Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):442-448
DOI 10.1590/SO100-720320140004941
To identify obstetric and perinatal factors associated with perinatal morbidity and mortality in pregnancies that progressed with ruptured membranes.
A cross-sectional hospital-based study with secondary data from records of patients (n=87) that evolved with the premature rupture of membranes between 24 and 42 weeks of gestation, admitted from January to April 2013 to a public hospital in Acre State, North of Brazil. Data were subjected to bivariate analysis for selection of variables to be used in a multiple regression model according to Poisson logistic regression with robust error.
The prevalence of perinatal morbidity-mortality was 51.4%, including a 2.3% death rate (2 cases) and a 9.2% fetal neonatal death rate (8 cases). The variables associated with mortality in the final multiple model were: number of prenatal consultations ≥6, with a prevalence ratio (PR) of 0.5 and a 95% confidence interval (95%CI) of 0.3-0.9, gestational age ≥30 weeks (PR=0.6; 95%CI 0.4-0.8), low birth weight (PR=2.9; 95%CI 1.5-5.4), and mechanical ventilation (PR=3.8; 95%CI 2.0-7.2).
Perinatal morbidity and mortality were high among cases of ruptured membranes. Morbidity and mortality were associated with factors such as fewer prenatal visits, extreme prematurity and low birth weight in this group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(7):296-302
DOI 10.1590/SO100-720320140004958
To describe the perinatal outcomes after preterm premature rupture of membranes.
A retrospective cohort study was carried out at Instituto de Medicina Integral Prof. Fernando Figueira - IMIP from January 2008 to December 2012. A total of 124 preterm premature rupture of membranes singleton pregnancies, with gestational age <35, were included in the study. Pregnant women carrying fetuses with malformations, hypertensive syndromes, diabetes, or diagnosis of infections at admission were excluded. The pregnant women were hospitalized for conservative treatment with corticosteroids, antibiotics and tocolysis with nifedipine if necessary. The results are reported as frequency distributions and measures of central tendency and dispersion.
Seventeen patients (13.7%) had a gestational age of less than 24 weeks. Mean maternal age was 25.7 years, mean gestational age at the diagnosis of preterm premature rupture of membranes was 29 weeks, mean amniotic fluid index was 3.5 cm, and mean latency period was 10.5 days. Most patients went into spontaneous labor by the 30th week of pregnancy, and the rate of vaginal delivery was 88.2%. Chorioamnionitis was the most frequent maternal complication (34.7%). Neonatal sepsis was observed in 12% of patients, and the perinatal mortality rate was 21.5% for the group at or beyond the 24th week of gestation and 76.5% for the group with less than 24 weeks of gestational age.
A low maternal mortality rate was observed in preterm premature rupture of membranes; however, high rates of complications and perinatal death were observed, suggesting that other conduct protocols should be studied.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(4):146-151
DOI 10.1590/S0100-720320140050.0003
To describe the potential influence of amniotic fluid on the maternal outcome of preterm premature rupture of membranes (PROM).
An observational, retrospective cohort study was conducted between December 2012 and January 2008 on 86 pregnant women with preterm PROM and a gestational age (GA) of 24 to 35 weeks. The amniotic fluid index (AFI) was used to measure aminiotic fluid volume. Pregnant women were compared at two cut-off points: those with AFI <5.0 and ≥5.0 cm and AFI <3.0 and ≥3.0 cm. We excluded women with hypertensive disorders, diabetesmellitus, fetal malformations and a diagnosis of infections at admission. For statistical analysis, we used the χ2test or Fisher's exact test, when appropriate, and simple linear regression analysis, with the level of significance set at 5%. We calculated the Risk Ratio (RR) and its 95% confidence interval (95%CI).
When maternal outcomes were assessed by comparing ILA ≥5.0versus <5.0 cm, no significant differences were detected. However, when considering ILA <3.0 and ≥3.0 cm, there was an increased risk of chorioamnionitis (36.7 versus10.7%, RR: 3.4, 95%CI 1.4 -8.3, p=0.004), with no significant differences for the other variables. There was also a statistically significant positive correlation between AFI and gestational age at delivery (R2=0.78, p<0.0001).
