-
Original Article
Mid-pregnancy circulating cytokine levels, placental efficiency and their relationship with preterm birth
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo58
07-26-2024
Summary
Original ArticleMid-pregnancy circulating cytokine levels, placental efficiency and their relationship with preterm birth
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo58
07-26-2024Views167See moreAbstract
Objective
To assess a panel of cytokines and placental insufficiency with the risk of preterm delivery (PTD).
Methods
Nested case-control study into the BRISA birth cohort. Eighty-two mother-infant-placenta pairs were selected at 20+0 to 25+6 weeks. Circulating biomarker levels were performed using Luminex flowmetric xMAP technology. Cytokines classified as Th1, Th2 or Th17 and other biomarkers were selected. The ratio between birth weight and placental weight (BW/PW) was used as a proxy for placental efficiency. Spearman correlation, univariate analyses and logistic regression models were calculated. Sensitivity, specificity, positive and negative likelihood ratios were calculated using the Receiver Operating Characteristic curve.
Results
Mean gestational age was 250 days, 14,6% were small for gestational age, 4,8% large for gestational age and 13,4% stunted. Placental efficiency was higher for term newborns (p<0,001), and 18/22 (81%) preterm biomarker values were higher than the control group. Th1 cytokines were highly correlated, while the weakest correlation was observed in other biomarkers. Less education was associated with a higher risk of PTD (p = 0.046), while there was no appreciable difference in the risk of PTD for placental insufficiency. Biomarkers showed negligible adjusted OR of PTD (0.90 to 1.02). IL-6, IL-8, IL-1β, TNFβ, IL-4, IL-13, GCSF, MIP1A, VEGF, EGF, and FGF2 presented a higher sensitivity ranging from 75.56% to 91.11%.
Conclusion
IL-8, IL-12p40, IL-4, IL-13, GCSF, MIP1B, and GMSF in asymptomatic pregnant women were associated with PTD. This finding suggests an activation of maternal inflammatory response.
-
Original Article
Systemic Inflammatory Patterns in Ovarian Cancer Patients: Analysis of Cytokines, Chemokines, and Microparticles
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):780-789
01-11-2023
Summary
Original ArticleSystemic Inflammatory Patterns in Ovarian Cancer Patients: Analysis of Cytokines, Chemokines, and Microparticles
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):780-789
01-11-2023Views161See moreAbstract
Objective
To compare the patterns of systemic inflammatory response in women with epithelial ovarian cancer (EOC) or no evidence of malignant disease, as well as to evaluate the profile of systemic inflammatory responses in type-1 and type-2 tumors. This is a non-invasive and indirect way to assess both tumor activity and the role of the inflammatory pattern during pro- and antitumor responses.
Materials and Methods
We performed a prospective evaluation of 56 patients: 30 women without evidence of malignant disease and 26 women with EOC. The plasma quantification of cytokines, chemokines, and microparticles (MPs) was performed using flow cytometry.
