-
Original Article01-24-2021
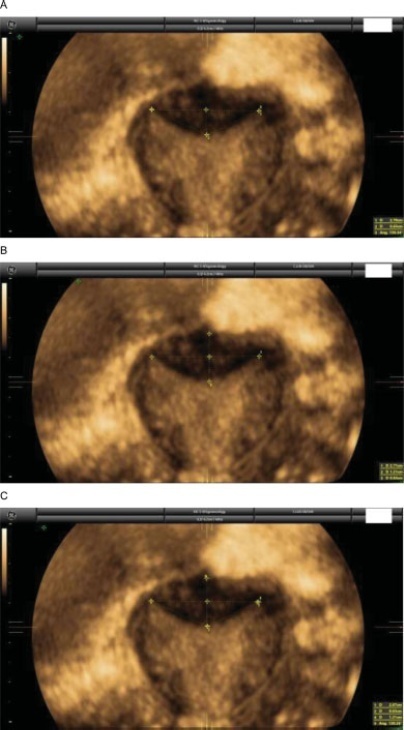
Diagnosing Septate Uterus Using Three-Dimensional Ultrasound Using Three Different Classifications: An Interobserver and Intraobserver Agreement Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):911-918
Abstract
Original ArticleDiagnosing Septate Uterus Using Three-Dimensional Ultrasound Using Three Different Classifications: An Interobserver and Intraobserver Agreement Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):911-918
Views223See moreAbstract
Objective
Currently, there are up to three different classifications for diagnosing septate uterus. The interobserver agreement among them has been poorly assessed.
Methods
A total of 50 three-dimensional (3D) volumes of a nonconsecutive series of women with suspected uterine malformation were used. Two nonexpert examiners evaluated a single 3D volume of the uterus of each woman, blinded to each other. The following measurements were performed: indentation depth, indentation angle, uterine fundal wall thickness, external fundal indentation, and indentation-to-wall-thickness (I:WT) ratio. Each observer had to assign a diagnosis in each case, according to the three classification systems (ESHRE/ESGE, ASRM, and CUME). The interobserver agreement regarding the ESHRE/ESGE, ASRM, and CUME classifications was assessed using the Cohen weighted kappa index (k). Agreement regarding the three classifications (ASRM versus ESHRE/ESGE, ASRM versus CUME, ESHRE/ESGE versus CUME) was also assessed.
Results
The interobserver agreement between the 2 nonexpert examiners was good for the ESHRE/ESGE (k = 0.74; 95% confidence interval [CI]: 0.55–0.92) and very good for the ASRM and CUME classification systems (k = 0.95; 95%CI: 0.86–1.00; and k = 0.91; 95%CI: 0.79–1.00, respectively). Agreement between the ESHRE/ESGE and ASRM classifications was moderate for both examiners. Agreement between the ESHRE/ESGE and CUME classifications was moderate for examiner 1 and good for examiner 2. Agreement between the ASRM and CUME classifications was good for both examiners.
Conclusion
The three classifications have good (ESHRE/ESGE) or very good (ASRM and CUME) interobserver agreement. Agreement between the ASRM and CUME classifications was higher than that for the ESHRE/ESGE and ASRM and ESHRE/ESGE and CUME classifications.
-
Original Article07-01-2016
Epidemiological Risk Factors and Perinatal Outcomes of Congenital Anomalies
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):348-355
Abstract
Original ArticleEpidemiological Risk Factors and Perinatal Outcomes of Congenital Anomalies
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):348-355
Views268See moreAbstract
Objectives
To identify the epidemiological risk factors for congenital anomalies (CAs) and the impact of these fetal malformations on the perinatal outcomes.
Methods
This prospective cohort study comprised 275 women whose fetuses had CAs. Maternal variables to establish potential risk factors for each group of CA and perinatal outcomes were evaluated. The primary outcome was CA. Secondary outcomes included: fetal growth restriction (FGR); fetal distress (FD); premature rupture of membranes (PROM); oligohydramnios or polyhydramnios; preterm delivery (PTD); stillbirth; cesarean section; low birth weight; Apgar score < 7 at the 1st and 5th minutes; need for assisted ventilation at birth; neonatal infection; need for surgical treatment; early neonatal death; and hospitalization time. Chi-square (x2) test and multilevel regression analysis were applied to compare the groups and determine the effects of maternal characteristics on the incidence of CAs.
Results
The general prevalence of CAs was of 2.4%. Several maternal characteristics were associated to CAs, such as: age; skin color; level of education; parity; folic acid supplementation; tobacco use; and history of previous miscarriage. There were no significant differences among the CA groups in relation to FGR, FD, PROM, 1-minute Apgar score > 7, and need for assisted ventilation at birth. On the other hand, the prevalence of the other considered outcomes varied significantly among groups. Preterm delivery was significantly more frequent in gastrointestinal tract/abdominal wall defects. The stillbirth rate was increased in all CAs, mainly in isolated fetal hydrops (odds ratio [OR]: 27.13; 95% confidence interval [95%CI]: 2.90-253.47). Hospitalization time was higher for the urinary tract and congenital heart disease groups (p < 0.01). Neonatal death was significantly less frequent in the central nervous system anomalies group.
Conclusion
It was possible to identify several risk factors for CAs. Adverse perinatal outcomes were presented in all CA groups, and may differ according to the type of CA considered.


