Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):847-852
To compare the prevalence of urinary incontinence (UI) before and during the COVID-19 quarantine in CrossFit women and their relationship with training level.
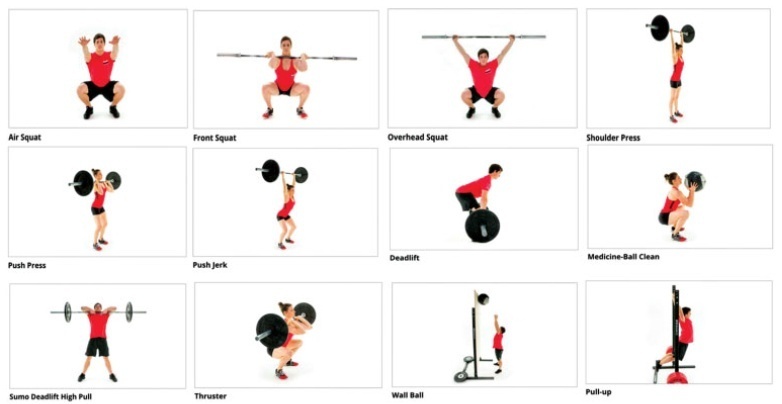
A cross-sectional study was performed among 197 women practicing CrossFit. The inclusion criteria were nulliparous women, between 18 and 45 years old, who had trained, before quarantine, in accredited gyms. The exclusion criteria were not following the COVID-19 prevention protocols and having UI on other occasions than just sport. An online questionnaire was emailed containing questions about frequency, duration, and intensity of training and data related to the COVID-19 pandemic. The participants were invited to answer whether they were infected with COVID-19 and what treatment/recommendation they have followed. Whether UI stopped among participants, they were asked about the possible reasons why this happened. The training intensity was categorized as “the same,” “decreased” or “increased.”
The mean age of the participants was 32 years old and most (98.5%) could practice CrossFit during the pandemic. There was a decrease in training intensity in 64% of the respondents. Exercises with their own body weight, such as air squat (98.2%), were the most performed. Urinary incontinence was reported by 32% of the participants before the COVID-19 pandemic, and by only 14% of them during the pandemic (odds ratio [OR]=0.32 [0.19-0.53]; p<0.01; univariate analysis). Practitioners reported that the reason possibly related to UI improvement was the reduction of training intensity and not performing doubleunder exercise.
The reduction in the intensity of CrossFit training during the COVID-19 quarantine decreased the prevalence of UI among female athletes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):765-774
To investigate depression and sexual function among pregnant and nonpregnant women throughout the COVID-19 pandemic.
A total of 188 women, 96 pregnant and 92 non-pregnant were included. The Beck Depression Inventory (BDI) and the Arizona Sexual Experience Scale (ASEX) were applied to the participants after obtaining sociodemographic data.
The depression scores of pregnant and non-pregnant women were similar (p = 0.846). We found that the depression scores were significantly higher among the group of participants who have lower economic status (p = 0.046). Moreover, the depression score was significantly higher among women who lost their income during the pandemic (p = 0.027). The score on the ASEX was significantly higher, and sexual dysfunction was more prevalent among women who have lower levels of schooling and income (p < 0.05). Likewise, the ASEX scores were significantly higher (p = 0.019) among the group who experienced greater income loss throughout the pandemic. Upon comparing the pregnant and non-pregnant groups, we detected that sexual dysfunction had a significantly higher rate among pregnant women (p < 0.001).
In times of global crisis, such as the current pandemic, low-income families have an increased risk of experiencing depression and sexual dysfunction. When we compared pregnant women with non-pregnant women, depression scores were similar, but pregnant women were at a 6.2 times higher risk of developing sexual dysfunction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):595-599
To describe the hematological changes, the platelet indices in particular, in pregnant women with coronavirus disease 2019 (COVID-19) compared to healthy pregnant women.