Results
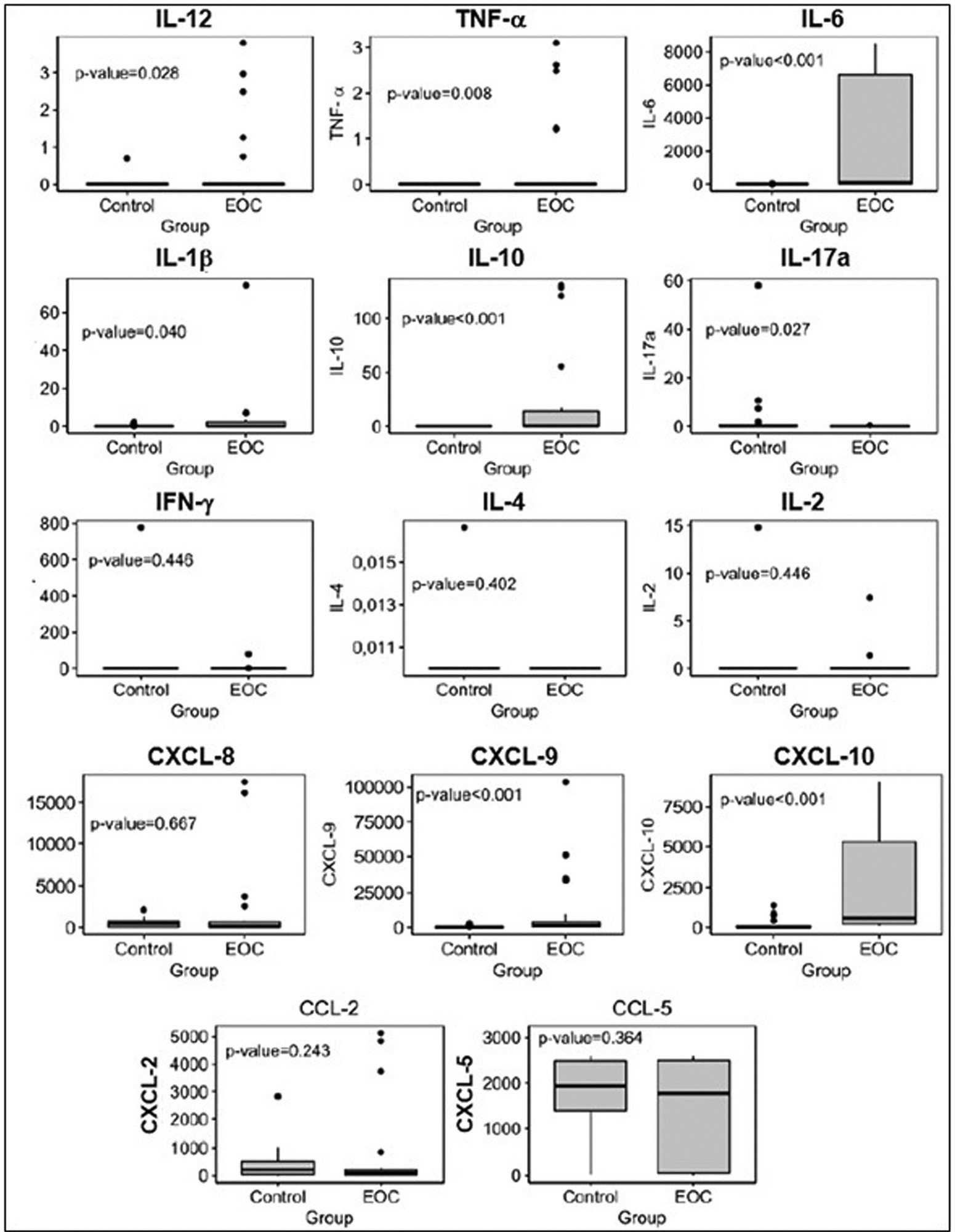
Plasma levels of proinflammatory cytokines interleukin-12 (IL12), interleukin-6 (IL-6), tumor necrosis factor alpha (TNF-α) interleukin-1 beta (IL-1β), and interleukin-10 (IL-10), and C-X-C motif chemokine ligand 9 (CXCL-9) and C-X-C motif chemokine ligand 10 (CXCL-10) were significantly higher in patients with EOC than in those in the control group. Plasma levels of cytokine interleukin-17A (IL-17A) and MPs derived from endothelial cells were lower in patients with EOC than in the control group. The frequency of leukocytes and MPs derived from endothelial cells was higher in type-2 tumors than in those without malignancy. We observed an expressive number of inflammatory/regulatory cytokines and chemokines in the cases of EOC, as well as negative and positive correlations involving them, which leads to a higher complexity of these networks.
Conclusion
The present study showed that, through the development of networks consisting of cytokines, chemokines, and MPs, there is a greater systemic inflammatory response in patients with EOC and a more complex correlation of these biomarkers in type-2 tumors.
-
Original Article
Association between Adverse Maternal Clinical Outcomes and Imbalance of Cytokines and Angiogenic Factors in Preterm Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):669-675
11-29-2021
Summary
Original ArticleAssociation between Adverse Maternal Clinical Outcomes and Imbalance of Cytokines and Angiogenic Factors in Preterm Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):669-675
11-29-2021Views121See moreAbstract
Objective
Preeclampsia (PE) is a pregnancy-specific syndrome characterized by abnormal levels of cytokines and angiogenic factors, playing a role in the disease development. The present study evaluated whether immunological markers are associated with the gestational age and with the disease severity in preeclamptic women.
Methods
Ninety-five women who developed PE were stratified for gestational age as preterm PE (< 37 weeks) and term PE (≥ 37 weeks of gestation) and compared for disease severity as well as plasma concentration of angiogenic factors and cytokines. The concentrations of placental growth factor (PlGF), vascular endothelial growth factor (VEGF), Fms-like soluble tyrosine kinase (sFlt-1) and soluble endoglin (sEng), as well as the cytokines, tumor necrosis factor-α (TNF-α) and interleukin 10 (IL-10), were determined by enzyme-linked immunosorbent assay (ELISA).
Results
The comparison between preeclamptic groups showed a higher percentage of severe cases in preterm PE (82.1%) than in term PE (35.9%). Similarly, the concentrations of TNF-α, sFlt-1, and sEng, as well as TNF-α/IL-10 and sFlt-1/PlGF ratios were significantly higher in the preterm PE group. In contrast, concentrations of PlGF, VEGF, and IL-10 were significantly lower in women with preterm PE. Negative correlations between TNF-α and IL-10 (r = 0.5232) and between PlGF and sFlt1 (r = 0.4158) were detected in the preterm PE.
