Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(5):255-265
06-22-2020
The optimal use of contraceptive methods requires that women participate in targeted choice of methods that meet their individual needs and expectations. The Thinking About Needs in Contraception (TANCO) study is a quantitative online survey of the views of health professionals and women on aspects of contraceptive counseling and contraceptive use.
Physicians and women attending clinics for contraception were invited to complete online questionnaires. The research explored the knowledge and use of contraceptive methods, satisfaction with the current method and interest in receiving more information on all methods. Aspects related to contraceptive practice among physicians were gathered in parallel. The results obtained in the Brazilian research were compared with those of the European research, which involved 11 countries.
There was a high prevalence of contraceptive use and general satisfaction with the current method. A total of 63% of the women were using short-acting contraceptive (SAC) methods, and 9% were using a long-acting reversible contraceptive (LARC). Sixty-six percent of women were interested in receiving more information on all methods; 69% of women said they would consider LARC if they received more comprehensive information about it. Health professionals tend to underestimate the interest of women in receiving information about contraception in general, and more specifically about LARCs.
Despite the high levels of use and satisfaction with the current methods, women were interested in receiving more information on all contraceptive methods. Structured contraceptive counseling based on individual needs and expectations may lead to greater knowledge and a greater likelihood of proper contraceptive choice.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):607-612
11-07-2019
Almost 80% of adolescent pregnancies are unplanned, and between 28 and 63% of adolescent mothers had a repeated pregnancy within 18 months. Among girls with repeated pregnancies, two-thirds reported that the pregnancy was unplanned. We aim to assess contraceptive use by adolescent mothers with increasing choice for long-acting reversible contraception (LARC) methods in postpartum consultation after a semistructured group intervention involving adolescent mothers.
Retrospective observational study conducted at the Universidade Estadual de Campinas, Campinas, state of São Paulo, Brazil, involving new antenatal and postpartum education groups for adolescents. At postpartum consultations, the adolescents chose their contraceptive. The datawas compared with previous series followed in a period before the implementation of the education group - a historical control group.
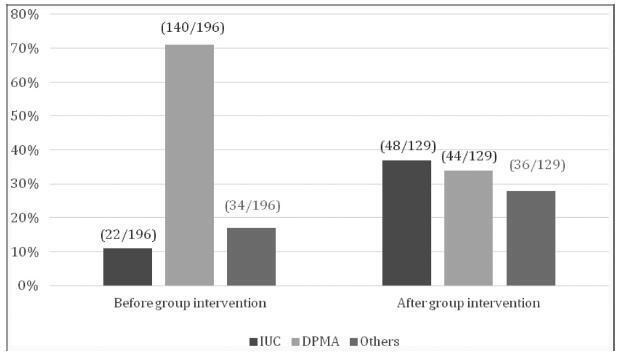
We included 129 adolescent after childbirth from January 1st, 2015 through July 31st, 2017. Out of this total, 63% had ever used contraceptive methods before pregnancy, and the most frequent method was combined oral contraceptives (33%) followed by condoms (21%). At the first postpartum consultation, the most common contraceptive chosen was intrauterine contraception (IUC) (37.2%) and depot-medroxyprogesterone acetate (DMPA) (34.1%).When comparing the rates before and after the education interventions, there was a 3-fold increase in the use of IUCs.
Antenatal and postpartum education have shown a significant increase in the choice for LARC methods among adolescent mothers, with very high acceptability after a period using the method. The educational groups performed during the antenatal care and beyond the gestational period are easy to be applied worldwide with low dependence on funding.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):236-241
06-19-2019
To compare sexual function and quality of life (QOL) among intrauterine contraceptive (copper-intrauterine device [Cu-IUD] or the 52-mg 20 μg/day levonorgestrel- releasing intrauterine system [LNG-IUS]) users.
This was part of a cross-sectional study. Women aged between 18 and 49 years old, in a heterosexual relationship, reporting sexual intercourse in the previous 4 weeks, using Cu-IUD (Group 1) or LNG-IUS (Group 2) responded to a questionnaire with sociodemographic information, to the Female Sexual Function Index (FSFI), to the World Health Organization QOL Questionnaire Abbreviated Version (WHOQOL-BREF), and to a questionnaire about the contraceptive method used. The Student t-test, the Pearson χ2 test or the Fisher exact test, and the Mann-Whitney test were used for the analysis. For the adjusted comparison, we have used the analysis of covariance (ANCOVA). A multiple regression analyzing factors related to FSFI 26.55 was done. Significance was established at p < 0.05.
