Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(5):374-376
07-30-2021
To analyze effects of the COVID-19 pandemic on the consumption of personal protective equipment and products (PPEP), as well as the frequency of surgical site infection (SSI) among non-COVID-19 patients submitted to cesarean sections.
A retrospective study was conducted in a maternity unity of a public teaching hospital which was not part of the reference service for COVID-19 treatment. It compared PPEP consumption and the occurrence of SSI after cesarean sections in monthly periods before and after the occurrence of the first case of COVID-19 in Porto Alegre, state of Rio Grande do Sul, Brazil. Personal protective equipment and products consumption was measured as units of masks, gloves, gowns, and caps, and use of alcohol-based products or soap for hand sanitation asml/patient/day. The SSI index was calculated as the proportion of cases of SSI over the number of cesarean sections performed monthly during the study period.
There was an increase in all measured items of PPEP, with consumption of disposable masks with a median of 1,450 units in the pre-COVID period, and of 2550 in the post-COVID period (a 75.9% increase). A decrease of 49% in SSI was detected, with a median of 1.74 in the pre-COVID period and of 0.89 in the post-COVID period.
The increase in consumption of PPEP could be a result of safer practices adopted by healthcare workers with the advent of COVID-19, of which the following reduction in the occurrence of SSI could be a direct consequence. Despite the severity of the crisis, one could state that extreme situations can lead to valuable reflections and opportunities for improvement.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):436-441
07-27-2021
The aim of the present study was to evaluate the risk factors for cesarean section (C-section) in low-risk multiparous women with a history of vaginal birth.
The present retrospective study included low-risk multiparous women with a history of vaginal birth who gave birth at between 37 and 42 gestational weeks. The subjects were divided into 2 groups according to the mode of delivery, as C-section Group and vaginal delivery Group. Risk factors for C-section such as demographic characteristics, ultrasonographic measurements, smoking, weight gain during pregnancy (WGDP), interval time between prior birth, history of macrosomic birth, and cervical dilatation at the admission to the hospital were obtained fromthe charts of the patients. Obstetric and neonatal outcomes were compared between groups.
The most common C-section indications were fetal distress and macrosomia (33.9% [n=77 and 20.7% [n=47] respectively). A bivariate correlation analysis demonstrated that mothers aged>30 years old (odds ratio [OR]: 2.09; 95% confidence interval [CI]: 1.30-3.34; p=0.002), parity >1 (OR: 1.81; 95%CI: 1.18-2.71; p=0.006), fetal abdominal circumference (FAC) measurement>360mm (OR: 34.20; 95%CI: 8.04 -145.56; p<0.001)) and<345mm (OR: 3.06; 95%CI: 1.88-5; p<0.001), presence of large for gestational age (LGA) fetus (OR: 5.09; 95%CI: 1.35-19.21; p=0.016), premature rupture of membranes (PROM) (OR: 1.52; 95%CI: 1-2.33; p=0.041), and cervical dilatation<5cm at admission (OR: 2.12; 95%CI: 1.34-3.34; p=0.001) were associated with the group requiring a C-section.
This is the first study evaluating the risk factors for C-section in low-risk multiparous women with a history of vaginal birth according to the Robson classification 3 and 4. Fetal distress and suspected fetal macrosomia constituted most of the Csection indications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):311-316
06-18-2021
A cesarean scar pregnancy (CSP) is a scary and life-threatening complication of cesarean section (CS). Nevertheless, the incidence of CS is constantly growing. The CSP incidence is 0,15% of pregnancies after CS which represents 6,1% of all ectopic pregnancies in women with condition after CS. Therefore, it should be more present in the clinical daily routine. From mild nonspecific symptoms to hypovolemic shock, diagnosis and therapy must be performed quickly. With the progressive growth of the scar pregnancy, a uterine rupture involves the risk of severe bleeding, and an emergency hysterectomy could be necessary. Prolongation of pregnancy has been successful only in a few cases.We report 11 cases from our hospital in the past 10 years. In the discussion, treatment options of this complication with an increasing incidence, which is associated with serious morbidity and mortality, are presented based on the current literature. Treatment options include drug therapy, but also surgical or combined procedures with radiological intervention.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):9-13
03-08-2021
We evaluated risk factors to determine if there were specific risk factors that could predict massive bleeding in nulliparous women with placenta previa.
The participants were classified into two groups. Women with a calculated blood loss ≥ 1,000mL were included in the massive bleeding group. Women without any signs or symptoms related with hypovolemia or with a calculated bleeding volume < 1,000 mL were categorized into the non-massive bleeding group.
There were 28 patients (40.6%) with massive bleeding and 41 cases (59.4%) with non-massive bleeding. The calculated blood loss and number of cases that required red cell transfusions were statistically different between the groups (< 0.005 and 0.002, respectively). There were no statistically significant differences in terms of maternal or fetal factors, placental location, or delivery characteristics between the two groups.
We could not determine the predictive features for massive hemorrhage based on clinical features, delivery features, or placental location.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):91-96
01-19-2021
To analyze the factors associated with the prevalence of exclusive breastfeeding (EBF) for up to six months in mother/infant binomials cared for at a usual-risk maternity hospital.
