Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(10):473-477
DOI 10.1590/S0100-72032012001000007
PURPOSES: To evaluate the hemodynamic patterns of the ophthalmic artery by Doppler analysis in women with gestational diabetes mellitus (GDM), comparing them to normal pregnant women. METHODS: A prospective case-control study that analyzed the ophthalmic artery Doppler indices in two groups: one consisting of 40 women diagnosed with GDM and the other of 40 normal pregnant women. Included were pregnant women with GDM criteria of the American Diabetes Association - 2012, with 27 weeks of pregnancy to term, and excluded were women with hypertension, use of vasoactive drugs on or previous diagnosis of diabetes. Doppler analysis was performed in one eye with a 10 MHz linear transducer and the Sonoace 8000 Live Medison® equipment . The following variables were analyzed: pulsatility index (PI), resistance index (RI), peak velocity ratio (PVR), peak systolic velocity (PSV) and end diastolic velocity (EDV). To analyze the normality of the samples we used the Lillefors test, and to compare means and medians we used the Student's t-test and Mann-Whitney test according to data normality, with the level of significance set at 95%. RESULTS: The median and mean values with standard deviation of the variables of the ophthalmic artery Dopplervelocimetry group GDM and normal pregnant women were: IP=1.7±0.6 and 1.6±0.4 (p=0.7); IR=0.7 and 0.7 (p=0.9); RPV=0.5±0.1 and 0.5±0.1 (p=0.1), PSV=33.6 and 31.9 cm/sec (p=0.7); VDF=6.3 and 7.9 cm/sec (p=0.4). There was no significant difference in the means and medians of these variables between the two groups of pregnant women. CONCLUSIONS: The ophthalmic artery hemodynamic patterns, analyzed by means of a Doppler technique remained unchanged in the group of pregnant women with GDM compared to the group of normal pregnant women, suggesting that the time of exposure to the disease during pregnancy was too short to cause significant vascular disorders in the central territory.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(5):215-220
DOI 10.1590/S0100-72032012000500005
PURPOSE: To evaluate factors associated with morbidities among Brazilian women aged 40-65 years and with 11 or more years of schooling. METHODS: A secondary analysis of a cross-sectional population-based study was conducted, using an anonymous self-report questionnaire completed by 377 women. Were evaluated, with this instrument, some morbidities (hypertension, diabetes, insomnia and depression) and sociodemographic, behavioral, clinical and reproductive factors. The association between morbidities and independent variables was evaluated by the Χ2 test. Multiple logistic regression analysis with stepwise selection criteria was used to select the major factors associated with morbid conditions. RESULTS: In the multiple regression analysis, insomnia was associated with bad/fair self-perception of health (OR=2.3) and nervousness (OR=5.1). Depression was associated with bad/fair self-perception of health (OR=3.7) and bad/poor leisure (OR=2.8). Hypertension was associated with obesity (OR=3.1) and being in postmenopausal (OR=2.6). Diabetes was associated with age above 50 years (OR=3.9) and obesity (OR=12.5). CONCLUSIONS: The prevalence of morbidities was high and a worse self-perception of health and obesity were the main factors associated with morbidity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):128-132
DOI 10.1590/S0100-72032012000300007
PURPOSE: To evaluate the importance of the oral glucose tolerance test for the diagnosis of glucose intolerance (GI) and type 2 diabetes mellitus (DM-2) in women with PCOS. METHODS: A retrospective study was conducted on 247 patients with PCOS selected at random. The diagnosis of GI was obtained from the two-hour oral glucose tolerance test with 75 g of glucose according to the criteria of the World Health Organization (WHO) (GI: 120 minutes for plasma glucose >140 mg/dL and <200 mg/dL), and the diagnosis of DM-2 was obtained by both the oral glucose tolerance test (DM: 120 minutes for plasma glucose >200 mg/dL) and fasting glucose using the criteria of the American Diabetes Association (impaired fasting glucose: fasting plasma glucose >100 and <126 mg/dL; DM: fasting glucose >126 mg/dL). A logistic regression model for repeated measures was applied to compare the oral glucose tolerance test with fasting plasma glucose. ANOVA followed by the Tukey test was used for the analysis of the clinical and biochemical characteristics of patients with and without GI and/or DM-2. A p<0.05 was considered statistically significant. RESULTS: PCOS patients had a mean age of 24.8±6.3, and body mass index (BMI) of 18.3 to 54.9 kg/m² (32.5±7.6). The percentage of obese patients was 64%, the percentage of overweight patients was 18.6% and 17.4% had healthy weight. The oral glucose tolerance test identified 14 cases of DM-2 (5.7%), while fasting glucose detected only three cases (1.2%), and the frequency of these disorders was higher with increasing age and BMI. CONCLUSIONS: The results of this study demonstrate the superiority of the oral glucose tolerance test in relation to fasting glucose in diagnosing DM-2 in young women with PCOS and should be performed in these patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(12):414-420
