-
Original Article04-30-2025
Evaluation of pathological complete response rates in breast cancer patients undergoing neoadjuvant therapy
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo13
Abstract
Original ArticleEvaluation of pathological complete response rates in breast cancer patients undergoing neoadjuvant therapy
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo13
Views84See moreAbstract
Objective:
This study aims to assess the rate of pathological complete response (pCR) in breast cancer patients undergoing neoadjuvant therapy and to explore its correlation with clinical, molecular, and prognostic factors.
Methods:
We conducted this retrospective observational study at Liga Contra o Câncer, a major public oncology reference center in Northeast Brazil. We included patients diagnosed with breast cancer who initiated neoadjuvant therapy between June 2018 and June 2019. Patients with a history of recurrent breast cancer or those who did not undergo surgery were excluded. The primary outcome was the pCR rate, with secondary outcomes including Overall Survival (OS), Disease-Free Survival (DFS), mortality, and disease recurrence. Follow-up extended until August 2022. We performed multivariate Cox regression analysis to correlate outcomes with predetermined variables.
Results:
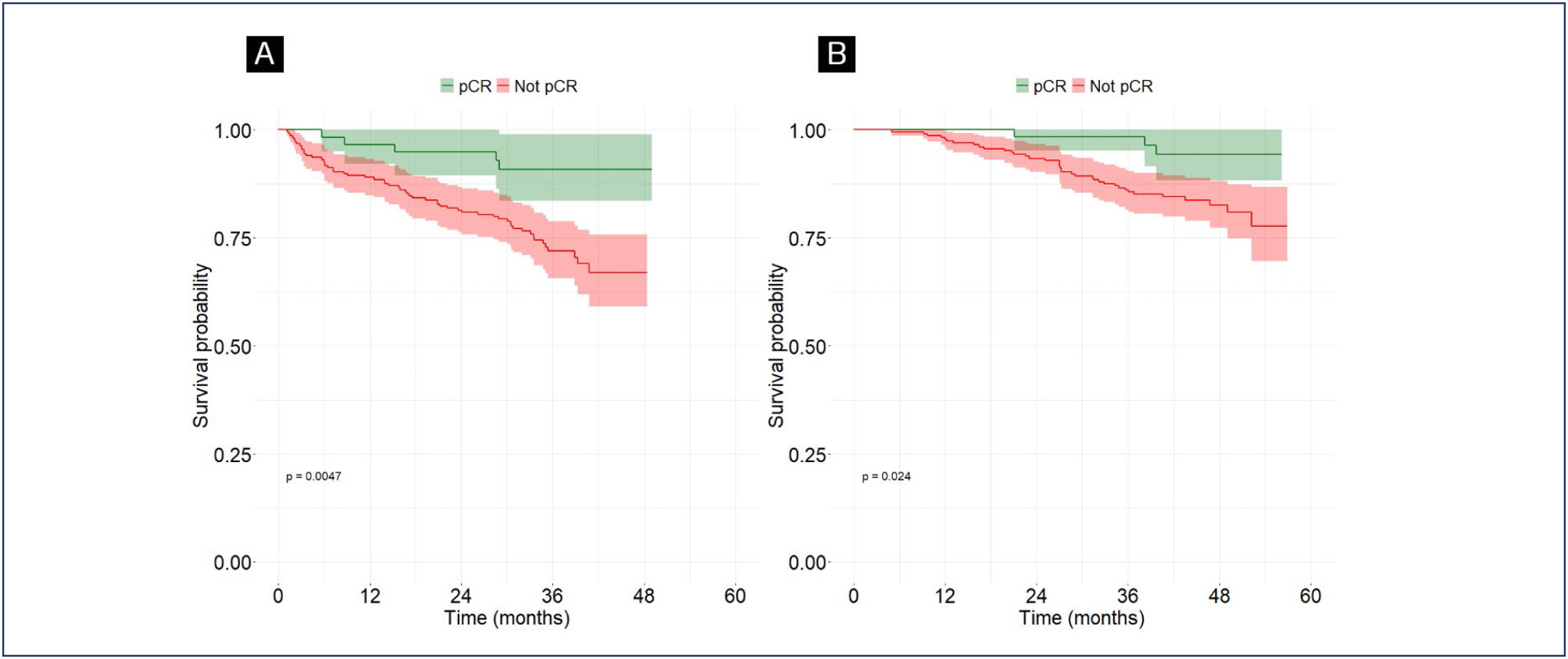
Of the 292 included patients, 63 (21.6%) achieved pCR. The mean follow-up duration was 42.8 months. Multivariate logistic regression analysis revealed an association between pCR and the AC-TH regimen [OR = 2.4; 95%CI = 1.13 - 5.24; p=0.023], as well as between pCR and HER2-positive tumors [OR 2.49; 95% CI = 1.14 - 5.86; p=0.028]. Complete pathological response was associated with higher DFS [HR 0.33; 95%CI 0.13-0.86; p=0.024].
