397
09-12-2014
DOI 10.1590/SO100-720320140005066
To evaluate the obstetric and perinatal outcomes evolution of triplet pregnancies.
A prospective observational study was conducted in triplet pregnancies delivered over 16 years in a tertiary obstetric center with differentiated perinatal support. Evaluation of demographic factors, obstetric complications, gestational age at delivery, mode of delivery, birth weight and immediate newborn outcome were done over a 16 years period. A global characterization of the sample was performed considering the listed parameters. Variables were categorized in three groups according to year of occurrence: 1996-2000, 2001-2006, 2007-2011, and all parameters were compared.
Of the 33 triplets included, 72.7% resulted from induced pregnancies. All except one patient received prenatal corticosteroids and five received tocolytics. All women delivered prenatally and no significant differences were seen in the mean gestational age at delivery or birth weight towards time. There were three intrauterine fetal deaths. Neonatal immediate outcomes were not significantly different over the years.
Despite remarkable progresses in perinatal and neonatal cares, no noticeable impact in triplet gestations' outcomes was seen, sustaining that triplets should be avoided due to their great risk of prematurity and neonatal morbidities, either by limiting the numbers of embryos transferred or by fetal reduction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):230-234
07-29-2009
DOI 10.1590/S0100-72032009000500005
PURPOSE: to evaluate the patient's age as an outcome predictor in an in vitro fertilization (IVF) program. METHODS: transversal study, which has included 302 women with ages varying from 24 to 46 years old, submitted to IVF, from May 2005 to July 2007. The patients were divided in three groups, according to their age: G<35 (n=161), G 36-39 (n=89) e G>40 (n=52). The number of collected oocytes, the fertilization rates, the number of transferred embryos, the embryonary quality and the pregnancy rate were evaluated. Statistical analysis was realized through Kruskal-Wallis variance analysis and χ2 test. RESULTS: in the G<35 group, an average of 8.8 oocytes by patient was obtained; in the G 36-49 group, 7.4; and in the G>40 group, 1.6. The number of oocytes obtained in G>40 group was significantly lower than in the other two groups (p<0.001).The fertilization rate was similar in the three groups, 61.4, 65.8 e 64.6% (p=0.2288), respectively. The percentage of good quality embryos was not statistically different among the three groups either, with rates of 57.4, 63.2 and 56.0% (p=0.2254), respectively. The average number of transferred embryos in each group was 3.1 (G<35), 2.8 (G 36-39) and 1.5 (G>40), respectively, with statistically significant decrease in the G>40 group (p<0.001). Concerning pregnancy rates, the G>40 group has presented a rate of 9.6%, a result which is significantly lower (p=0.0330) than the one presented by the G<35 and G 36-39 groups (26.1 e 27.0%, respectively), with no significant difference between themselves. CONCLUSIONS: though the embryonary quality is not different among women from different age groups, the number of collected oocytes, the number of transferred embryos and the pregnancy rate indicate that the women's age is an important predictive factor of success for the techniques of assisted reproduction and should be taken into consideration when this kind of treatment is proposed to women over 40.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(12):715-720
03-19-2006
DOI 10.1590/S0100-72032006001200005
PURPOSE: to investigate the effects of previous bilateral tubal sterilization on the outcome of in vitro fertilization. METHODS: retrospective study of 98 consecutive in vitro fertilization cycles. Fifty-five women with previous tubal sterilization without any other infertility factor (TL group) were compared with 43 women with infertility due only to mild male factor (MI group. Age, cancellation rate per induction cycle, response to ovulation induction (number of days of ovulation induction, total amount of gonadotrophin units used, number of follicles and oocytes retrieved), fertilization and cleavage rates, number of transferred embryos and clinical pregnancy per transfer cycle were the variables considered. RESULTS: the cycle discontinuation rate due to poor response, results of ovulation induction, fertilization and cleavage rates, number of transferred embryos and the occurrence of clinical pregnancy were similar in both groups. Considering solely the variable age in TL group, we observed that patients older than 35 years required higher gonadotrophin doses during ovulation induction (2445 versus 2122 IU), presented lower response with fewer follicular growth (11.3 versus 15.8) and less oocytes retrieved (6.1 versus 8.5) compared to younger women (34 years old or less). CONCLUSIONS: tubal sterilization did not interfere with in vitro fertilization outcomes. We observed a worse response to ovulation induction in women older than 35 years, who had previous tubal sterilization.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(6):311-315
08-03-1999
DOI 10.1590/S0100-72031999000600002
Purpose: to verify the effects of the goserelin depot as GnRH agonist for hypophysis suppression, during the controlled ovarian hyperstimulation (COH) for in vitro fertilization and intrauterine embryo transfer (IVF & ET). Method: this is a prospective study of 110 cycles of 101 women. Goserelin depot was administered subcutaneously as a single dose; for some women (87 cycles) it was administered in the first phase of the menstrual cycle, and in 23 cycles it was administered in the luteal phase. The administration of menopausal gonadotropins was daily, until the identification of at least two follicles with a diameter equal to or larger than 18 mm; at this time the chorionic gonadotropin was administered and the follicular aspiration was programmed. Results: the women's age average was 36.7 years (between 23 to 42 years). The main indications for IVF & ET were: tubo-peritoneal factor (75.2%), endometriosis (10.9%), ovulatory factor (7.9%), male factor (3.0%) and unexplained infertility (3.0%). Of the total of the cycles, 28 (25.5%) cycles were cancealed. In 7 cycles (8.04%), for which goserelin depot was administered in the first phase of the menstrual cycle, it was necessary to perform the ovarian cysts aspiration before beginning the ovulation induction. On the average, 3.3 embryos were transferred for each patient (1-5 embryos per woman). Of the total of 70 embryos transferred, 16 clinical pregnancies resulted (pregnancy rate: 22.85%). Conclusion: the goserelin depot administration is a useful alternative for pituitary suppression for IVF & ET, since its results are similar to those observed in the literature, and the patient does not need to come every day to receive medication, a fact of extreme importance in a public service.