-
Original Article01-11-2023
Arabin-pessary or McDonald Cerclage in Cervical Shortening?
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):764-769
Abstract
Original ArticleArabin-pessary or McDonald Cerclage in Cervical Shortening?
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):764-769
Views169See moreAbstract
Objective
The aim of the present study is to compare the effectiveness of Arabin pessary and McDonald cervical cerclage on preterm delivery.
Methods
We conducted a retrospective analysis of data from patients who underwent either Arabin pessary or McDonald cerclage between January 1, 2019, and January 1, 2023. A total of 174 patients were included in the study, with 31 undergoing Arabin pessary and 143 receiving cervical cerclage using the McDonald technique in singleton pregnant women with cervical insufficiency, which applied between 14 and 22 gestational weeks. We included singleton pregnant women with normal morphology, and with normal combined test. The primary outcome was the impact of each method on preterm delivery (< 34 gestational weeks).
Results
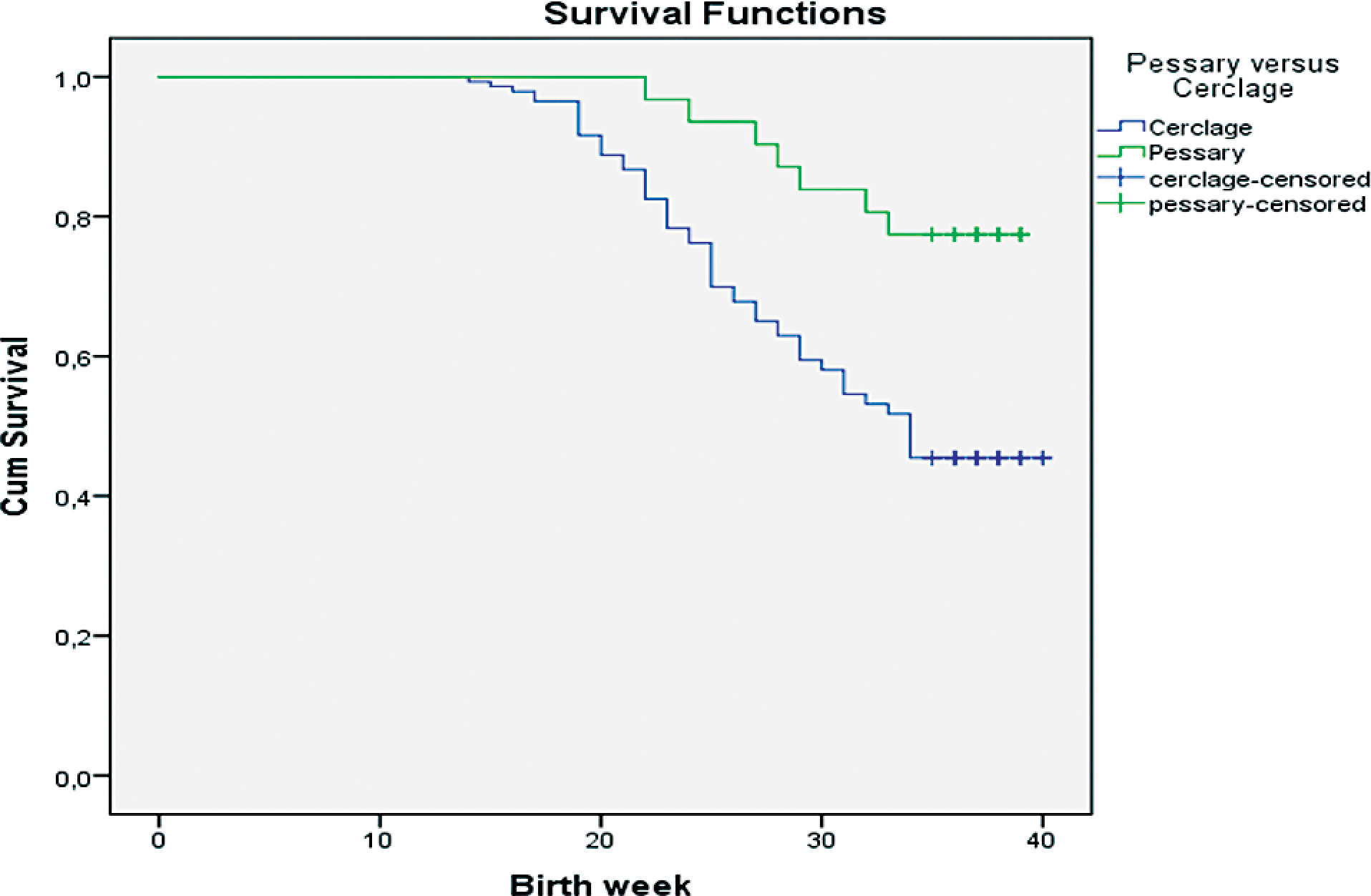
The weeks of cervical cerclage or pessary application were compatible with each other (p < 0.680). The pessary group had a statistically significant longer time to delivery compared with the Cerclage group (cerclage group mean 30.8 c 7.1 standard deviation [SD] versus pessary group mean 35.1 ± 4.4 SD; p < 0.002). A statistically significant difference was found between the pessary and cerclage groups in terms of delivery at < 34 weeks (p = 0.002). In patients with cervical length between 25 and 15mm and < 15mm, no significant difference was found between the pessary and cerclage groups in terms of delivery week (p < 0.212; p < 0.149). Regardless of the technique applied, no statistically significant difference was observed between cervical length and birth < 34 weeks.