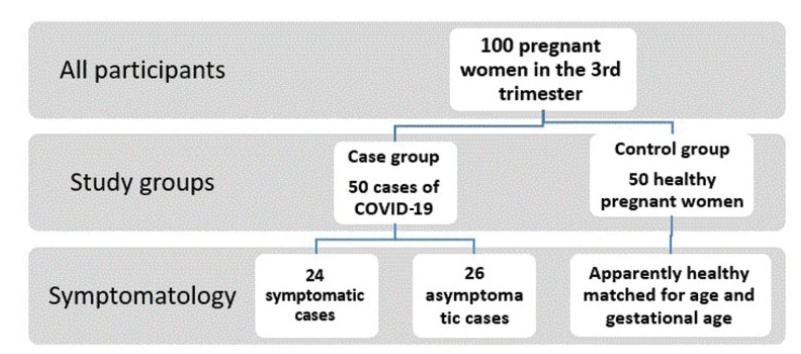
A retrospective case-control study conducted at the Al Yarmouk Teaching Hospital, in Baghdad, Iraq, involving 100 pregnant women, 50 with positive viral DNA for COVID-19 (case group), and 50 with negative results (control group); both groups were subjected to a thorough hematological evaluation.
Among the main hematological variables analyzed, the platelet indices, namely the mean platelet volume (MPV) and the platelet distribution width (PDW), showed statistically significant differences (MPV: 10.87±66.92 fL for the case group versus 9.84±1.2 fL for the control group; PDW: 14.82±3.18 fL for the case group versus 13.3±2.16 fL for the controls). The criterionvalue of the receiver operating characteristic (ROC) curve forPDWat a cutoffpoint of>11.8 fL showed a weak diagnostic marker, while the MPV at a cutoff value of>10.17 fL showed a good diagnostic marker.
The MPV and PDW are significantly affected by the this viral infection, even in asymptomatic confirmed cases, and we recommend that both parameters be included in the diagnostic panel of this infection.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(5):384-394
Coronavirus disease 2019 (COVID-19) is a disease caused by a newly discovered coronavirus, severe acute respiratory syndrome coronavirus 2 (SARSCoV-2), which usually leads to non-specific respiratory symptoms. Although pregnant women are considered at risk for respiratory infections by other viruses, such as SARS and Middle East respiratory syndrome (MERS), little is known about their vulnerability to SARS-CoV-2. Therefore, this study aims to identify and present the main studies on the topic, including the postpartum period.
In this narrative review, articles were searched in various databases, organizations, and health entities using keywords compatible with medical subject headings (MeSH), such as: COVID-19, pregnancy, vertical transmission, coronavirus 2019, and SARS-CoV-2.
The review of the scientific literature on the subject revealed that pregnant women with COVID-19 did not present clinical manifestations significantly different from those of non-pregnant women; however, there are contraindicated therapies. Regarding fetuses, studies were identified that reported that infection by SARS-CoV-2 in pregnant women can cause fetal distress, breathing difficulties and premature birth, but there is no substantial evidence of vertical transmission.
Due to the lack of adequate information and the limitations of the analyzed studies, it is necessary to provide detailed clinical data on pregnant women infected with SARS-CoV-2 and on the maternal-fetal repercussions caused by this infection. Thus, this review may contribute to expand the knowledge of professionals working in the area as well as to guide more advanced studies on the risk related to pregnant women and their newborns. Meanwhile, monitoring of confirmed or suspected pregnant women with COVID-19 is essential, including in the postpartum period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):474-479
Placental pathophysiology in SARS-CoV-2 infection can help researchers understand more about the infection and its impact on thematernal/neonatal outcomes. This brief review provides an overview about some aspects of the placental pathology in SARSCoV- 2 infection. In total, 11 papers were included. The current literature suggests that there are no specific histopathological characteristics in the placenta related to SARSCoV- 2 infection, but placentas frominfected women aremore likely to show findings of maternal and/or fetal malperfusion. The most common findings in placentas from infected women were fibrin deposition and intense recruitment of inflammatory infiltrates. The transplacental transmission of this virus is unlikely to occur, probably due to low expression of the receptor for SARS-CoV-2 in placental cell types. Further studies are needed to improve our knowledge about the interaction between the virus and the mother-fetus dyad and the impact on maternal and neonatal/fetal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):200-206