Conclusion:
Neoadjuvant therapy demonstrated significant efficacy in achieving pathological response in breast cancer patients. We observed a strong association between the AC-TH regimen, HER2-positive status, and pCR.
-
Original Article10-23-2024
Nipple-sparing mastectomy in young versus elderly patients
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo90
Abstract
Original ArticleNipple-sparing mastectomy in young versus elderly patients
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo90
Views169See moreAbstract
Objective:
In this study, we compared indications and outcomes of 115 young (< 40 years) versus 40 elderly (> 60 years) patients undergoing nipple-sparing mastectomy (NSM) as risk-reducing surgery or for breast cancer (BC) treatment.
Methods:
Between January 2004 and December 2018, young and elderly patients undergoing NSM with complete data from at least 6 months of follow-up were included.
Results:
BC treatment was the main indication for NSM, observed in 85(73.9%) young versus 33(82.5%) elderly patients, followed by risk-reducing surgery in 30(26.1%) young versus 7(17.5%) elderly patients. Complication rates did not differ between the age groups. At a median follow-up of 43 months, the overall recurrence rate was higher in the younger cohort (p = 0.04). However, when stratified into local, locoregional, contralateral, and distant metastasis, no statistical difference was observed. During the follow-up, only 2(1.7%) young patients died.
Conclusion:
Our findings elucidate a higher recurrence rate of breast cancer in younger patients undergoing NSM, which may correlate with the fact that age is an independent prognostic factor. High overall survival and low complication rates were evidenced in the two groups showing the safety of NSM for young and elderly patients.
-
Original Article11-29-2021
Exposed Implant after Immediate Breast Reconstruction – Presentation and Analysis of a Clinical Management Protocol
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):690-698
Abstract
Original ArticleExposed Implant after Immediate Breast Reconstruction – Presentation and Analysis of a Clinical Management Protocol
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(9):690-698
Views219See moreAbstract
Objective
Infection and exposure of the implant are some of the most common and concerning complications after implant-based breast reconstruction. Currently, there is no consensus on the management of these complications. The aim of the present study was to review our cases and to present a clinical protocol.
Methods
We conducted a retrospective review of consecutive patients submitted to implant-based breast reconstruction between 2014 and 2016. All patients were managed according to a specific and structured protocol.
Results
Implant exposure occurred in 33 out of 277 (11.9%) implant-based reconstructions. Among these, two patients had history of radiotherapy and had their implant removed; Delayed reconstruction with a myocutaneous flap was performed in both cases. Signs of severe local infection were observed in 12 patients, and another 5 presented with extensive tissue necrosis, and they were all submitted to implant removal; of them, 8 underwent reconstruction with a tissue expander, and 2, with a myocutaneous flap. The remaining 14 patients had no signs of severe infection, previous irradiation or extensive tissue necrosis, and were submitted to primary suture as an attempt to salvage the implant. Of these, 8 cases (57.1%) managed to keep the
Conclusion
Our clinical protocol is based on three key points: history of radiotherapy, severe infection, and extensive tissue necrosis. It is a practical and potentially-reproducible method of managing one of the most common complications of implant-based breast reconstruction.