AFI <3.0 cm causes a three-fold increase in the risk for chorioamnionitis; also, the higher the ILA, the higher the gestational age at delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(4):153-157
DOI 10.1590/S0100-72032012000400003
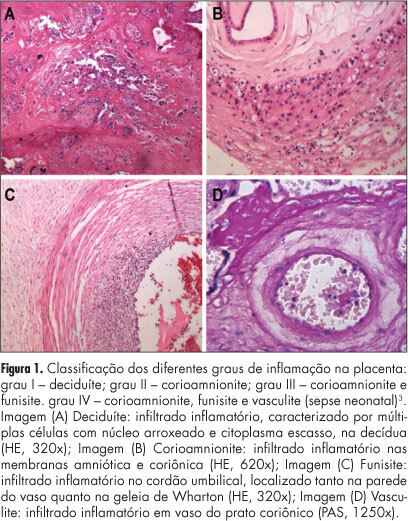
PURPOSE: To evaluate the influence of maternal complications, prematurity, fetal anthropometric parameters and conditions of the newborn on different degrees of chorioamnionitis. METHODS: We analyzed 90 placentas from deliveries performed at the General Hospital of Triângulo Mineiro Federal University with a diagnosis of inflammation in the anatomopathological exams. We reviewed the medical records to obtain relevant maternal and fetal information. The infections were classified as grade I - deciduitis; grade II - chorioamnionitis; grade III - chorioamnionitis and vasculitis; grade IV - neonatal sepsis and grade V - fetal death and pneumonitis. RESULTS: Among the pregnant women analyzed, 50.0% had no complications, 15.0% had ruptured membranes, 15.0% urinary tract infection, 7.5% hypertensive disorders, 7.5% transvaginal infection, 5.0% hematogenous infection, and 11.1% other complications. More than a half the neonates were males and 72.2% were born at term. Analysis of the degree of chorioamnionitis showed that 56.7% had grade I, 22.2% grade II, 4.4% grade III, 10.0% grade IV, and 6.7% grade V. Data were analyzed statistically by the Χ2 test for qualitative variables and by the Spearman test for correlation analysis. The higher grades of chorioamnionitis were observed in cases of maternal complications. We observed negative correlations between all parameters and the degree of fetal chorioamnionitis, which were significant regarding weight, length, thoracic circumference and Apgar score in the first and fifth minutes. CONCLUSIONS: The different patterns of chorioamnionitis were related to different maternal and fetal clinical features, affecting the life conditions of the newborn and the severity of morphological lesions found in stillbirths.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(5):249-253
DOI 10.1590/S0100-72032009000500008
PURPOSE: to compare the expression of tumor necrosis factor-alpha (TNF-α) in ovular membranes with premature rupture (MPR) and with opportune rupture; to verify the association between the expression of the TNF-α in ovular membranes and the degree of chorioamnionitis, correlating the expression of the TNF-α and the membranes' time of rupture. METHODS: ovular membranes from 31 parturients with MPR, with gestational ages over 34 weeks, and from parturients with opportune membranes' rupture, with gestational ages equal or over 37 weeks. Chorioamnionitis detection has been done by histopathological analysis. The evaluation of the TNF-α expression has been done by immune-histochemical technique, using the labile streptavidin-biotin-peroxidase (LSAB) method. RESULTS: the average rupture time was 16.6 hours. The ratio of the TNF-α expression in the Control and Study Groups did not show a significant difference (χ2=6.6; p=0.08). In the Study Group, there was no correlation between the degree of chorioamnionitis and the intensity of TNF-α expression (Spearman's coefficient (Rs)=0.4; p=0.02). CONCLUSIONS: there was no significant difference between the TNF-α expression in ovular membranes with premature or opportune rupture; in the Study Group, there was significant association between TNF-α expression and the degree of chorioamnionitis, and there was no association between rupture time and the intensity of TNF-α expression.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(4):175-180
DOI 10.1590/S0100-72032007000400002
PURPOSE: the premature rupture of membranes (PROM) has been a reason for many investigations, amongst which the involved immune mechanisms. Ahead of the scarcity of studies related to the subject, this work had as objective to evaluate the serum values of IgA, IgG, IgM, C3 and C4 in pregnant women with pre-term PROM. METHODS: in this transversal study, 36 pregnant women had been enclosed, with gestational age between 23 and 37 weeks. Of this total, 15 women had had laboratorial and clinical diagnosis of PROM. Patients with beginning of the childbirth work, clinical signals of infection, clinical dysfunction with systemic repercussion had been excluded. Serum concentrations of immunoglobulin (IgA), immunoglobulin M (IgM) and