Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo11
00-00-2024
To show the experience of a Latin American public hospital, with SNM in the management of either OAB, NOUR or FI, reporting feasibility, short to medium-term success rates, and complications.
A retrospective cohort was conducted using data collected prospectively from patients with urogynecological conditions and referred from colorectal surgery and urology services between 2015 and 2022.
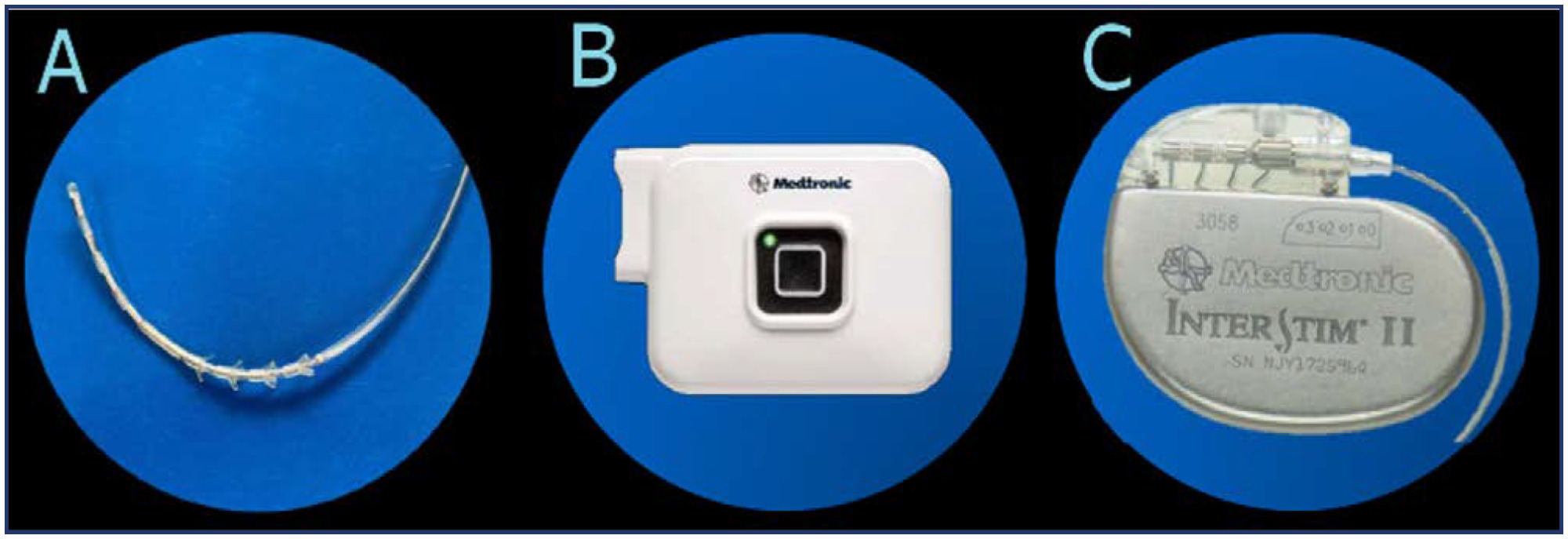
Advanced or basic trial phases were performed on 35 patients, 33 (94%) of which were successful and opted to move on Implantable Pulse Generator (GG) implantation. The average follow-up time after definitive implantation was 82 months (SD 59). Of the 33 patients undergoing, 27 (81%)reported an improvement of 50% or more in their symptoms at last follow-up. Moreover, 30 patients (90%) with a definitive implant reported subjective improvement, with an average PGI-I "much better" and 9 of them reporting to be "excellent" on PGI-I.
