Home
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 02-01-2016;38(2):97-111
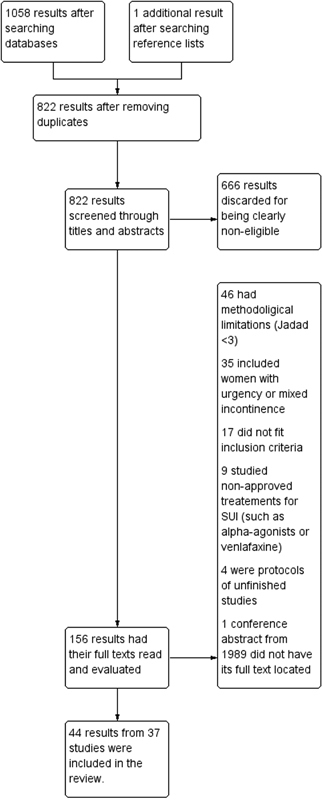
We performed a systematic review and meta-analysis of randomized controlled trials that studied the conservative management of stress urinary incontinence (SUI). There were 1058 results after the initial searches, from which 37 studies were eligible according to previously determined inclusion criteria. For the primary outcomes, pelvic floor muscle training (PFMT) was more efficacious than no treatment in improving incontinence-specific quality of life (QoL) scales (SMD = [1]1.24SDs; CI 95% = [1]1.77 to [1]0.71SDs). However, its effect on pad tests was imprecise. Combining biofeedback with PFMT had an uncertain effect on QoL (MD = [1]4.4 points; CI 95% = [1]16.69 to 7.89 points), but better results on the pad test, although with elevated heterogeneity (MD = 0.9g; 95%CI = 0.71 to 1,10g); group PFMT was not less efficacious than individual treatment, and home PFMT was not consistently worse than supervised PFMT. Both intravaginal and superficial electrical stimulation (IES and SES) were better than no treatment for QoL and pad test. Vaginal cones had mixed results. The association of IES with PFMT may improve the efficacy of the latter for QoL and pad test, but the results of individual studies were not consistent. Thus, there is evidence of the use of PFMT on the treatment of SUI, with and without biofeedback.


Summary
Revista Brasileira de Ginecologia e Obstetrícia. 02-01-2016;38(2):97-111
We performed a systematic review and meta-analysis of randomized controlled trials that studied the conservative management of stress urinary incontinence (SUI). There were 1058 results after the initial searches, from which 37 studies were eligible according to previously determined inclusion criteria. For the primary outcomes, pelvic floor muscle training (PFMT) was more efficacious than no treatment in improving incontinence-specific quality of life (QoL) scales (SMD = [1]1.24SDs; CI 95% = [1]1.77 to [1]0.71SDs). However, its effect on pad tests was imprecise. Combining biofeedback with PFMT had an uncertain effect on QoL (MD = [1]4.4 points; CI 95% = [1]16.69 to 7.89 points), but better results on the pad test, although with elevated heterogeneity (MD = 0.9g; 95%CI = 0.71 to 1,10g); group PFMT was not less efficacious than individual treatment, and home PFMT was not consistently worse than supervised PFMT. Both intravaginal and superficial electrical stimulation (IES and SES) were better than no treatment for QoL and pad test. Vaginal cones had mixed results. The association of IES with PFMT may improve the efficacy of the latter for QoL and pad test, but the results of individual studies were not consistent. Thus, there is evidence of the use of PFMT on the treatment of SUI, with and without biofeedback.


Search
Search in:
