Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):712-716
To determine whether there was any difference in neonatal and maternal outcomes between breech vaginal delivery and cephalic vaginal delivery.
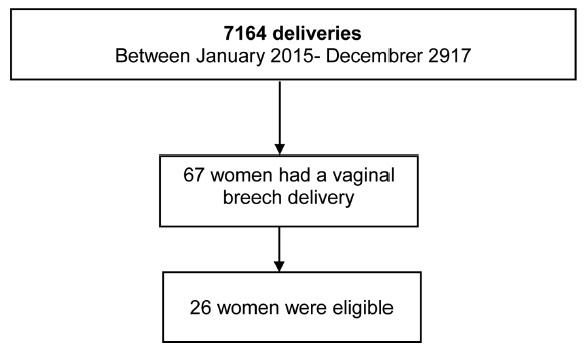
A retrospective, case-control study was conducted between January 2015 and December 2017 in a Portuguese hospital. A total of 26 cases of breech vaginal delivery were considered eligible and 52 pregnant women formed the control group.
Induced labor was more frequent in the breech vaginal delivery group (46% versus 21%, p = 0.022). Episiotomy was more common in the breech vaginal delivery group (80% versus 52%, p = 0.014), and one woman had a 3rd degree perineal laceration. Newborns in the study group had a lower birthweight (2,805 g versus 3,177 g, p < 0.001). There was no significant difference in the neonatal outcomes.
The present study showed that breech vaginal delivery at term compared with cephalic presentation was not associated with significant differences in neonatal and maternal morbidity. It also suggests that breech vaginal delivery remains a safe option under strict selection criteria and in the presence of an experienced obstetrician.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(1):04-10
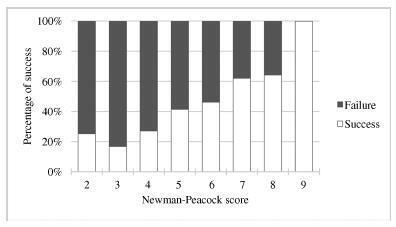
External cephalic version (ECV) is a maneuver that enables the rotation of the non-cephalic fetus to a cephalic presentation. The Newman-Peacock (NP) index, which was proposed by Newman et al. in a study published in 1993, was described as a prediction tool of the success of this procedure; it was validated in a North-American population, and three prognostic groups were identified.
To evaluate the value of the NP score for the prediction of a successful ECV in a Portuguese obstetrical population, and to evaluate maternal and fetal safety.
We present an observational study conducted from 1997-2016 with pregnant women at 36-38 weeks of pregnancy who were candidates for external cephalic version in our department. Demographic and obstetrical data were collected, including the parameters included in the NP index (parity, cervical dilatation, estimated fetal weight, placental location and fetal station). The calculation of the NP score was performed, and the percentages of success were compared among the three prognostic groups and with the original study by Newman et al. The performance of the score was determined using the Student t-test, the Chi-squared test, and a receiver operating characteristic (ROC) curve.
In total, 337 women were included. The overall success rate was of 43.6%. The univariate analysis revealed that multiparity, posterior placentation and a less engaged fetus were factors that favored a successful maneuver (p < 0.05). Moreover, a higher amniotic fluid index was also a relevant predictive factor (p < 0.05). The Newman-Peacock score had a poorer performance in our population compared with that of the sample of the original study, but we still found a positive relationship between higher scores and higher prediction of success (p < 0.001). No fetal or maternal morbidities were registered.
The Newman-Peacock score had a poorer performance among our population compared to its performance in the original study, but the results suggest that this score is still a useful tool to guide our clinical practice and counsel the candidate regarding ECV.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(8):519-523
DOI 10.1590/S0100-72032000000800008
Purpose: to evaluate the results of assistance to breech deliveries. Methods: this was a descriptive study where 160 pregnant women with breech presentation and live newborns were analyzed. They were divided into two groups according to the route of delivery. Clinical data concerning labor, delivery and newborns were studied. For statistical analysis vaginal deliveries were compared with cesarean sections using mean and standard deviation estimates, Student's t, Mann-Whitney and chi² tests. Results: the global cesarean section rate was 81.2%. The gestational age and the weight of the newborns were significantly lower in the vaginal delivery group. Prematurity and low birth weight were significantly associated with vaginal delivery. Only 14 newborns had an Apgar score below 7 at the fifth minute, almost 60% of them in the vaginal delivery group. Conclusions: this population presented a high cesarean section rate and also high perinatal morbidity, prematurity and low birth weight in the vaginal delivery group. These findings do not allow conclusions regarding the real relationships among breech presentation, route of delivery and perinatal outcomes. The control regarding gestational age and parity, besides a random decision on the route of delivery, is necessary for future conclusions.