A total of 347 women in Group 1 (mean age of 32.3 ± 7.5 years old) and of 298 in Group 2 (mean age of 32.7 ± 6.4 years old) completed the questionnaires.Most women had ≥ 8 years of schooling, were in amonogamous relationship, and had had ≤ 2 pregnancies. A total of 122 Cu-IUD and of 87 LNG-IUS users scored ≤ 26.55 on the FSFI. Significant lower scores in physical, environmental, and overall QOL domains in the WHOQOL-BREF questionnaire were found in Group 1. More women using the Cu- IUD were not satisfied with the method.
We did not find significant differences in sexual function; there was a lower score in some domains of QOL among women who used the Cu-IUD. It was not possible to ensure that those differences were related to the contraceptive method.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):437-443
08-01-2018
To evaluate the social, obstetric and psychological risk factors related to repeat pregnancy in teenagers.
A case control study conducted at Centro de Atenção à Saúde Integral da Mulher (Caism, in the Portuguese acronym), in Campinas, Brazil, from 2015 to 2017. Three groups were selected: a case-group of adolescents who had repeat pregnancy and two control-groups, one consisting of adolescents who had delivered at first time and another one of adult women with more than one deliveries. Participants were asked about habits, socio-demographics characteristics, reproductive and obstetric history and assessed psychological issues.
Ninety women were enrolled, 30 in each study group. Adolescents with repeat pregnancy have lower self-esteem scores and more ineffective contraceptive use. When compared with teens at first delivery, they had less schooling level (odds ratio [OR] 4.03 [1.37-11.8]), more school abandon (OR 8.16 [2.36-28.2]) and drugs use (OR 4.97[1.39-17.8]). Non-white skin color (OR 6.2 [1.15-41.0]), drugs use (OR 17.5 [2.62-116.6]) and first sexual intercourse under 15y (OR 18.0[2.82-115.0]) were found as higher risk factors for repeat pregnancy when comparing adolescents and adults.Moreover, adolescents withmore than one gestation had lower self-esteem and greater susceptibility to unplanned pregnancy.
There was an association between repeat pregnancy among adolescents and lower education, early onset of sexual activity, non-white skin color, low use of contraception and increased use of drugs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):397-402
08-01-2017
To describe the reproductive variables associated with different sickle cell disease (SCD) genotypes and the influence of contraceptive methods on acute painful episodes among the women with the homozygous hemoglobin S (HbSS) genotype.
A cross-sectional study was conducted between September of 2015 and April of 2016 on 158 women afflicted with SCD admitted to a hematology center in the Northeast of Brazil. The reproduction-associated variables of different SCD genotypes were assessed using the analysis of variance (ANOVA) test to compare means, and the Kruskal-Wallis test to compare medians. The association between the contraceptive method and the acute painful episodes was evaluated by the Chi-square test.
Themean age of women with SCD was 28.3 years and 86.6% were mixed or of African-American ethnicity. With respect to the genotypes, 134 women (84.8%) had HbSS genotype, 12 women (7.6%) had hemoglobin SC (HbSC) disease genotype, and 12 (7.6%) were identified with hemoglobinopathy S-beta (S-β) thalassemia. The mean age of HbSS diagnosis was lower than that of HbSC disease, the less severe formof SCD (p < 0.001). The mean age ofmenarche was 14.8 ± 1.8 years for HbSS and 12.7 ± 1.5 years for HbSC (p < 0.001). Among women with HbSS who used progestin-only contraception, 16.6% had more than 4 acute painful episodes per year. There was no statistically significant difference when compared with other contraceptive methods.
