Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):269-275
DOI 10.1590/S0100-72032004000400002
OBJECTIVE: to evaluate the performance of Pap smear, hybrid capture II (HC II), and visual inspection with acetic acid in the detection of pre-invasive and invasive cervical lesions. METHODS: a total of 2281 women were submitted to a clinical exam, including Pap smear, HC II for HPV DNA detection and visual inspection with 5% acetic acid (VIA). When at least one of the tests was positive, colposcopy was performed and targeted biopsies were taken from suspicious lesions. Colposcopy was also performed in 420 women with negative results. Test performance was evaluated, using colposcopy as the gold standard, with or without biopsy. RESULTS: Pap smear, VIA and HC II were positive in 9.2, 10.9 and 17.5% of all women screened, respectively. Although at least one positive test was found in 671 women (29.4%), only 82 (3.6%) presented histologically confirmed disease (50 NIC1, 20 NIC2, 7 NIC3, and 5 invasive carcinoma). VIA and HC II sensitivities were similar and significantly higher than Pap smear. Pap smear showed better specificity than VIA and than HC II. In women with a negative Pap smear result, VIA showed better performance than HC II. CONCLUSION: Pap smear combined with VIA performed better than Pap smear combined with HC II or than Pap smear alone.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):233-240
DOI 10.1590/S0100-72032004000300010
OBJECTIVE: to evaluate the existence of intra and intercytophathologists disagreement in the analysis of cervical slides previously diagnosed as atypical skin cells with undetermined significance (ASCUS), and the degree of this disagreement. METHODS: a transversal study of 50 cervical slides of Pap smears previously diagnosed as ASCUS, collected in November 2000 in Contagem town. They were analyzed and classified by four cytopathologists according to the first Bethesda system review of 1991 (normal, atrophic alteration, inflammatory alteration, suggestive of LoSIL, suggestive of HiSIL, suggestive of invasive carcinoma and others). After the first analysis, the slides were renumbered in a random order and sent to the same cytophathologists for a new exam. The Kappa test and the weighted Kappa were used in the analysis of the results. RESULTS: there was a high degree of disagreement between the different analyses of the same cytopathologist, varying from 7.8 to 74.4% according to the Kappa test. When a weight of 20% was settled for each degree of disagreement, these values increased from 16.1% for the cytopathologist A to 81.08% for the cytopathologist B. Concerning the comparative analyses made by different examiners the Kappa test values obtained varied from 50.6% to 63.4% in the normal and weighted versions, respectively. CONCLUSIONS: this study confirms the existence of subjectivity in the analysis of the ASCUS category and imprecision in the analysis criteria by the same examiner.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(1):59-64
DOI 10.1590/S0100-72032004000100009
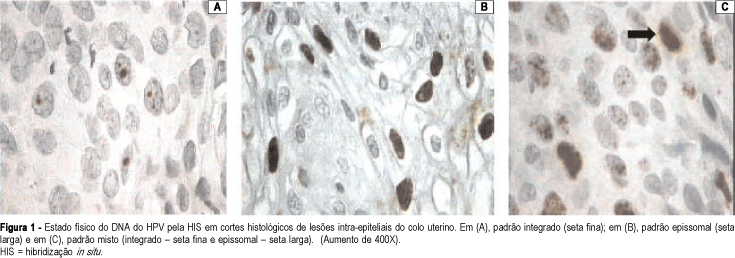
PURPOSE: to carry out a molecular study (in situ hybridization) on patients who present intraepithelial lesions of the uterine cervix, and to assess the frequency and the physical state of the human papillomavirus (HPV). METHODS: histological sections of biopsies of the uterine cervix from 84 patients were evaluated by in situ hybridization, with a broad-spectrum probe, which allows the identification of the HPV types 6, 11, 16, 18, 31, 33, 35, 39, 42, 45, and 56 and with specific probes for HPV types 6, 11, 16, 18, 31, and 33. The physical patterns of HPV DNA found were: episomal, when the entire nucleus stains with biotin (brown); integrated - one or two brown points in the hybridized nucleus, or mixed, associating both patterns. Of the 84 patients evaluated, 31 (36.9%) had low-grade squamous intraepithelial lesions (LSIL), and 53 (63.1%) had high-grade squamous intraepithelial lesions (HSIL) on