-
Review Article
Is it Necessary to Evaluate Fear of Childbirth in Pregnant Women? A Scoping Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(7):692-700
06-29-2022
Summary
Review ArticleIs it Necessary to Evaluate Fear of Childbirth in Pregnant Women? A Scoping Review
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(7):692-700
06-29-2022Views125See moreAbstract
Objective
To review concepts, definitions, and findings about fear of childbirth (FOC).
Methods
A bibliographic review was carried out through the main scientific databases in 2020.
Results
All 32 articles considered potentially relevant were analyzed. A recent study suggests that the global prevalence of FOC can reach up to 14%. Factors such as parity, gestational age, previous birth experience, age and nationality of the woman seem to influence FOC.
Conclusion
Fear of childbirth could be related to an increased risk of adverse obstetric outcomes such as maternal request for cesarean delivery, preterm birth, prolonged labor, postpartum depression, and post-traumatic stress. These evidence highlight the importance of the discussion regarding this topic.
-
Original Article
Impact of Plasmatic Progesterone on the Day of Frozen Embryo Transfer in Hormone-induced Cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):608-615
09-21-2021
Summary
Original ArticleImpact of Plasmatic Progesterone on the Day of Frozen Embryo Transfer in Hormone-induced Cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):608-615
09-21-2021Views167See moreAbstract
Objective
To establish a relationship between serum progesterone values on the day of frozen blastocyst transfer in hormone-replaced cycles with the probability of pregnancy, miscarriage or delivery.
Methods
This was an ambispective observational study including all frozen-thawed embryo transfer cycles performed at our department following in vitro fecundation from May 2018 to June 2019. The outcomes evaluated were β human chorionic gonadotropin (β-hCG)-positive pregnancy and delivery. Groups were compared according to the level of serum progesterone on the day of embryo transfer: the 1st quartile of progesterone was compared against the other quartiles and then the 2nd and 3rd quartiles against the 4th quartile.
Results
A total of 140 transfers were included in the analysis: 87 with β-HCG>10 IU/L (62%), of which 50 (36%) delivered and 37 had a miscarriage (42%).Women with lower progesterone levels (< 10.7ng/mL) had a trend toward higher β-HCG-positive (72 versus 59%; p>0.05), lower delivery (26 versus 39%; p>0.05) and higher miscarriage rates (64 versus 33%; p<0.01). Comparing the middle quartiles (P25-50) with those above percentiles 75, the rate of pregnancy was similar (60 versus 57%; p>0.05), although there was a trend toward a higher number of deliveries (43 versus 31%; p>0.05) and a lower number of miscarriages (28 versus 45%; p>0.05). These differences were not statistically significant.
Conclusion
There were no differences in pregnancy and delivery rates related with the progesterone level when measured in the transfer day. The miscarriage rate was higher in the 1st quartile group.
-
Review Article
Covid-19 and Pregnancy: An Overview
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):420-426
08-26-2020
Summary
Review ArticleCovid-19 and Pregnancy: An Overview
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):420-426
08-26-2020Views156See moreAbstract
Since the World Health Organization (WHO) declared coronavirus infection (COVID-19) a Public Health Emergency of International Concern in January 2020, there have been many concerns about pregnant women and the possible effects of this emergency with catastrophic outcomes inmany countries. Information on COVID-19 and pregnancy are scarce and spread throughout a fewcase series, with no more than 50 cases in total. The present review provides a brief analysis of COVID-19, pregnancy in the COVID-19 era, and the effects of COVID-19 on pregnancy.
-
Original Article
Cesarean Section Rate Analysis in a Tertiary Hospital in Portugal According to Robson Ten Group Classification System
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(6):310-315
07-17-2020
Summary
Original ArticleCesarean Section Rate Analysis in a Tertiary Hospital in Portugal According to Robson Ten Group Classification System
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(6):310-315
07-17-2020Views136See moreAbstract
Objective
The Robson 10 group classification system (RTGCS) is a reproducible, clinically relevant and prospective classification system proposed by the World Health Organization (WHO) as a global standard for assessing, monitoring and comparing cesarean section (CS) rates. The purpose of the present study is to analyze CS rates according to the RTGCS over a 3-year period and to identify the main contributors to this rate.
Methods
We reviewed data regarding deliveries performed from 2014 up to 2016 in a tertiary hospital in Portugal, and classified all women according to the RTGCS. We analyzed the CS rate in each group.
Results
We included data from 6,369 deliveries. Groups 1 (n = 1,703), 2 (n = 1,229) and 3 (n = 1,382) represented 67.7% of the obstetric population. The global CS rate was 25% (n = 1,594). Groups 1, 2, 5 and 10 were responsible for 74.2% of global CS deliveries.
