Summary
Revista Brasileira de Ginecologia e Obstetrícia. 09-18-2024;46:e-rbgo69
To compare the effectiveness and safety of non-mRNA versus mRNA COVID-19 vaccines on pregnant women and their newborns in a systematic review with meta-analysis.
We searched PubMed, Embase, and Cochrane Central in May 2023.
The search strategy yielded 4451 results, 16 studies were fully reviewed. We selected case-control studies analysing non-mRNA versus mRNA vaccines. Data collection and analysis: we assessed the risk of bias using the Cochrane Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool. Standardised mean differences were pooled using random-effect models.
We identified 8 prospective and retrospective studies with a total of 32,153 patients. Non-mRNA vaccines were associated with a higher incidence of fever (OR 2.67; 95% CI 2.08-3.43; p<0.001), and a lower incidence of fetal or neonatal death (OR 0.16; 95% CI 0.08-0.33; p<0.001). In subgroup analyses, the Jansen vaccine (Ad26.COV2.S) was found to have a higher rate of premature labor/delivery (OR 4.48; 95% CI 1.45-13.83; p=0.009) and missed/spontaneous abortion (OR 1.90; 95% CI 1.09-3.30; p=0.02), as compared with the Pfizer (BNT162b2) vaccine.
non-mRNA vaccines are associated with a lower incidence of fetal or neonatal death among pregnant women who receive a Covid19 vaccine, although at an increased rate of pyrexia compared with mRNA vaccines. Other studies are required for better assessment.
CRD42023421814
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 06-27-2024;46:e-rbgo52
To analyze the death of Brazilian pregnant and postpartum women due to COVID-19 or unspecific cause.
This is retrospective, descriptive-exploratory, population-based study carried out with the Sistema de Informação de Vigilância Epidemiológica da Gripe (SIVEP-Gripe) database, with pregnant and postpartum women of reproductive age who died from confirmed COVID-19 between 2020 and 2021. The chosen variables were: age, gestational period, type and number of comorbidities, skin color, using the statistical software R Foundation for Statistical Computing Platform, version 4.0.3 and Statistical Package for Social Science, version 29.0 for analysis.
A total of 19,333 cases of pregnant and postpartum women aged between 10 and 55 years diagnosed with SARS were identified, whether due to confirmed COVID-19 or unspecific causes. Of these, 1,279 died, these cases were classified into two groups according to the cause of death: deaths from COVID-19 (n= 1,026) and deaths from SARS of unspecific cause (n= 253).
The risk of death increased among black and brown women, in the postpartum period and with the presence of comorbidities, mainly diabetes, cardiovascular diseases and obesity. The data presented here draw attention to the number of deaths from SARS, especially among sociodemographic profiles, precarious access to health, such as the black population. In addition, limitations in adequate access to health care are reinforced by even lower rates of ICU admissions among women who died from SARS of an unspecified cause.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 01-27-2024;46:e-rbgo3
The aims of the study are to describe the association of coronavirus disease (COVID-19) with the abnormal histopathological findings in human placenta and to highlight the potential predictors of these histopathological findings.
A retrospective cohort study, held in two obstetric units from January 2021- 2022, 34 patients who were confirmed cases of COVID- 19 were followed up till the time of delivery as their placenta were sent for histopathology. Patients diagnosed with other viral infections, chorioamnionitis, or were known case of as pre-term or term pre labour rupture of membrans (PROM) were excluded as well as pre exisiting diabetes mellitus or pre-eclampsia. Data analysis were performed using STATA software version 16.
Specific histopatological findings (fetal vascular malperfusion, maternal vascular malperfusion, inflammatory pathology and thrombotic finding) were significantly high among 13 (38.2%) of the study group who got infected earlier in pregnancy (P<0.001). The period between the diagnosis of COVID-19 and the delivery significantly increases the odds of the presence of pathological findings by 2.75 times for each week the patients getting infected earlier.
Association of abnormal placental histopathological findings with COVID-19 infection in pregnancy and the potential predictor for the occurrence of placental findings is the longer duration between the diagnosis of the infection and the delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 01-24-2022;43(12):949-960
To analyze the clinical and obstetric aspects of pregnant women with COVID-19.