histological examination. Fisher's exact test was used for the statistical analysis. RESULTS: considering all the cases, 46 (54.7%) were positive for HPV DNA with the broad-spectrum probe. Regarding typing, HPV-16 was the most frequent in HSIL (12 cases - 22.6% - p<0.05). The frequencies of the other HPV types did not show statistically significant differences between the LSIL and HSIL cases. By physical condition assessment of the HPV DNA, the percentage of the episomal (most common in LSIL) and integrated patterns showed no significant differences between the two groups; the mixed HSIL type prevailed when compared to LSIL: 26.4 and 3.2%, respectively (p<0.01). The physical condition of the HPV DNA, integrated in the host cell, was more frequent in the most severe cases. CONCLUSIONS: HPV-16 was the most frequent in HSIL cases. The frequencies of the other HPV types did not show statistically significant differences between the LSIL and HSIL cases. The physical condition of the HPV DNA, integrated in the host cell, was more frequent in the more severe cases.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(1):47-51
DOI 10.1590/S0100-72032001000100007
Purpose: to evaluate the incidence of thermal damage to the specimens excised through large loop excision of the transformation zone (LLETZ) and to determine qualitatively and quantitatively the thermal injury to the ectocervical and endocervical epithelia as well as the influence of the menstrual phase on such process. Methods: we performed a prospective study of 100 patients with high-grade squamous intraepithelial lesions (HGSIL). Thermal damage was subdivided into three grades according to Messing et al¹. Results: thermal injury occurred in all the cases, however, through statistical analysis we found that in 91% of the cases it was insignificant, thus leading to a precise histological evaluation, hence to measure the thermal injury was unnecessary. The grade and extent of thermal damage in excised specimens using LLETZ had no relation to the menstrual phase. The extension of thermal tissue alteration in the endocervical epithelia was 271,6 mu while the extension in ectocervical epithelia was 254,8 mu, showing that the extension of thermal damage is significantly higher in endocervical epithelia. Of the one hundred patients, 80 were in menacme and 20 in menopause correlating the grade and extension of thermal damage with the menstrual state. Conclusion: there was no significant difference in both qualitative and quantitative evaluations. There is no need to measure the thermal damage.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(5):313-319
DOI 10.1590/S0100-72032001000500007
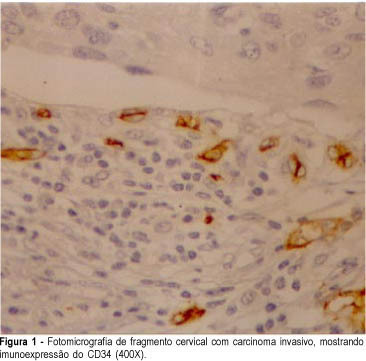
Purpose: to compare the efficiency of anti-factor VIII and anti-CD34 antibodies as vascular makers in cervical cancer, in cervical intraepithelial neoplasia and in normal cervix. Methods: using an immunohistochemical method, factor VIII-related antigen and leukocyte antigen CD34, we performed microvascular counts in 18 squamous cell carcinomas, in 15 cervical high-grade intraepithelial neoplasia, in 15 low-grade intraepithelial lesions and in 10 normal cervices. Using light microscopy we counted microvessels per 400X field in the most active areas of neovascularization with higher microvessel density in each case. Results: the average of microvessels stained with anti-CD34 in invasive carcinoma, high-grade intraepithelial lesions, low-grade intraepithelial lesions and in the normal cervices was 154, 134, 112 and 93, respectively. When we used anti-factor VIII the average was 56, 44, 33 and 30 vessels, following the same order. High-grade intraepithelial lesions and invasive carcinomas showed greater means number of vessels than normal tissue. Conclusions: the use of anti-CD34 allowed the detection of a greater number of vessels when compared to anti-factor VIII. However, we could observe that anti-factor VIII staining was able to significantly discriminate high-grade from low-grade lesions.