Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(5):224-228
05-01-2017
This study analyzed the effectiveness of the thyroid-stimulating hormone (TSH) as a predictor of insulin resistance (IR) and its association with the clinical and metabolic parameters of women with polycystic ovary syndrome (PCOS) without overt hypothyroidism.
A cross-sectional study was performed. Women with PCOS and without overt hypothyroidism (n = 168) were included.
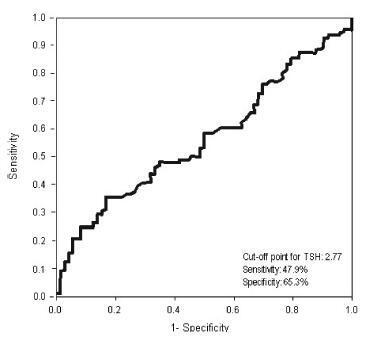
Receiver operating characteristic (ROC) curve was used to determine the cut-off point for TSH that would maximize sensitivity and specificity for a diagnosis of IR using homeostatic model assessment of insulin resistance (HOMA-IR)≥ 2.71. Clinical and metabolic parameters were compared as a function of the TSH cut-off limit and the presence of IR.
Thyroid-stimulating hormone ≥ 2.77 mIU/L was associated with a diagnosis of IR, with sensitivity of 47.9% and specificity of 65.3%. There were no differences in clinical, hormonal or metabolic parameters between TSH < 2.77 and TSH of 2.77 - 10 mIU/L.
In women with PCOS without overt hypothyroidism, TSH ≥2.77 mIU/L is associated with IR; however, with poor sensibility, showing TSH to be a poor predictor of IR in this population. No clinical or metabolic alterations were found that would justify a change in clinical management. Thus, the IR should be investigated in all women with PCOS irrespective of TSH level.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(12):600-608
12-01-2016
Female sexual dysfunction is a complex and common condition that affects women, and the relationship between sexual function and dyslipidemia is poorly studied. This study aims to assess this relationship in the reproductive life women in the menacme who use combined oral contraceptives (COCs) .
A total of 49 healthy women who were sexually active received COC pills that contained ethinylestradiol 30 mcg (EE30) plus levonorgestrel 150 mcg (LNG150). The women were divided into two groups according to their lipid profiles. Dyslipidemia was defined as a high-density lipoprotein (HDL) level < 50 mg/dL or a low-density lipoprotein (LDL) level > 130 mg/dL. Sexual function was assessed using the Female Sexual Function Index (FSFI) Questionnaire. Lipid and lipoprotein parameters were obtained at baseline and after the sixth cycle.
After six cycles of the COCs, the total cholesterol and LDL cholesterol levels in the women with a LDL level > 130 mg/dL decreased by 14.7% and 22.1% respectively. In the women with a HDL level < 50 mg/dL at baseline, the HDL level increased by 15.5% at the end of the study. The arousal and orgasm domains and the FSFI total scores significantly increased in women with and without dyslipidemia. The desire and satisfaction domains increased only in the group without dyslipidemia at the end of the treatment period.
The EE30/LNG150 formulation increased the sexual function and it was only positively correlated with the HDL cholesterol level. These data indicated a low correlation between sexual function and the changes in the lipid and lipoprotein metabolism.