Conclusion
As expected, Groups 1, 2, 5 and 10 were the greatest contributors to the overall CS rate. An attempt to increase the number of vaginal deliveries in these groups, especially in Groups 2 and 5, might contribute to the reduction of the CS rate.
-
Original Articles
Knowledge, Attitude and Practice of Brazilian Obstetricians Regarding Episiotomy
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(11):636-646
12-20-2019
Summary
Original ArticlesKnowledge, Attitude and Practice of Brazilian Obstetricians Regarding Episiotomy
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(11):636-646
12-20-2019Views114Abstract
Objective
To determine the prevalence of episiotomy and the factors associated with the knowledge, attitude and practice (KAP) of Brazilian obstetricians in relation to this procedure.
Methods
A KAP survey was conducted with obstetricians working in Brazil. An electronic form containing structured questions previously evaluated using the Delphi method was created in Google Docs and sent by e-mail. A multivariate logistic regression was performed to determine the principal factors associated with adequate KAP. For each dependent variable (knowledge, attitude and practice) coded as adequate (1 = yes; 0 = no), a multiple logistic regression model was developed. Binary codes (1 = yes and 0 = no) were assigned to every independent or predictor variables. Prevalence ratios (PRs) and their respective 95% confidence intervals (95%CIs) were calculated as measures of relative risk, at a significance level of 5%.
Results
Out of the 13 thousand physicians contacted, 1,163 replied, and 50 respondents were excluded. The mean episiotomy rate reported was of 42%. Knowledge was determined as adequate in 44.5% of the cases, attitude, in 10.9%, and practice, in 26.8% of the cases.
Conclusion
Most respondents had inadequate knowledge, attitudes and practices regarding episiotomy. Although some factors such as age, teaching, working in the public sector and attending congresses improved knowledge, attitude and practice, we must recognize that episiotomy rates remain well above what would be considered ideal. Adequate knowledge is more prevalent than adequate attitude or practice, indicating that improving knowledge is crucial but insufficient to change the outlook of episiotomies in Brazil.
Key-words attitudes in healthDeliveryEpisiotomyhealth knowledgeObstetricsPerineumpractices in healthSee more -
Original Article
Do We Know How to Avoid OASIs in Non-Supine Birth Positions? A Retrospective Cohort Analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):581-587
11-07-2019
Summary
Original ArticleDo We Know How to Avoid OASIs in Non-Supine Birth Positions? A Retrospective Cohort Analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):581-587
11-07-2019Views135See moreAbstract
Objective
To evaluate the association between the upright and supine maternal positions for birth and the incidence of obstetric anal sphincter injuries (OASIs).
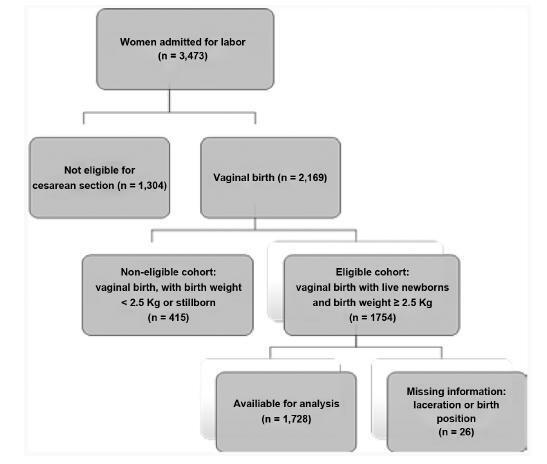
Methods
Retrospective cohort study analyzed the data of 1,728 pregnant women who vaginally delivered live single cephalic newborns with a birth weight of 2,500 g. Multiple regression analyses were used to investigate the effect of the supine and upright positions on the incidence of OASIs after adjusting for risk factors and obstetric interventions.
Results
In total, 239 (13.8%) births occurred in upright positions, and 1,489 (86.2%) in supine positions. Grade-III lacerations occurred in 43 (2.5%) patients, and grade-IV lacerations occurred in 3 (0.2%) women. Supine positions had a significant protective effect against severe lacerations, odds ratio [95% confidence interval]: 0,47 [0.22- 0.99], adjusted for the use of forceps 4.80 [2.15-10.70], nulliparity 2.86 [1.44-5.69], and birth weight 3.30 [1.56-7.00]. Anesthesia (p<0.070), oxytocin augmentation (p<0.228), shoulder dystocia (p<0.670), and episiotomy (p<0.559) were not associated with the incidence of severe lacerations.