Conclusion
Our study found that pessary use for cervical insufficiency is statistically more effective than cervical cerclage surgery in preventing preterm births < 34 weeks in singleton pregnancy.
-
Original Article11-04-2003
Gestational and perinatal outcomes of pregnancies with cervical incompetence submitted to elective cerclage
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):483-489
Abstract
Original ArticleGestational and perinatal outcomes of pregnancies with cervical incompetence submitted to elective cerclage
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):483-489
DOI 10.1590/S0100-72032003000700004
Views82See morePURPOSE: to describe the pregnancy outcome of women submitted to cervical cerclage during pregnancy. METHODS: a series of 123 pregnancies in 116 women submitted to elective cervical cerclage by Espinosa-Bahamondes, Palmer and MacDonald techniques and followed at the High-Risk Antenatal Care Unit at CAISM/UNICAMP is described. Variables were analyzed through frequency, mean and standard deviation, comparisons were made using c² or Fisher exact tests. RESULTS: 73% had at least one previous abortion, 17.9% had had 3 prior abortions, and 48% had prior preterm deliveries. The mean gestational age at cerclage was 16 weeks. Cerclage by the Espinosa-Bahamondes technique predominated (94.3%). The overall complication rate was 69%, with preterm labor as the most frequent (31.7%), followed by vaginitis (26%), preterm premature rupture of membranes (10.5%) and fetal death (8.7%). Other clinical complications were less common and included urinary tract infections (5.6%), hypertensive disorders (4%) and gestational diabetes (2.4%). Fetal loss occurred in 8.9% of pregnancies (11 stillbirths). Premature deliveries were present in 18%. History of previous premature deliveries was associated with the occurrence of premature deliveries. CONCLUSION: Obstetrical history compatible with cervical incompetence was frequent, and prior preterm delivery was associated with a preterm delivery in the pregnancy under analysis. The use of cerclage by the Espinosa-Bahamondes technique resulted in 18% of premature newborns, and 104 per thousand rate of perinatal death. Prospective, controlled trials are needed to evaluate the real benefits of cervical cerclage performed during pregnancy.
-
Original Article05-19-2003
Characterization of pregnancy with cervical incompetence
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(1):29-34
Abstract
Original ArticleCharacterization of pregnancy with cervical incompetence
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(1):29-34
DOI 10.1590/S0100-72032003000100005
Views77See morePURPOSE: to identify characteristics common to women who suffer from cervical incompetence (CI) allowing their early identification and helping in the follow-up of the gestational-postdelivery cycle. PATIENTS AND METHODS: fifty pregnant women suffering from CI and submitted to uterine cerclage according to modified McDonald's technique were analyzed in an observational descriptive study. The following variables of the medical records were evaluated: age, preceding obstetrical aspects, time of CI diagnosis, cerclage-related aspects and preterm delivery incidence. RESULTS: the average age of the mothers was 29.28 years and mean number of previous gestations was 3.76. As to the preceding obstetrical aspects, 189 gestations with a CI diagnosis were reported and cerclage had been applied to 18 of them, resulting in 18 babies who were born alive (8 preterm deliveries and 10 term deliveries). Of the 171 previous pregnancies in which CI diagnosis was not reported, 90 progressed to abortion, 68 were preterm and 13 were term deliveries. In 30 (60%) patients, CI was diagnosed during the intergestational interval, and 20 (40%) during gestation. The average gestational period in which patients were submitted to cerclage was 18.29 weeks; 40% of the cerclages were emergency procedures and 60% were elective. The incidence of prematurity was 30% (15/50). CONCLUSION: careful obstetrical evaluation of multiparous women, presenting recurrent miscarriages, during the intergestational interval and/or during the first trimester of pregnancy, may allow the early diagnosis and adequate treatment of CI, avoiding prematurity.