DOI 10.1590/S0100-72032011001200007
PURPOSE: to describe lower urinary tract dysfunctions and clinical demographic characteristics of patients with urinary symptoms. This study assessed the prevalence of diabetes mellitus and urodynamic changes in these women. METHODS: We conducted a cross-sectional, retrospective study on 578 women. The prevalence of diabetes mellitus and urodynamic diagnoses was assessed in patients with lower urinary tract dysfunctions, with their respective 95% confidence intervals. The prevalence ratios of urodynamic alterations were calculated according to the diabetes mellitus diagnoses. RESULTS: Seventy-seven patients (13.3%) had diabetes and type 2 diabetes was predominant (96.1%). Stress urinary incontinence was the most frequent urodynamic diagnosis (39%) in diabetic patients, followed by detrusor overactivity (23.4%). The prevalence of urodynamic alterations was associated with diabetes (PR=1.31; 95%CI=1.17-1.48). Changes in detrusor contractility (over- or underactivity) were diagnosed in 42.8% diabetic patients and in 31.5% non-diabetic patients. CONCLUSIONS: Diabetic women had a greater prevalence of urodynamic alterations than the non-diabetic ones. There was no association between diabetes mellitus and detrusor contractility alterations (p=0.80).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(2):81-86
DOI 10.1590/S0100-72032011000200005
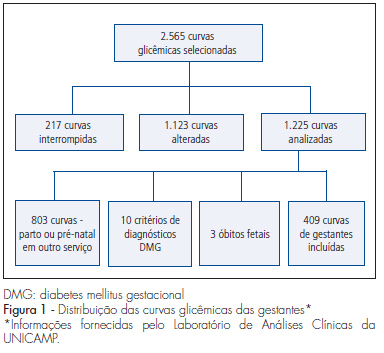
PURPOSE: to determine the prevalence of adverse gestational and neonatal outcomes in women with a positive screening and negative diagnosis for gestational diabetes mellitus (GDM). METHODS: a retrospective descriptive cross-sectional study was conducted from 2000 to 2009 on 409 women with positive screening for GDM. The maternal variables studied were: age, body mass index, history of cesarean section, macrosomia or diabetes mellitus in a previous pregnancy and a personal or family history of diabetes mellitus and chronic arterial hypertension. The neonatal variables studied were: polyhydramnios, gestational age at birth, prematurity, cesarean delivery, large for gestational age (LGA) newborn, macrosomia, Apgar score, neonatal respiratory distress syndrome, hypoglycemia and hyperbilirubinemia. Uni- and multivariate descriptive analyses were first performed regarding risk factors and neonatal outcome and the prevalences and respective 95% confidence intervals were determined. RESULTS: the route of delivery was cesarian section in 255 cases (62.3%), preterm birth occurred in 14.2% of cases and 19.3% of the newborns were LGA. The risk factors correlated with LGA newborns were overweight or obesity, maternal age and a history of macrosomia in a previous pregnancy. CONCLUSIONS: a high rate of LGA newborns was observed in the population with positive risk factors or altered fasting glycemia on the occasion of the first prenatal visit, even when the glycemia curve was normal, with cesarean rates above those habitually observed in populations considered to be of low risk. Pregnant women with these characteristics represent a differential group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(10):504-509
DOI 10.1590/S0100-72032010001000006
PURPOSE: to investigate the application of a multidisciplinary educational program to high-risk pregnancies due to endocrine diseases. METHODS: we retrospectively evaluated the application of a multidisciplinary educational program to 185 pregnant women with endocrine diseases referred to a maternity specialized in high-risk pregnancy. All pregnant women received multidisciplinary prenatal care from a team consisting of endocrinologists, obstetricians, sonographers, nurses and dietitians. Oral and written information about healthy habits, diabetes care, use of artificial sweeteners and exercise during pregnancy was given to all patients at the first endocrine consultation. An individualized nutrition plan was prepared on the occasion of the first visit to the nutritionist. In bi-weekly and monthly endocrine and nutritional visits, respectively, information about healthy changes in lifestyle was emphasized and the weight was recorded. Adherence to physical activity and nutritional counseling was self-reported. We compared the weekly weight before and after the intervention, fetal weight at birth, rate of macrosomia and low birth weight, and frequency of cesarean delivery among the four categories of body mass index (BMI) before pregnancy (<18.5, from 18.5 to 24.9, from 25 to 29.9 and >30 kg/m²). RESULTS: the main disease of referral was diabetes (84.9%). One third of the pregnant women (31.2%) were overweight and 42.5% were obese before pregnancy. Most women was first seen by the multidisciplinary team in the third trimester of pregnancy (64.1%) and 50.5% exceeded the recommended weight gain at first evaluation. Obese women exceeded the recommended weight gain in 62.5% of cases. After the intervention, the percentage of women who exceeded the recommended weekly weight gain was reduced in all categories of pre-pregnancy BMI, although a statistically significant difference was found only in the group with normal pre-pregnancy BMI (40.6 versus 21.9%, p = 0.03). At birth, average fetal weight was similar among the various BMI categories (p=0.277). Macrosomia was more frequent in women who were overweight and obese before pregnancy. Cesarean delivery was the most frequent route of delivery, regardless of pre-pregnancy BMI. CONCLUSIONS: in high-risk pregnancies due to endocrine disorders, a multidisciplinary educational approach limits excessive weekly weight gain despite the advanced gestational age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(2):66-71
