Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):847-852
01-12-2021
To compare the prevalence of urinary incontinence (UI) before and during the COVID-19 quarantine in CrossFit women and their relationship with training level.
A cross-sectional study was performed among 197 women practicing CrossFit. The inclusion criteria were nulliparous women, between 18 and 45 years old, who had trained, before quarantine, in accredited gyms. The exclusion criteria were not following the COVID-19 prevention protocols and having UI on other occasions than just sport. An online questionnaire was emailed containing questions about frequency, duration, and intensity of training and data related to the COVID-19 pandemic. The participants were invited to answer whether they were infected with COVID-19 and what treatment/recommendation they have followed. Whether UI stopped among participants, they were asked about the possible reasons why this happened. The training intensity was categorized as “the same,” “decreased” or “increased.”
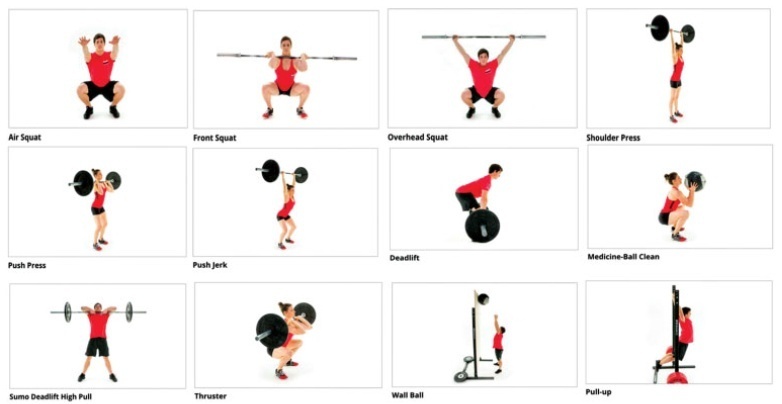
The mean age of the participants was 32 years old and most (98.5%) could practice CrossFit during the pandemic. There was a decrease in training intensity in 64% of the respondents. Exercises with their own body weight, such as air squat (98.2%), were the most performed. Urinary incontinence was reported by 32% of the participants before the COVID-19 pandemic, and by only 14% of them during the pandemic (odds ratio [OR]=0.32 [0.19-0.53]; p<0.01; univariate analysis). Practitioners reported that the reason possibly related to UI improvement was the reduction of training intensity and not performing doubleunder exercise.
The reduction in the intensity of CrossFit training during the COVID-19 quarantine decreased the prevalence of UI among female athletes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):169-174
04-01-2017
Vaginal pessary is used as a conservative treatment for pelvic organ prolapse (POP). Some studies have shown that common complaints of its use may include vaginal discomfort and increased vaginal discharge. Scant information is available about the microflora status after using this device.
To determine if the usage of vaginal pessary can interfere with the vaginal environment.
A cross-sectional study was performed from March of 2014 to July of 2015 including 90 women with POP. The study group was composed of 45 women users of vaginal pessary and 45 nom-users. All enrolled women answered a standardized questionnaire and were subjected to a gynecological exam to collect vaginal samples for microbiological evaluation under optic microscopy. Clinical and microbiological data were compared between study and control groups.
Vaginal discharge was confirmed in 84% of the study group versus 62.2% in the control group (p< 0.01); itching was reported in 20 and 2.2%, respectively (p< .05); genital ulcers were only found in the pessary group (20%). There was no difference with regard to the type of vaginal flora. Bacterial vaginosis was prevalent in the study group (31.1% study group versus 22.2% control group), (p=.34).
Women using vaginal pessaries for POP treatment presented more vaginal discharge, itching and genital ulcers than non-users.