Conclusion
In pregnant women with preterm PE, there is an imbalance between immunological markers, with the predominance of anti-angiogenic factors and TNF-α, associated with adverse maternal clinical outcomes.
-
Original Article
Negative Correlation between Placental Growth Factor and Endocan-1 in Women with Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):593-598
10-01-2018
Summary
Original ArticleNegative Correlation between Placental Growth Factor and Endocan-1 in Women with Preeclampsia
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):593-598
10-01-2018Views134See moreAbstract
Objective
To analyze endocan-1, a biomarker of vascular endothelial related pathologies, and the placental growth factor (PlGF), an angiogenic factor and a placental dysfunction marker in patients with preeclampsia (PE).
Methods
Case-control study conducted at Hospital São Lucas, in the city of Porto Alegre, Brazil. Endocan-1 and PlGF levels were quantified in the maternal plasma using the MagPlexTH-C microsphere system (MAGPIX System, Luminex, Austin, Texas, US) and evaluated through analysis of covariance (ANCOVA) and adjusted by body mass index (BMI), gestational age and maternal age. To estimate the difference between the groups, the mean ratio (MR) and the 95% confidence interval (95%CI) were calculated. The Pearson correlation test was used to establish any association between endocan-1 and PlGF levels. The null hypothesis was rejected when p < 0.05.
Results
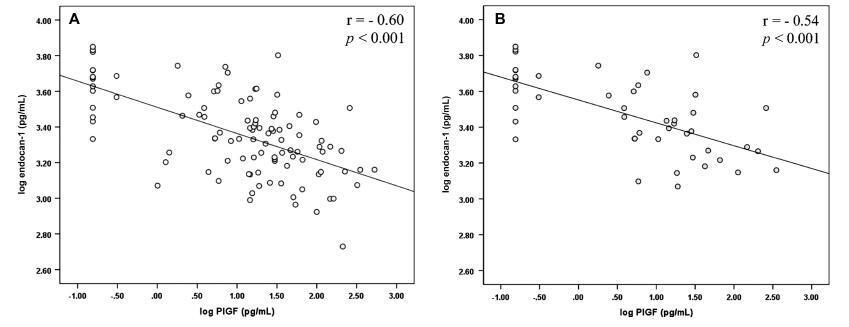
The group of patients was composed by normotensive (n = 67) patients and patients with PE (n = 50). A negative correlation between endocan-1 and the PlGF was noted in the entire normotensive group (linear correlation coefficient [r] = -0.605; p < 0.001), as well as in the PE group (r = -0.545; p < 0.001).
Conclusion
Endocan-1 levels are increased in patients with PE, and are inversely correlated with PlGF levels. We suggest that it is important to analyze angiogenic and proinflammatory molecules concomitantly in women with PE to better understand the pathophysiology of the disease. Both molecules are strong candidates for PE biomarkers, and future studies will examine any mechanisms connecting these factors in PE.
-
Artigos Originais
Local expression of tumor necrosis factor-alpha on premature rupture of membranes
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):249-253
07-29-2009
Summary
Artigos OriginaisLocal expression of tumor necrosis factor-alpha on premature rupture of membranes
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):249-253
07-29-2009DOI 10.1590/S0100-72032009000500008
Views80PURPOSE: to compare the expression of tumor necrosis factor-alpha (TNF-α) in ovular membranes with premature rupture (MPR) and with opportune rupture; to verify the association between the expression of the TNF-α in ovular membranes and the degree of chorioamnionitis, correlating the expression of the TNF-α and the membranes' time of rupture. METHODS: ovular membranes from 31 parturients with MPR, with gestational ages over 34 weeks, and from parturients with opportune membranes' rupture, with gestational ages equal or over 37 weeks. Chorioamnionitis detection has been done by histopathological analysis. The evaluation of the TNF-α expression has been done by immune-histochemical technique, using the labile streptavidin-biotin-peroxidase (LSAB) method. RESULTS: the average rupture time was 16.6 hours. The ratio of the TNF-α expression in the Control and Study Groups did not show a significant difference (χ2=6.6; p=0.08). In the Study Group, there was no correlation between the degree of chorioamnionitis and the intensity of TNF-α expression (Spearman's coefficient (Rs)=0.4; p=0.02). CONCLUSIONS: there was no significant difference between the TNF-α expression in ovular membranes with premature or opportune rupture; in the Study Group, there was significant association between TNF-α expression and the degree of chorioamnionitis, and there was no association between rupture time and the intensity of TNF-α expression.