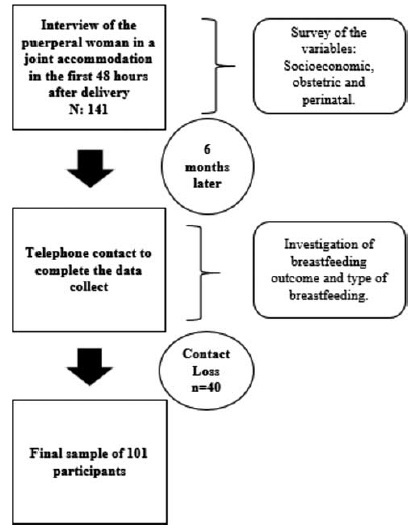
The present is a descriptive, longitudinal, prospective, quantitative study. Socioeconomic, obstetric and perinatal variables from 101 mother/infant binomials in a Public Maternity Hospital in the city of Curitiba, state of Paraná, Brazil, were investigated during hospitalization after delivery and 6 months after birth. For the statistical analysis, the Chi-squared test was used. The variables that showed values of p < 0.25 for the Chi-squared test were also submitted to an odds ratio (OR) analysis.
The prevalence (42.6%) of EBF was observed. Most women (93.1%) had had more than 6 prenatal consultations, and the variables maternity leave and support to breastfeeding were associated with EBF. Support to breastfeeding by professionals and family members increased 4-fold the chance of maintenance of EBF (OR = 0.232; 95% confidence intercal [95%CI]: 0.079 to 0.679; p = 0.008). Cracked nipples were the biggest obstacle to breastfeeding, and low milk production was the main responsible factor for weaning.
The encouragement of breastfeeding and the mother’s stay for a longer period with the child contributed to the maintenance of EBF until the sixth month of life of the infant.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(2):84-90
01-19-2021
To analyze and compare the frequency of cesarean sections and vaginal deliveries through the Robson Classification in pregnant women attended at a tertiary hospital in two different periods.
Cross-sectional, retrospective study of birth records, comprising 4,010 women, conducted from January 2014 to December 2015 in the only public regional referral hospital for the care of high- risk pregnancies, located in Southern Brazil.
The overall cesarean section rate reached 57.5% and the main indication was the existence of a previous uterine cesarean scar. Based on the Robson Classification, groups 5 (26.3%) and 10 (17.4%) were the most frequent ones. In 2015, there was a significant increase in the frequency of groups 1 and 3 (p < 0.001), when compared with the previous year, resulting in an increase in the number of vaginal deliveries (p < 0.0001) and a reduction in cesarean section rates.
The Robson Classification proved to be a useful tool to identify the profile of parturients and the groups with the highest risk of cesarean sections in different periods in the same service. Thus, it allowsmonitoring in a dynamic way the indications and delivery routes and developing actions to reduce cesarean rates according to the characteristics of the pregnant women attended.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):690-696
12-21-2020
To evaluate the prevalence of hypertensive disorders, perinatal outcomes (preterm infants, low birthweight infants and Apgar score < 7 at the 5th minute and fetal deaths) and the cesarean rates in pregnant women hospitalized for delivery at the Maternidade Hilda Brandão da Santa Casa de Belo Horizonte, Belo Horizonte, state of Minas Gerais, Brazil, from March 1, 2008 to February 28, 2018.
A case-control study was performed, and the groups selected for comparison were those of pregnant women with and without hypertensive disorders. Out of the 36,724 women, 4,464 were diagnosed with hypertensive disorders and 32,260 did not present hypertensive disorders
The prevalence of hypertensive disorders was 12.16%; the perinatal outcomes and cesarean rates between the 2 groups with and without hypertensive disorders were: preterm infants (21.70% versus 9.66%, odds ratio [OR] 2.59, 95% confidence interval [CI], 2.40-2.80, p < 0.001); low birthweight infants (24.48% versus 10.56%; OR 2.75; 95% CI, 2.55-2.96; p < 0.001); Apgar score < 7 at the 5th minute (1.40% versus 1.10%; OR 1.27; 95% CI, 0.97-1.67; p = 0.84); dead fetuses diagnosed prior to delivery (1.90% versus 0.91%; OR 2.12; 95% CI, 1.67-2.70; p < 0.001); cesarean rates (60.22% versus 31.21%; OR 3.34; 95% CI, 3.14-3.55; p < 0.001).
Hypertensive disorders are associated with higher rates of cesarean deliveries and higher risk of preterm infants, low birthweight infants and a higher risk of fetal deaths.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(10):597-606
12-21-2020
The purpose of the present study was to evaluate the quality of mother-child bonding in three different contexts related to the labor, that is, vaginal delivery, elective cesarean section, and intrapartum cesarean section.
This was an observational, cross-sectional clinical study conducted in two cities within the state of São Paulo, Brazil. The study sample consisted of 81 babies born without any major complications during pregnancy and labor, aged 3 to 4 months, and their respective mothers, aged between 20 and 35 years old, primiparous, living in the cities of Palmital and Ourinhos, state of São Paulo, Brazil. The evaluation of the quality of the maternal-filial interaction was performed through video-image analysis, using the Mother-baby Interaction Observation Protocol from 0 to 6 months (POIMB 0-6, in the Portuguese acronym).
Mothers who had vaginal delivery had higher amount of visual contact or attempted visual contact (p = 0.034), better response to the social behavior of the child (p = 0.001) and greater sensitivity (p = 0.007) than the others. Their children also showed more interaction with them, as they looked more frequently at the mother's face (p ≤ 0.008) and responded more frequently to the mother's communicative stimulus (p < 0.001).
Considering the occurrence of vaginal delivery, it is concluded that the interaction between the mother-child dyad is quantitatively larger and qualitatively better when compared with intrapartum or elective cesarean section.