-
Review Article12-01-2016
Multidisciplinary Approach to Neoadjuvant Endocrine Therapy in Breast Cancer: A Comprehensive Review
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(12):615-622
Abstract
Review ArticleMultidisciplinary Approach to Neoadjuvant Endocrine Therapy in Breast Cancer: A Comprehensive Review
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(12):615-622
Views109See moreABSTRACT
Breast cancer is the most common type of cancer and the leading cause of cancer-related death among women worldwide. Hormone receptor-positive (HRþ) tumors represent the most common form of this disease, with more than 70% of breast cancers expressing these receptors. Response and benefit to neoadjuvant chemo-therapy (NCT) varies according to HR expression, with lower responses in luminal tumors as compared with hormone receptor-negative (HR-) and human epidermal growth factor receptor 2-positive (HER2þ) tumors. Neoadjuvant endocrine therapy (NET) is an option for selected patients with HRþ locally advanced breast cancer. Neoadjuvant endocrine therapy has a favorable toxicity profile, and is associated with benefits such as having low cost and being more easily available even for cancer care professionals outside major urban areas or tertiary centers. These factors are particularly relevant, as 70% of breast cancer deaths occur in women from low-income and middle-income countries. Additionally, NET is being increasingly explored, not simply to allow for less extensive surgery, but also as a scientific tool, with the use of biomarkers to predict outcomes in adjuvant trials and for the individual patient. This review details the current and most relevant evidence about NET for breast cancer as well as the future directions of this field.
-
Original Article07-27-2011
Diagnostic accuracy of the fine needle aspiration cytologyand core needle biopsy as a diagnostic method for breast lesions
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(3):139-143
Abstract
Original ArticleDiagnostic accuracy of the fine needle aspiration cytologyand core needle biopsy as a diagnostic method for breast lesions
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(3):139-143
DOI 10.1590/S0100-72032011000300007
Views71See morePURPOSE: to determine the accuracy of fine-needle aspiration biopsy (FNAB) and of core-needle biopsy (CNB) in diagnosing breast lumps and breast cancer. METHODS: this was a cross-sectional, retrospective and descriptive study based on the review of medical records. FNAB and CNB were carried out sequentially according to the routine of the Mastology Service. Both percutaneous procedures were applied to 233 patients during the period from March 2005 to February 2007. Women aged 18 years or more with changes in the clinical and/or image examination of the breast or a family history of breast and/or ovarian cancer were included. FNAB and CNB were carried out according to the technical recommendations of the National Institute of Cancer. The percentage of agreement, Cohen's Kappa coefficient, sensitivity, specificity, positive and negative predictive values and the accuracy of FNAB and CNB were calculated, considering the surgical biopsy as the gold standard. RESULTS: the average age of the patients was 49.0 years (±12.7) and the tumors measured 26.9 mm on average (±23.1), being larger than 20 mm in 47.2% of cases. Sensitivity, specificity, positive and negative predictive values and accuracy were higher for CNB than for FNAB, regardless of the size of the breast lesion. The diagnostic accuracy was 97.5% for CNB and 77.5% for FNAB. CONCLUSION: although the CNB showed higher rates of sensitivity, specificity, positive predictive value, negative predictive value and accuracy than FNAB for palpable and non-palpable breast lumps, the method remains useful for the minimally invasive diagnosis of mammary lesions, especially when its results are analyzed together with the clinical and imaging examination.