Key-words ChorioamnionitisCytokinesFetal membranes, premature ruptureImmune systemPregnancyTumor necrosis factor-alphaSee more -
Artigo de Revisão
Effects of the menopause hormone therapy on the immune system
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(11):593-601
02-27-2007
Summary
Artigo de RevisãoEffects of the menopause hormone therapy on the immune system
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(11):593-601
02-27-2007DOI 10.1590/S0100-72032007001100008
Views63See moreThere is evidence that estrogen, progesterone and testosterone have modulatory effects over both cellular and humoral immune responses. These effects occur via immune-neuroendocrine interactions, involving the pituitary, gonadal steroids, thymic hormones, and the presence of specific receptors and messengers. These immune responses may be altered during pregnancy, gonadectomy, menopause and hormone therapy. Estrogen depresses the cellular immunity, suppresses the natural killer cell activity and increases the production of antibodies. Progesterone/progestogen suppresses the cellular immune system. Androgens, after metabolization in estrogens, might stimulate the humoral immune response. Hormone therapy is still broadly used in post-menopause women with the purpose of decreasing climacteric symptoms, as well as preventing genital atrophy and bone loss. Its use to attenuate the risk of cardiovascular and neurodegenerative diseases remains in debate. A few studies have been carried out to examine the effect of post-menopause hormone therapy on the immune system. There is evidence that the hypoestrogenic state, following menopause, could result in less resistance to infections. The present review examines the interaction between sexual steroids and the immune system and, based on epidemiological and clinical studies, evaluates the effects of hormone therapy on the immune responses. It was concluded that the hormone therapy normalizes the cellular immune response in post-menopausal women.
-
Artigo de Revisão
Periodontal disease and obstetrical complications: is there a risk relationship?
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(7):370-375
10-29-2007
Summary
Artigo de RevisãoPeriodontal disease and obstetrical complications: is there a risk relationship?
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(7):370-375
10-29-2007DOI 10.1590/S0100-72032007000700008
Views73Studies have shown possible risk relations among oral illnesses, mainly periodontal disease and adverse pregnancy outcomes, such as prematurity, low birth weight and preeclampsia. The explanation for this hypothesis is based on the fact that periodontal disease is an infectious state, which may increase maternal serum cytokines through the release of such agents directly from the periodontal pocket or by through the dissemination of pathogenic bacteria, inducing systemic production. This assumption is based on the knowledge that the physiopathology of the pregnancy complications cited above is associated with the presence of some cytokines in the maternal serum. The present study work has the objective to review literature in search of evidence to these alleged associations. Although a number of clinical studies have been found in this review, we noticed a lack of methodological standards, what limits the conclusions about this topic. On the other side, the fact that periodontal disease is not yet a confirmed risk factor for adverse pregnancy outcomes does not reduce the importance of oral health maintenance during pregnancy, since it is important to allow adequate feeding without pain and bleeding in order to maintain an adequate nutritional supply.
Key-words CytokinesOral healthPeriodontal diseasesPeriodontitisPregnancy complicationsPregnant womenRisk assessmentSee more -
Artigos Originais
Interleukin-10 production during pregnancy reduces HIV-1 replicaction in cultures of maternal lymphocytes
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):393-400
11-16-2005
Summary
Artigos OriginaisInterleukin-10 production during pregnancy reduces HIV-1 replicaction in cultures of maternal lymphocytes
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):393-400
11-16-2005DOI 10.1590/S0100-72032005000700005
Views149See morePURPOSE: to evaluate T cell proliferation and cytokine production in HIV-1-infected pregnant women and their impact on in vitro virus replication. METHODS: peripheral blood from 12 HIV-1-infected pregnant women and from their neonates was collected. As control, 10 samples from non-infected pregnants were also colleted. The CD4+ and CD8+ T cell counts were assayed by flow cytometry. Peripheral blood mononuclear cells (PBMC) and plasma were obtained by centrifugation with and without Ficoll-Hypaque gradient, respectively. The freshly purified PBMC were kept in cultures for seven days with PHA plus r-IL-2, and the lymphoproliferative response was assayed by Trypan blue dye exclusion. In some experiments we added anti-IL-10 monoclonal antibody. The plasma samples and supernatants from cell cultures were stored to determine both peripheral cytokine levels, by ELISA sandwich, and viral load, by RT-PCR. RESULTS: the results showed that the lymphoproliferative response was smaller in cultures obtained from HIV-1-infected women than in control cultures [4.2±0.37 vs 2.4±0.56 (x 10(6) cell/mL), p<0.005]. In both control and infected pregnant women who had low plasma viral load, the level of IL-10 was higher than in those with high viral replication (9.790±3.224 vs 1.256±350 pg/mL, p=0.002). The elevated TNF-alpha production detected in serum (7.200±2.440 pg/mL) and supernatants (21.350±15.230 pg/mL) was associated with higher plasma viral loads and vertical infection. The IL-10 blockade by anti-IL-10 antibodies augmented viral replication in the cell cultures. CONCLUSION: these results indicate that IL-10 production exerts a negative influence on virus replication, diminishing the probability of intrauterine HIV-1 infection.


