Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):72-79
To evaluate the diagnostic accuracy of elastography for breast cancer identification in patients with indeterminate lesions on ultrasound.
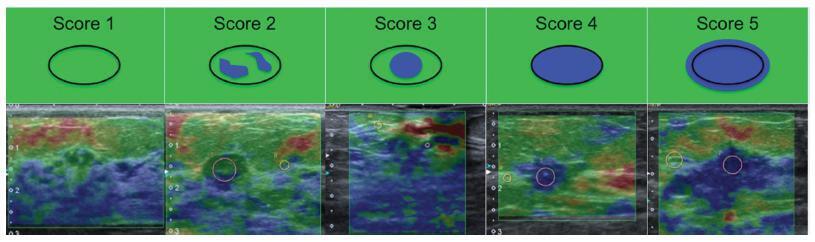
This prospective, descriptive study included patients with indeterminate breast lesions in the ultrasound and with indication for percutaneous or surgical biopsy. The elastography was evaluated by qualitative analysis and by two methods for the semi quantitative analysis.
We evaluated 125 female patients with 159 lesions, with a mean age of 47 years, and a range of 20-85 years. Ultrasound has shown to be a method with good sensitivity (98.1%), but with a lower specificity (40.6%). On the elastography qualitative analysis, the specificity and accuracy were of 80.2% and 81.8% respectively. The mean size of the lesions showed no difference in classification by elastography. For the semiquantitative elastography, the mean values of the malignant lesions were statistically higher when compared with the subcutaneous tissue or the adjacent fibroglandular tissue. The analysis of the receiver operating characteristic (ROC) curves for these two semiquantitativemethods showed that both are considered satisfactory, with an area under the curve above 0.75 and statistical significance (p < 0.0001). The best results were obtained when using the findings of combined conventional ultrasound and qualitative elastography, with 100% sensitivity and 63.2% specificity.
Elastography can be a useful complementary method, increasing the specificity and diagnostic accuracy of conventional ultrasound for the diagnosis of breast cancer in patients with indeterminate breast lesions.