-
Original Article04-04-2007
Evaluation of response to primary chemotherapy in Brazilian patients with locally advanced breast cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(1):18-26
Abstract
Original ArticleEvaluation of response to primary chemotherapy in Brazilian patients with locally advanced breast cancer
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(1):18-26
DOI 10.1590/S0100-72032007000100004
Views73See morePURPOSE: to evaluate the loco-regional response to primary chemotherapy in patients with breast cancer at stages II and III. METHODS: a retrospective and analytical clinical study carried out in 97 patients with an average age of 52.2 years old, with breast cancer at stages II and III, attended from January 1993 to December 2004, and submitted to 3 to 4 cycles of primary chemotherapy with 5-fluorouracil - 500 mg/m2, epirubicin - 50 mg/m2 and cyclophosphamide - 500 mg/m2 or doxorubicin - 50 mg/m2 e cyclophosphamide - 500 mg/m2, and then to loco-regional surgical conservative or radical surgical treatment. Chi-square and Fisher’s exact tests were used to study the association among the variables (age, menopausal state, pre-chemotherapy tumoral volume, axillary condition, stage, therapeutic scheme and number of cycles), while Pearson’s correlation coefficient was used for the quantitative variables (tumoral volume according to the anatomo-pathological study and the post-chemotherapy clinical tumoral volume. The significance level was 5%. RESULTS: there were 56.8% of cases at stage II and 43.2% at stage III. Approximately 50% of the patients received FEC50 and 50% AC. Objective clinical response with primary chemotherapy was obtained in 64.9% of the cases. Full clinical response occurred in 12.3% of patients, while full pathological response occurred in 10.3% of the cases. CONCLUSIONS: there was a statistically significant correlation between the number of cycles and the response to primary chemotherapy. Patients who received 4 cycles had better response than those who received 3 cycles. There was also a statistically significant concordance between the evaluation through clinical examination of the response to primary chemotherapy and the pathological findings. No statistically significant correlation was observed concerning age, menopausal status, tumoral volume, and pretreatment of axillary damage.
-
Original Article03-20-1999
Core Biopsy for the Diagnosis of Subclinical Breast Lesions
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(2):69-76
Abstract
Original ArticleCore Biopsy for the Diagnosis of Subclinical Breast Lesions
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(2):69-76
DOI 10.1590/S0100-72031999000200003
Views73See morePurpose: to evaluate core biopsy (CB) for the diagnosis of subclinical breast lesions, comparing with surgical biopsy previously identified by stereotaxic mammography. Methods: this is a cross-sectional study of 41 subclinical lesion cases over 35 years of age, between January 1995 and February 1997 at the Instituto de Ginecologia da Universidade Federal do Rio de Janeiro. The cases were classified mammographically as benign, probably benign, suspicious and malignant. Benign and probably benign lesions were studied together for statistical purposes. The histopathologic diagnosis of CB was classified as inadequate for diagnosis, absence of malignancy, suspicious and malignant. The histopathologic diagnosis of the surgical biopsy was classified as absence of malignancy, pre-malignant and malignant. The sensitivity, especificity and predictive values of CB were evaluated. Mammography likelihood ratio and core biopsy likelihood ratio were evaluated to predict breast cancer. Results: CB coincided with surgical biopsy in 86.2% of the 29 cases of absence of malignancy. All cases suspected by CB were malignant by surgical biopsy. All cases malignant by CB were also malignant by surgical biopsy. CB sensitivity and specificity were 36.4% and 100%, respectively. Positive predictive value was 100% and negative predictive value was 78.1%. In the group classified mammographically as malignant the likelihood ratio was 9.7; for suspicious lesions it was 1.3 and for probably benign lesions it was 0.1. Core biopsy likelihood ratio was infinite (¥) for suspicious and malignant lesions, 0.4 for cases classified as absence of malignancy and 1.4 for inadequate for diagnosis cases. Conclusions: after analysis of the results, with the use of the likelihood ratio, we conclude that CB report of absence of malignancy did not allow to rule out the diagnosis of malignancy. In these cases, we should correlate the result with mammography. If CB shows absence of malignancy and there is no correlation with mammography, the research must be continued. When the report of CB was suspicious, the probability of a breast carcinoma was very high. In these cases, we should perform a surgical biopsy to establish a definitive diagnosis, because an infiltrating carcinoma needs a different therapy when compared with carcinoma in situ and atypical hyperplasia. In the cases of histopathologic report of malignancy, the probability of breast cancer was high, since we did not observe any false positive CB. In these cases, CB allowed a quick diagnosis without the need of surgical biopsy.