immunoglobulin G (IgG), C3 and C4 had been evaluated in the patients with (study group) and without PROM (control group). Correlation among dosages; number of childbirths and time of rupture was determined by Spearman coefficient correlation (r value). RESULTS: serum levels of IgA (average±SD) had been significantly higher in the patients of the control group (271.0±107.0 versus 202.9±66.1; respectively, control and study group; p=0.024). There was no statistical difference when the levels of IgM, IgG, C3 and C4 had been compared between two groups. Significant association was not noticed between the number of childbirths and the IgA, IgM, IgG, C3 and C4 dosages (Spearman; r between -0,009 and 0,027; p>0,05). The average time of rupture of study group patients was of 19.1 hours (one - 72 hours), without association with the evaluated serum dosages. CONCLUSIONS: pregnant women with PROM show levels of IgA significantly lower than normal pregnant patients. The variable "number of childbirths" does not act as a factor of confusion in the comparative analysis of the dosages obtained in patients with or without PROM, as well as also it did not have association between the time of rupture and the immunoglobulin and complements serum dosages.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):501-505
DOI 10.1590/S0100-72032003000700006
PURPOSE: to identify Listeria monocytogenes (Lm) in human placentas by immunohistochemistry (IHC) and relate its presence to the histological alterations found on conventional examination, to the pregnancy trimester, age of pregnant women, cases of abortion and premature delivery, and to the occurrence of habitual abortion. METHODS: a retrospective study was carried out at the pathology service of a teaching hospital in the city of Porto Alegre in 2000. The paraffin blocks of 254 placentas, obtained from abortion, premature delivery and full-term birth, were analyzed by conventional histology using hematoxylin and eosin (HE) staining. The IHC assay consisted of a rabbit anti-listeria polyclonal antibody B65420R (Biodesign®) diluted 1:1000, in addition to the avidin-biotin-streptavidin complex; 148 placentas revealed inflammatory disorders, hemorrhage, necrosis and thrombosis. The c² test was used for statistical analysis. RESULTS: Listeria monocytogenes was detected in 33.78% of the placentas analyzed by IHC. Chorioamnionitis and villitis showed significant statistical difference in the positive placentas. Lm occurred in the 1st, 2nd and 3rd trimester of pregnancy. The age of pregnant women, the cases of abortion and/or premature births were not statistically different as to the presence or absence of Lm in the placentas. Habitual abortions occurred in patients with or without Lm in the placental tissue. CONCLUSION: Immunohistochemistry may be used to confirm the histopathological diagnosis of listeriosis in all trimesters of pregnancy.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(3):175-179
DOI 10.1590/S0100-72032002000300005
Purpose: to determine the presence of asymptomatic amniotic fluid infection in pregnant women, to identify the bacterial agents involved in the infection and to determine the antimicrobial susceptibility in vitro. Methods: amniotic fluid samples were obtained by amniocentesis from 81 pregnant women without labor signs and without suspucion of clinical infection, attended at Maternidade Escola Assis Chateaubriand from August 1997 to January 1999. The presence of aerobic bacteria, strict/facultative anaerobic bacteria and genital mycoplasmas was investigated. The anaerobic bacteria were identified by the ATB SystemÒ (Biolab Mérieux) and mycoplasmas by the IST MycoplasmaÒ kit (Biolab-Mérieux). Results: among the obtained samples, eight (9.8%) showed positive culture and in two samples two different strains were identified. The isolated pathogens were Ureaplasma urealyticum (7 cases, 8.6%), Mycoplasma hominis (1 case, 1.2%) and Peptostreptococcus sp (2 cases, 2.4%). The antimicrobial susceptibility was characterized by great mycoplasma resistance to erythromycin (37.5%) and no resistance to cyclins. Conclusions: the percentage of asymptomatic infections was high, and furthe research is necessary to evaluate the asymptomatic infection consequences in pregnant women and their newborns, involving methods that identify genital mycoplasmas, which were the most frequently isolated bacteria.