Conclusion
Upright birth positions were not associated with a lower rate of perineal tears. The interpretation of the findings regarding these positions raised doubts about perineal protection that are still unanswered.
-
Review Articles
Use of the Pessary in the Prevention of Preterm Delivery
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):53-58
04-15-2019
Summary
Review ArticlesUse of the Pessary in the Prevention of Preterm Delivery
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):53-58
04-15-2019Views199See moreAbstract
Objective
The gestational complication most associated with perinatalmortality and morbidity is spontaneous preterm birth with gestational age < 37 weeks. Therefore, it is necessary to identify its risk factors and attempt its prevention. The benefits of the pessary in prematurity are under investigation. Our objective was to analyze the use of the pessary in the prevention of preterm births in published studies, and to compare its efficacy with other methods.
Methods
Randomized clinical trials published between 2010 and 2018 were selected from electronic databases. Studies on multiple gestations were excluded.
Results
Two studies were in favor of the pessary as a preventive method, one study was contrary to the method and another two showed no statistically significant difference. Themeta-analysis showed no statistical difference with the use of a cervical pessary in the reduction of births < 37 (odds ratio [OR]: 0.63; confidence interval [95% CI]: 0.38-1.06) and < 34 weeks (OR: 0.74; 95% CI: 0.35-1.57)
Conclusion
The pooled data available to date seems to show a lack of efficacy of the cervical pessary in the prevention of preterm birth, although the heterogeneity of the studies made comparisons more difficult.
-
Original Article
Umbilical Cord Blood Gas Analysis, Obstetric Performance and Perinatal Outcome
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):740-748
12-01-2018
Summary
Original ArticleUmbilical Cord Blood Gas Analysis, Obstetric Performance and Perinatal Outcome
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):740-748
12-01-2018Views141See moreAbstract
Objective
To analyze if umbilical artery pH (pHua) ≤7.00 and umbilical artery blood deficit (BDua) ≥12.00 mmol/L are good predictors of adverse neonatal outcomes.
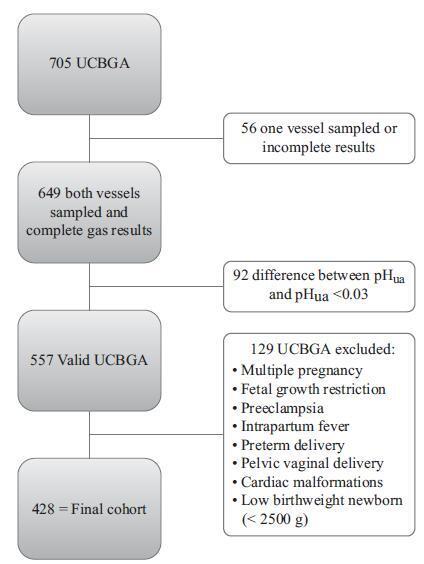
Methods
This was an observational, longitudinal and retrospective cohort study, conducted at the department of obstetrics and gynecology of Centro Hospitalar Tondela Viseu between September 2013 and September 2015. Total cohort and subgroup analysis were performed: group A-women with umbilical cord blood gas analysis (UCBGA) performed for non-reassuring fetal cardiotocographic patterns, placental abruption, or shoulder dystocia; and group B-all the others. Assays were made with the software SPSS for Windows, Versions 20.0 and 21.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 428 UCBGAs met the inclusion criteria. The group analysis revealed an association between group A and pHua ≤7.00, as well as between BDua ≥12.00 mmol/L and 1st minute Apgar score ≤4 (p = 0.011). After the application of the logistic regression models in the total cohort analysis, pHua ≤7.00 had an impact in the occurrence of acute neonatal hypoxia (odds ratio [OR]: 6.71; 95% confidence interval [CI]: 1.21-37.06; p = 0.029); multiparous women had a higher risk of delivering a newborn with first minute Apgar score ≤4 and acute neonatal hypoxia (OR: 5.38; 95% CI: 1.35-21.43; p = 0.017; and OR: 2.66; 95% CI: 1.03-6.89, p = 0.043, respectively); women who had urologic problems during pregnancy had a higher risk of delivering a newborn with 5th minute Apgar score ≤7 (OR: 15.17; 95% CI: 1.29-177.99; p = 0.030); and shoulder dystocia represented a 15 times higher risk of acute neonatal hypoxia (OR: 14.82; 95% CI: 2.20-99.60; p = 0.006).
Conclusion
The pHua and the BDua are predictors of adverse neonatal outcome, and UCBGA is a useful tool for screening newborns at risk. Universal UCBGA should be considered for all deliveries, as it is an accurate screening test for neonatal hypoxia.