-
Original Article
Sedentary Lifestyle and High-Carbohydrate Intake are Associated with Low-Grade Chronic Inflammation in Post-Menopause: A Cross-sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):317-324
07-01-2016
Summary
Original ArticleSedentary Lifestyle and High-Carbohydrate Intake are Associated with Low-Grade Chronic Inflammation in Post-Menopause: A Cross-sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):317-324
07-01-2016Views171See moreAbstract
Introduction
Cardiovascular disease (CVD) is the leading cause of death in post menopausal women, and inflammation is involved in the atherosclerosis process.
Purpose
to assess whether dietary pattern, metabolic profile, body composition and physical activity are associated with low-grade chronic inflammation according to highsensitivity C-reactive protein (hs-CRP) levels in postmenopausal women.
Methods
ninety-five postmenopausal participants, with no evidence of clinical disease, underwent anthropometric, metabolic and hormonal assessments. Usual dietary intake was assessed with a validated food frequency questionnaire, habitual physical activity was measured with a digital pedometer, and body composition was estimated by bioelectrical impedance analysis. Patients with hs-CRP ≥ 10 mg/L or using hormone therapy in the last three months before the study were excluded from the analysis. Participants were stratified according to hs-CRP lower or ≥3 mg/L. Sedentary lifestyle was defined as walking fewer than 6 thousand steps a day. Two-tailed Student's t-test, Wilcoxon-Mann-Whitney U or Chi-square (x 2) test were used to compare differences between groups. A logistic regression model was used to estimate the odds ratio of variables for high hs-CRP.
Results
participants with hs-CRP ≥ 3 mg/L had higher body mass index (BMI), body fat percentage, waist circumference (WC), triglycerides, glucose, and homeostasis model assessment of insulin resistance (HOMA-IR) (p = 0.01 for all variables) than women with hs-CRP <3 mg/L. Also, women with hs-CRP ≥3 mg/L had a higher glycemic load diet and lower protein intake. Prevalence of sedentary lifestyle (p < 0.01) and metabolic syndrome (p < 0.01) was higher in women with hs-CRP ≥3 mg/L. After adjustment for age and time since menopause, the odds ratio for hs- CRP ≥3 mg/L was higher for sedentary lifestyle (4.7, 95% confidence interval [95%CI] 1.4-15.5) and carbohydrate intake (2.9, 95%CI 1.1-7.7).
Conclusions
sedentary lifestyle and high-carbohydrate intake were associated with low-grade chronic inflammation and cardiovascular risk in postmenopause.
-
Original Articles
Association between Lipid Accumulation Product and Hirsutism in Patients with Polycystic Ovary Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):71-76
02-01-2016
Summary
Original ArticlesAssociation between Lipid Accumulation Product and Hirsutism in Patients with Polycystic Ovary Syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):71-76
02-01-2016Views147See moreObjective
Polycystic ovary syndrome (PCOS) is the most common endocrine metabolic disorder in women between menarche and menopause. Clinical hyperandrogenism is the most important diagnostic criterion of the syndrome, which manifests as hirsutism in 70% of cases. Hirsute carriers of PCOS have high cardiovascular risk. Lipid accumulation product (LAP) is an index for the evaluation of lipid accumulation in adults and the prediction of cardiovascular risk. The aim of this study was to evaluate the association between LAP and hirsutism in women with PCOS.
Methods
This was a cross-sectional observational study of a secondary database, which included 263 patients who had visited the Hyperandrogenism Outpatient Clinic from November 2009 to July 2014. The exclusion criteria were patients without Ferriman-Gallwey index (FGI) and/or LAP data. We used the Rotterdam criteria for the diagnosis of PCOS. All patients underwent medical assessment followed by measurement and recording of anthropometric data and the laboratory tests for measurement of the following: thyroid-stimulating hormone, follicle-stimulating hormone, prolactin, total testosterone, sex hormone binding globulin, 17-α-hydroxyprogesterone (follicular phase), glycohemoglobin A1c, and basal insulin. In addition, the subjects underwent lipid profiling and oral glucose tolerance tests. Other laboratory measurements were determined according to clinical criteria. LAP and the homeostatic model assessment index (HOMA-IR) were calculated using the data obtained. We divided patients into two groups: the PCOS group with normal LAP (< 34.5) and the PCOS group with altered LAP (> 34.5) to compare the occurrence of hirsutism. For statistical analysis, we used SPSS Statistics for Windows(r) and Microsoft Excel programs, with descriptive (frequencies, percentages, means, and standard deviations) and comparative analyses (Student's t-test and Chi-square test). We considered relations significant when the p-value was≤0.05.