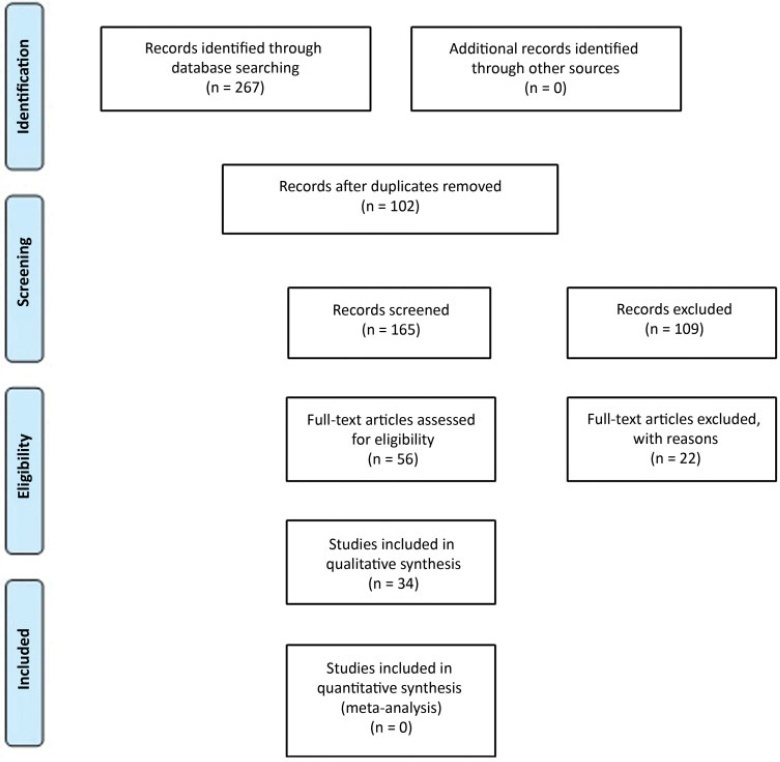
A systematic literature review in the MEDLINE/PubMed, LILACS, SCIELO, and CNKI databases was performed from March to May 2020, with the descriptors: Pregnancy; 2019-nCov; Coronavirus; SARS-Cov-2, Covid-19. Of those chosen were original titles, without language and period restriction and that addressed pregnant women with a clinical and/or laboratory diagnosis of COVID-19. Revisions, editorials, and duplicate titles were excluded. The Newcastle-Ottawa (NOS) and Murad et al. scales were used to assess the quality of the studies.
We included 34 articles with 412 pregnant women infected with severe acute respiratory syndrome (SARS-Cov-2), with an average age of 27.5 years of age and 36.0 gestational weeks. The most common symptom was fever (205 [49.7%]), and 89 (21.6%) pregnant women progressed to severe viral pneumonia. Laboratory tests showed an increase in C-reactive protein (154 [37.8%]), and radiological tests showed pneumonia with peripheral ground-glass pattern (172 [51.4%]). Emergency cesarean delivery was indicated for most pregnant women, and the most common gestational complication was premature rupture of ovarian membranes (14 [3.4%;]). We detected 2 (0.5%) neonatal deaths, 2 (0.5%) stillbirths, and 1 (0.2%) maternal death.
Pregnant women with COVID-19 presented a clinical picture similar to that of non-infected pregnant women, with few obstetric or neonatal repercussions. There was a greater indication of cesarean deliveries before the disease aggravated, and there was no evidence of vertical transmission of the infection.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 12-21-2020;42(10):669-671
The present report describes the case of a 31-year-old primigravida, with dichorionic twins at 31 weeks. She presented with history of myalgia, jaundice, and abdominal discomfort. No flu-like symptoms as fever or cough. She was not aware of exposure to COVID-19. Normal blood pressure and O2 saturation. Laboratory tests showed platelet count of 218,000 mm3, alanine aminotransferase (ALT) 558 IU and serum creatinine 2.3 mg/dl. Doppler ultrasound in one twin was compatible with brain sparing. Partial hemolysis, elevated liver enzymes, low platelet count (HELLP) syndrome was the hypothesis, and a cesarean section was performed. On day 2, the white-cell count reached 33,730, with decreased consciousness and mild respiratory distress. Tomography revealed both lungs with ground-glass opacities. Swab for COVID-19 polymerase chain reaction (PCR) was positive. Thrombocytopenia in patients with COVID-19 appears to be multifactorial, similar to what occurs in preeclampsia and HELLP syndrome. We assume that the synergism of these pathophysiological mechanisms could accelerate the compromise of maternal conditions and could be a warning to the obstetric practice.