With respect to reproduction-associated variables, only the age of the menarche showed delay in HbSS when compared with HbSC. The contraceptive method used was not associated with the frequency of acute painful episodes among the HbSS women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(6):294-308
06-01-2017
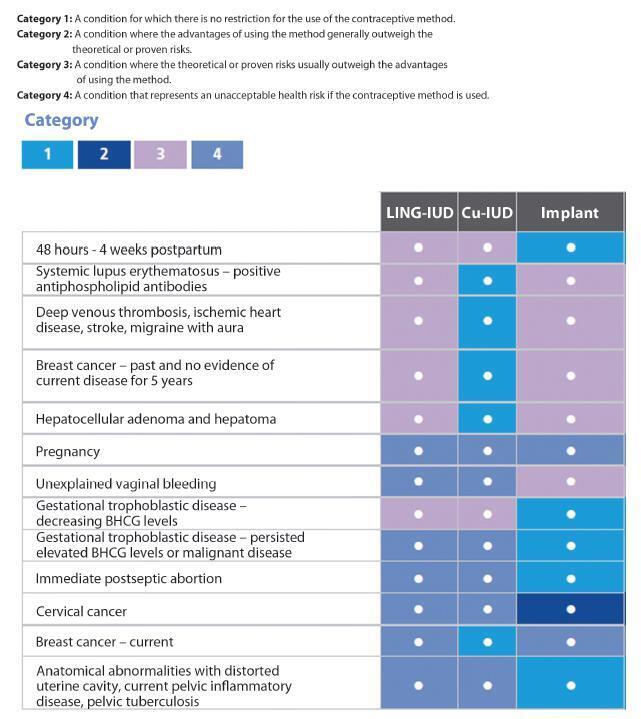
Unwanted pregnancy is a major public health problem both in developed and developing countries. Although the reduction in the rates of these pregnancies requires multifactorial approaches, increasing access to long-acting contraceptive methods can contribute significantly to change this scenario. In Brazil, gynecologists and obstetricians play a key role in contraceptive counseling, being decisive in the choice of long-acting reversible methods, characterized by intrauterine devices (IUDs) and the contraceptive implant. The vast scope due to the reduced number of situations to indicate long-acting methods should be emphasized in routine contraceptive counseling. On the other hand, gynecologists and obstetricians should adapt the techniques of insertion of long-acting methods, and engage in facilitating conditions to access these contraceptives through public and private health systems in Brazil. This study is part of a project called Diretrizes e Recomendações FEBRASGO (Guidelines and Recommendations of the FEBRASGO - Brazilian Federation of Gynecology and Obstetrics Associations from the Portuguese acronym). It aims to review the main characteristics of long-acting contraceptives and critically consider the current situation and future prospects to improve access to these methods, proposing practical recommendations of interest in the routine of gynecologists and obstetricians.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):545-551
11-01-2016
To determine methods of contraception used by adolescents before and after pregnancy.
A cross-sectional study was performed, and data were collected from medical records of all teens in puerperal consultation at the Hospital da Mulher - José Aristodemo Pinotti (Caism), Universidade Estadual de Campinas (CAISM), São Paulo, Brazil, between July 2011 and September 2013. The inclusion criterionwas being 10 to 19 years old, and the exclusion criterion was having a first consultation 90 days after childbirth. Statistical analyseswere performed with averages, standard deviations, percentages, correlations and Fisher's exact tests using the SAS program, version 9.4.
A total of 196 adolescents in postpartum consultation were included (44 days after childbirth on average). The majority was older than 14 years (89%), with an average age of 16.2 years, and the most were exclusively breast-feeding (70%). Before pregnancy, the use of any contraceptive methods was mentioned by 74% adolescents; the most frequent use was combined oral contraceptive followed by condom. The main reason for abandoning the use of contraception was the occurrence of an unintended pregnancy (41%), followed by reports of side effects (22%), behavior issues (18%) and desire for pregnancy (16%). A positive correlation was found between the age of the adolescent at the moment of childbirth, the age of menarche (r = 0.3), and the first sexual intercourse (r = 0.419). Vaginal delivery occurred in 76% of the cases. After birth, depot medroxyprogesterone acetate (DMPA) was the contraception method most frequently used (71%), followed by oral contraceptives (11.8%) and intrauterine devices (IUDs, 11.2%).
The most prescribed contraceptive method before pregnancy in adolescents who had childbirth was combined oral contraceptives. Many of the study participants had an unintended pregnancy. After childbirth, the most used contraceptive method was DMPA. To improve contraception and reduce the chance of unintended pregnancies among adolescents, we should promote the use of long-acting reversible contraceptives (LARCS).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):132-139
03-01-2016
To evaluate the compliance and degree of satisfaction of nulligravida (has not given birth) and parous (had already given birth) women who are using intrauterine devices (IUDs).
A cross-sectional cohort study was conducted comparing nulligravida and parous women who had had an IUD inserted between July 2009 and November 2011. A total of 84 nulligravida women and 73 parous women were included. Interviews were conducted with women who agreed to participate through telephone contact. Statistical analysis was performed with Student s t-test and Mann-Whitney test for numeric variables; Pearson s chi-square test to test associations; and, whenever pertinent, Fisher s exact test for categorical variables. A survival curve was constructed to estimate the likelihood of each woman continuing the use of the IUD. A significance level of 5% was established.
When compared with parous women, nulligravida women had a higher education level (median: 12 vs. 10 years). No statistically significant differences were found between the nulligravida and parous women with respect to information on the use of the IUD, prior use of other contraceptive methods, the reason for having chosen the IUD as the current contraceptive method, reasons for discontinuing the use and adverse effects, compliance, and degree of satisfaction. The two groups did not show any difference in terms of continued use of the IUD (p = 0.4).
There was no difference in compliance or the degree of satisfaction or continued use of IUDs between nulligravida and parous women, suggesting that IUD use may be recommended for women who have never been pregnant.