Results
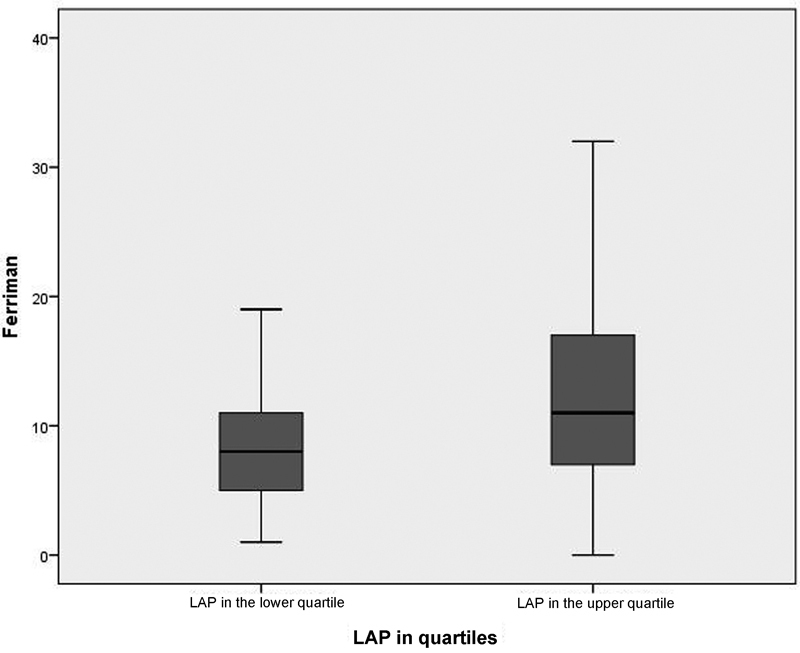
LAP was high in most patients (n = 177; 67.3%) and the FGI indicated that 58.5% of the patients (n = 154) had hirsutism. The analysis by LAP quartiles showed a positive correlation (p = 0.04) among patients with a high FGI and an upper quartile LAP (> 79.5) when compared with those with LAP < 29.0 (lower quartile).
Conclusion
This study demonstrated an association between high LAP and hirsutism. The FGI could represent a simple and low-cost tool to infer an increased cardiovascular risk in women with PCOS.
-
Artigos Originais
Cardiovascular risk markers in polycystic ovary syndrome in women with and without insulin resistance
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(3):111-116
06-08-2009
Summary
Artigos OriginaisCardiovascular risk markers in polycystic ovary syndrome in women with and without insulin resistance
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(3):111-116
06-08-2009DOI 10.1590/S0100-72032009000300002
Views106PURPOSE: to evaluate whether the presence of insulin resistance (IR) alters cardiovascular risk factors in women with polycystic ovary syndrome (POS). METHODS: transversal study where 60 POS women with ages from 18 to 35 years old, with no hormone intake, were evaluated. IR was assessed through the quantitative insulin sensitivity check index (QUICKI) and defined as QUICKI <0.33. The following variables have been compared between the groups with or without IR: anthropometric (weight, height, waist circumference, arterial blood pressure, cardiac frequency), laboratorial (homocysteine, interleucines-6, factor of tumoral-α necrosis, testosterone, fraction of free androgen, total cholesterol and fractions, triglycerides, C reactive protein, insulin, glucose), and ultrasonographical (distensibility and carotid intima-media thickness, dilation mediated by the brachial artery flux). RESULTS: Eighteen women (30%) presented IR and showed significant differences in the following anthropometric markers, as compared to the women without IR (POS with and without IR respectively): body mass index (35.56±5.69 kg/m² versus 23.90±4.88 kg/m², p<0.01), waist (108.17±11.53 versus 79.54±11.12 cm, p<0.01), systolic blood pressure (128.00±10.80 mmHg versus 114.07±8.97 mmHg, p<0.01), diastolic blood pressure (83.67±9.63 mmHg versus 77.07±7.59 mmHg, p=0.01). It has also been observed significant differences in the following laboratorial markers: triglycerides (120.00±56.53 mg/dL versus 77.79±53.46 mg/dL, p=0.01), HDL (43.06±6.30 mg/dL versus 40.45±10.82 mg/dL, p=0.01), reactive C protein (7.98±10.54 mg/L versus 2.61±3.21 mg/L, p<0.01), insulin (28.01±18.18 µU/mL versus 5.38±2.48 µU/mL, p<0.01), glucose (93.56±10.00 mg/dL versus 87.52±8.75 mg/dL, p=0.02). Additionally, two out of the three ultrasonographical markers of cardiovascular risk were also different between the groups: carotid