DOI 10.1590/S0100-72032010000200003
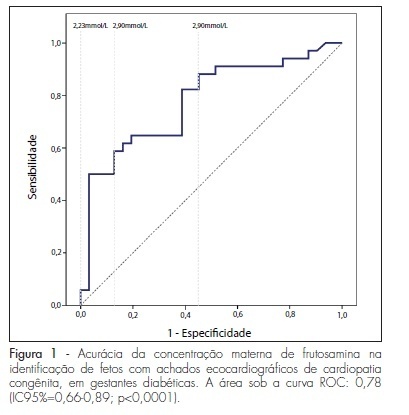
PURPOSE: to evaluate the importance of maternal plasma concentration of fructosamine as an indicator of fetal congenital cardiopathies in pregnancies complicated by diabetes mellitus. METHODS: this was a retrospective study conducted on 91 pregnant women with diabetes mellitus who underwent routine fetal echocardiography at a university reference center in fetal medicine. Sixty-five patientes who presented pre-gestational diabetes mellitus and plasma fructosamine level were registered in the medical records prior to the ultrasound exam. The first measurement recorded was compared with the result of routine fetal echocardiography, carried out by a specialist physician of the service. The presence or absence of echocardiographic findings of congenital cardiopathies (EFCC) was related to plasma levels of fructosamine by the mean t-test and its accuracy for EFCC was verified by the ROC curve. Plsama fructosamine concentrations of 2.68, 2.9 and 2.23 mmol/L, which are, respectively, the local reference laboratory values, the value of the kit employed for measurement and the one of highest overall accuracy, were discussed as the cut-off values. RESULTS: EFCC was found in 52.3% of the fetuses. The first measurement of fructosamine, during the prenatal care period, was performed, on average, at 20.4±8.0 weeks of pregnancy. The maternal concentration ability of the fructosamine to identify fetuses with EFCC was significant (p<0.0001) and had an area under the ROC curve of 0.78 (95%CI=0.66-0.89). The 2.9 mmol/L plasma concentration of fructosamine revealed EFCC with better specificity, but with a higher percentage of false-negative results (96.8 and 55.9%). Values above 2.68 mmol/L were associated with a probability of 4.6 to identify fetuses with EFCC compared with lower values, with 58.8% of sensitivity and 87.1%, specificity. The value of 2.23 mmol/L proved to be the most overall accurate of the three values suggested, with a sensitivity of 88.2% in the identification of fetuses with echocardiographic abnormalities. CONCLUSIONS: it is possible to use a second trimester plasma fructosamine level to refer high risk pregnant women to a reference center of fetal echocardiography. These findings are important for the management of women with diabetes mellitus who initiate late prenatal care.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):241-248
DOI 10.1590/S0100-72032009000500007
OBJECTIVE: to determine the frequency of macrosomia in babies born alive at a reference obstetric service, and its association with maternal risk factors. METHODS: a transversal descriptive study, including 551 women at puerperium, hospitalized at Instituto de Saúde Elpídio de Almeida, in Campina Grande (PB), Brazil, from August to October, 2007. Women, whose deliveries had been assisted at the institution, with babies born alive from one single gestation and approached in the first postpartum day, were included in the study. The nutritional and sociodemographic maternal characteristics were analyzed, and the ratio of macrosomia (birth weight >4.000 g) and its association with maternal variables were determined. Macrosomia was classified as symmetric or asymmetric according to Rohrer's index. Statistical analysis has been done through Epi-Info 3.5 software; the prevalence ratio (PR) and the confidence interval at 95% (CI 95%) were calculated. The research protocol was approved by the local Ethics Committee and all the participants signed the informed consent. RESULTS: the mean maternal age was 24.7 years old, and the mean gestational age was 38.6 weeks. Excessive gestational weight gain was observed in 21.3% of the pregnant women, and 2.1% of the participants had a diagnosis of diabetes mellitus (gestational or clinic). A ratio of 5.4% of macrosomic newborns was found, 60 were asymmetric. There was no significant association between macrosomia, mother's age and parity. There was an association between macrosomia and overweight/obesity in the pre-gestational period (PR=2.9; CI 95%=1.0-7.8) and at the last medical appointment (PR=4.9; CI 95%=1.9-12.5), excessive weight gain (PR = 6.9; CI 95%:2.8-16.9), clinical or gestational diabetes (PR = 8.9; CI 95%:4.1-19.4) and hypertension (PR=2.9; CI 95%=1.1-7.9). The factors that persisted significantly associated with macrosomia in the multivariate analysis were the excessive weight gain during the gestation (RR=6.9; CI 95%=2.9-16.9) and the presence of diabetes mellitus (RR=8.9, CI 95%=4.1-19.4). CONCLUSIONS: considering that excessive gestational weight gain and diabetes mellitus were the factors more strongly associated with macrosomia, it is important that precocious detection measurements and adequate follow-up of such conditions be taken, aiming at preventing unfavorable perinatal outcomes.