SNM is a feasible and effective treatment for pelvic floor dysfunction. Its implementation requires highly trained groups and innovative leadership. At a nation-wide level, greater diffusion of this therapy among professionals is needed to achieve timely referral of patients who require it.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(4):159-163
06-06-2013
DOI 10.1590/S0100-72032013000400005
PURPOSE: To evaluate the effects of electrical stimulation (ES) of the pelvic floor on the urethra of female rats. METHODS: Forty adult rats were divided at random into four groups of ten animals each: Ctrl - without intervention; Sham - not submitted to ES, but with an electrode inserted into the vagina; Exp6 - submitted to six sessions of ES of the pelvic floor, and Exp12 - submitted to 12 sessions of ES of the pelvic floor. At the end of the experiment, all animals were anesthetized and the middle third of the urethra was removed, fixed in Bouin's fluid and processed for histomorphometric study. Sections were stained with hematoxylin and eosin for morphological and morphometric description, and others were stained with picrosirius red for the quantitation of total collagen. The thicknesses of the muscle layer and of the epithelium were determined, in 4 quadrants of the urethra, by performing 20 measurements per animal. The number of blood vessels present in the lamina propria was counted in the four quadrants over an area of 10³ µm² per quadrant and the images were obtained using the image analysis program AxioVision® REL 4.3 (Carl Zeiss). The collagen and muscle fiber ratios in the urethrae were calculated from two images per quadrant of every slice stained with picrosirius red, employing the Imagelab® Program. Data were subjected to analysis of variance (ANOVA) and the Tukey-Kramer multiple comparison test (p<0.05). RESULTS: The morphometry of the collagen, number of blood vessels and thickness of the epithelium showed no significant changes; however, the thickness of the periurethral muscle tissue increased significantly in Exp12 group, compared to the other groups (Exp12*>Exp6==Ctrl==Sham; *p<0.05). CONCLUSION: Prolonged functional electric stimulation of the pelvic floor induced an increase in periurethral muscle thickness in rats.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(5):234-240
08-26-2010
DOI 10.1590/S0100-72032010000500006
PURPOSE: to evaluate the effect of pelvic floor muscle training (PFMT) on female sexual dysfunctions. METHODS: twenty-six women with a diagnosis of sexual dysfunction (sexual desire, arousal, orgasmic disorders and/or dyspareunia) were included in a clinical trial with a before/after approach . The assessment was carried out before, during (after five sessions) and at the end of the treatment (after ten sessions) by two-digit palpation (assessment of pelvic floor muscle, PFM, strength), intravaginal electromyography (EMG) (capture of PFM contraction amplitudes) and Female Sexual Function Index (FSFI, a questionnaire for the evaluation of sexual function). The women underwent PFMT in different positions for ten sessions (once or twice a week). For statistical analysis, absolute and relative frequencies were used for clinical characteristics and PFM strength. The Friedman test was used to compare the FSFI domain scores and EMG values, the Students t-test was used to determine the association between these values and the characteristics of the women, and the Wilcoxon test for percent modification of the EMG. The Mann-Whitney test permitted us to compare these values with clinical characteristics. The Spearman correlation test was used to correlate the EMG values with mean total score. Results were considered statistically significant if p<0.05. RESULTS: a significant improvement (p<0.0001) of FSFI scores was observed at the end of treatment compared to the values observed before and in the middle of treatment. Regarding the EMG, the amplitudes of tonic and phasic contractions increased significantly during treatment (p<0.0001). Pelvic floor strength increased, which 69% of the women presenting grade 4 or 5 at the end of treatment, with a total improvement of sexual complaints. CONCLUSIONS: the PFMT improved muscle strength and electromyography contraction amplitudes, with improved sexual function, indicating that this physiotherapy approach may be successfully used for the treatment of female sexual dysfunctions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(9):447-452
10-30-2009
DOI 10.1590/S0100-72032009000900005
PURPOSE: to compare the effects of functional electrostimulation of the pelvic floor and therapy with cones in women with stress urinary incontinence (SUI). METHODS: randomized clinical study for which 45 patients with SUI were selected. The effects of functional electrostimulation of the pelvic floor were evaluated in the SUI treatment of 24 women, with the use of clinical data (micturition diary, pad test and a questionnaire about quality of life - I-QoL). The patients were submitted to two 20' weekly sessions for four consecutive months, under the supervision of a physiotherapist. The electrode used had 10 cm length and 3.5 cm width with a double metallic ring and a cylindrical shape, positioned in the medium third of the vagina. The electric parameters used were: intensity varying from 10 to 100 mA and 50 Hz of fixed frequency, with pulse duration of 1 ms. Also, we evaluated 21 patients who were submitted to vaginal cone treatment. The cone therapy was done with two 45 minute sessions per week. The cones' weight varied from 20 to 100 gr. RESULTS: there was no difference between the outcomes of electrostimulation of the pelvic floor and the vaginal cones for the treatment of SUI (p>0.05). After four months, there was a significant improvement in the I-QoL index of the patients treated both with electrostimulation (40.3 versus 82.9) or with the cones (47.7 versus 84.1). There was a significant decrease in pad weight in both groups, measured before and after the treatment (28.5 and 32 g versus 2.0 and 3.0 g for the electrostimulation and cone group, respectively). Finally, there was a significant decrease in the number of urinary leakage evaluated by the micturition diary in both groups (p<0.0001). CONCLUSIONS: both electrostimulation and vaginal cones were effective in the treatment of women with SUI.