distensibility (0.24±0.05 mmHg-1 versus 0.30±0.08 mmHg-1, p<0.01) and carotid intima-media thickness (0.52±0.08 mm versus 0.43±0.09, p<0.01). Besides, the metabolic syndrome ratio was higher in women with IR (nine cases=50% versus three cases=7.1%, p<0.01). CONCLUSIONS: POS and IR women present significant differences in several ultrasonographical, seric and anthropometric markers, which point out to higher cardiovascular risk, as compared to women without POS and IR. In face of that, the systematic IR evaluation in POS women may help to identify patients with cardiovascular risk.
Key-words Biological markersCardiovascular diseaseEndotheliumInsulin resistancePolycystic ovary syndromeRisk factorsSee more -
Trabalhos Originais
Effects of raloxifene on plasma homocysteine concentration and lipid profile in postmenopausal women
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):573-578
10-14-2004
Summary
Trabalhos OriginaisEffects of raloxifene on plasma homocysteine concentration and lipid profile in postmenopausal women
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):573-578
10-14-2004DOI 10.1590/S0100-72032004000700010
Views97See morePURPOSE: to evaluate the effects of raloxifene on plasma homocysteine concentration and lipid profile in postmenopausal women. METHODS: twenty-four healthy postmenopausal women, aged 50 to 70 years, with osteopenia and/or osteoporosis, were submitted to raloxifene therapy, 60 mg/day, for six months. Plasma homocysteine concentration was determined before and after three and six months of therapy, as well as total cholesterol, HDL-cholesterol LDL-cholesterol and triglyceride levels. Plasma homocysteine was measured by a polarized immunofluorescence assay and serum lipids by the enzymatic and colorimetric method. Data were analyzed statistically by ANOVA, Newman-Keuls test and Pearson's correlation test. RESULTS: a significant decrease in total cholesterol of 15.3% (227.6±56.3 vs 200.6±29.8 vs 192.8±32.1 mg/dl; p<0.001) and LDL-cholesterol of 21.4% (151.4±46.3 vs 122.7±29.4 vs 119.0±28.6 mg/dl; p<0.001), and a significant increase in HDL-cholesterol of 9.5% (44.7±10.8 vs 52.2±12.6 vs 49.0±10.8 mg/dl; p<0.05) were observed. There was no reduction in triglyceride levels (134.9±50.3 vs 127.5±50.0 vs 121.0±36.0 mg/dl; p>0.05). Although not significant, a decrease in homocysteine by 4.5% (11.7±3.0 vs 11.0±2.9 vs 11.2±2.1 muM/l; p>0.05) was observed between the pre-and posttreatment periods, with a significant negative correlation between basal levels and posttreatment percentual reduction (r=-0.71; p<0.0001). CONCLUSIONS: raloxifene treatment, 60 mg/day, for six months caused a significant decrease in total and LDL-cholesterol and an increase in HDL-cholesterol in postmenopausal women. Plasma homocysteine concentration tended to decrease, this effect being more favorable in patients with elevated baseline levels.