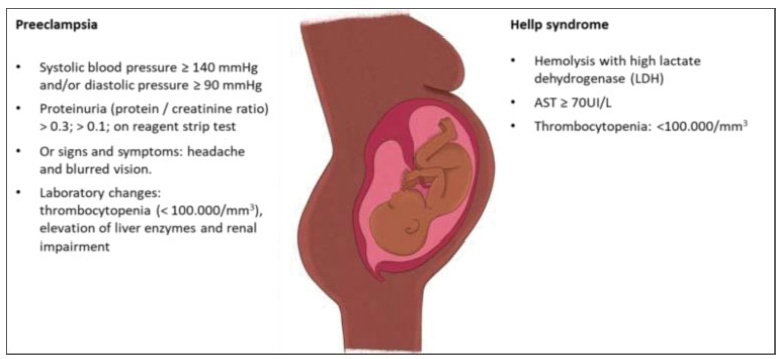
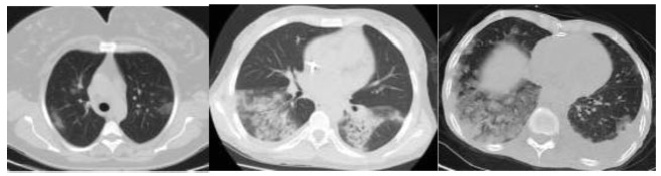
Covid-19 became a pandemic, and researchers have not been able to establish a treatment algorithm. The pregnant population is also another concern for health care professionals. There are physiological changes related to pregnancy that result in different laboratory levels, radiological findings and disease progression. The goal of the present article is to determine whether the laboratory results and radiological findings were different in non-pregnant women (NPWs) of reproductive age and pregnant women (PWs) diagnosed with the Covid-19 infection.
Out of 34 patients, 15 (44.11%) PWs and 19 (55.8%) NPWs were included in the study. Age, comorbidities, complaints, vitals, respiratory rates, computed tomography (CT) findings and stages, as well as laboratory parameters, were recorded from the hospital database.
Themean age of the PWs was of 27.6 ± 0.99 years, and that of the NPWs was of 37.63 ± 2.00; when agewas compared between the groups, a statistically significant difference (p=0.001) was found. The mean systolic blood pressure of the PWs was of 116.53 ± 11.35, and that of the NPWs was of 125.53 ± 13.00, and their difference was statistically significant (p=0.05). The difference in the minimum respiratory rates of the patients was also statistically significant (p=0.05). The platelet levels observed among the PWs with Covid-19 were lower than those of the NPWs (185.40 ± 39.09 x 109/mcL and 232.00 ± 71.04 x 109/mcL respectively; p=0.05). The mean D-dimer value of the PWs was lower in comparison to that of the NPWs (p<0.05).
The laboratory findings and imaging studiesmay differ between pregnant and non-pregnant populations. It is important to properly interpret these studies. Future studies with a higher number of patients are required to confirm these preliminary data.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(3):207-215
The evaluation of the available evidence on vertical transmission by severe acute respiratory syndrome coronavirus 2 (SARS-CoV)-2.
An electronic search was performed on June 13, 2020 on the Embase, PubMed and Scopus databases using the following search terms: (Coronavirus OR COVID-19 OR COVID19 OR SARS-CoV-2 OR SARS-CoV2 OR SARSCoV2) AND (vertical OR pregnancy OR fetal).
The electronic search resulted in a total of 2,073 records. Titles and abstracts were reviewed by two authors (WPM, IDESB), who checked for duplicates using the pre-established criteria for screening (studies published in English without limitation regarding the date or the status of the publication).
Data extraction was performed in a standardized way, and the final eligibility was assessed by reading the full text of the articles. We retrieved data regarding the delivery of the potential cases of vertical transmission, as well as themain findings and conclusions of systematic reviews.
The 2,073 records were reviewed; 1,000 duplicates and 896 clearly not eligible records were excluded. We evaluated the full text of 177 records, and identified only 9 suspected cases of possible vertical transmission. The only case with sufficient evidence of vertical transmission was reported in France.
The risk of vertical transmission by SARS-CoV-2 is probably very low. Despite several thousands of affected pregnant women, we have identified only one case that has fulfilled sufficient criteria to be confirmed as a case of vertical transmission. Well-designed observational studies evaluating large samples are still necessary to determine the risk of vertical transmission depending on the gestational age at infection.
