Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(4):221-224
DOI 10.1590/S0100-72031998000400008
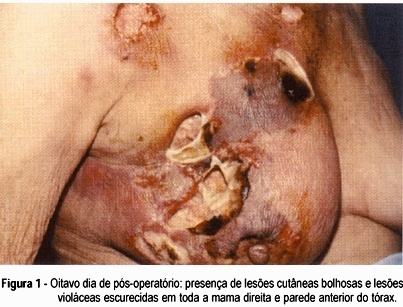
A case of postsurgical necrotizing fasciitis is presented. A 68-year-old female patient was submitted to a lumpectomy for a big breast lipoma. After surgen there was an aggressive local infection, with extensive necrosis of the breast tissue, including the superficial and deep fasciae and also the skin over the breast. The gravity of the disease and the difficulties in its diagnosis due to the late skin necrosis are emphasized. Under such circunstances an early and aggressive approach is necessary.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(4):209-213
DOI 10.1590/S0100-72031998000400006
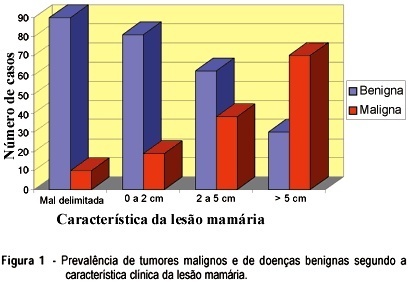
Fine-needle aspiration cytology (FNAC) is a simple method and free from complications, among great value in mastology. Its accuracy can suffer the influence of several factors, among which we can highlight the experience of the physician who performs it. With the objective of verifying the effectiveness of FNAC performed by general gynecologists, 341 patients were studied concerning the relationship between the results of FNAC and the histology of the breast lesion. We obtained sensitivity of 70.87%, specificity of 70.58%, predictive positive value of 92.40%, predictive negative value of 89.36% and accuracy of 70.67%. We concluded that FNAC is of great value in handling breast lesions and can be appropriately performed by general gynecologists. The method, however, may lead to errors of diagnosis. We do not recommend, therefore, the use of the result of FNAC as a definitive diagnosis; instead this result must be interpreted in the context of the clinical diagnosis and mammography.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(6):303-308
DOI 10.1590/S0100-72031998000600002
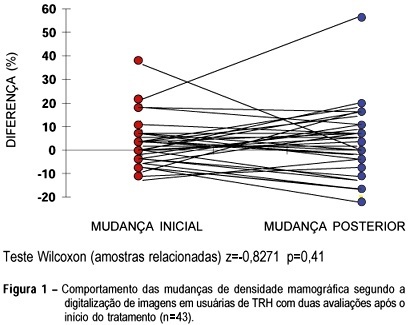
Objective: to compare mammographic density changes, case by case, according to image digitization in three consecutive evaluations of users or nonusers of hormonal replacement therapy (HRT). Methods: 59 postmenopausal women were evaluated, 43 being users of cyclic or continuous estro-progestin hormonal replacement therapy, and 16 nonusers. The criteria of inclusion were: amenorrhea for at least 12 months, a normal mammographic examination at the beginning of the HRT (users) or the clinical follow-up without HRT (nonusers), at two incidences (mediolateral and craniocaudal). The following variables were used for the evaluation of mammary density: initial change - the difference between the first mammography after HRT performed in 12 ± 3 months and the mammography performed before HRT-and final change - the difference between the second mammography after HRT performed in 24 ± 3 months and the mammography performed before HRT. Wilcoxon and c² tests were used in order to evaluate the differences in mammographic density changes. Results: more than half (56.3%) of the women, HRT users with initial increase in mammographic density remained with the increase after the final evaluation. This finding was not significant (p=0.617). In the same group, the initial nonincrease was significantly associated with the final nonincrease (p=0.017). Among the nonusers, all breasts that were not totally fat at the initial evaluation presented a mammographic density decrease at the final evaluation. Conclusions: the majority of HRT users presenting mammographic density increase at the first evaluation, after approximately one year of use, remained with the increase at a second evaluation. After some time, the nonusers tended to present a significant mammographic density decrease (p=0.003).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(11):658-663
DOI 10.1590/S0100-72032006001100005
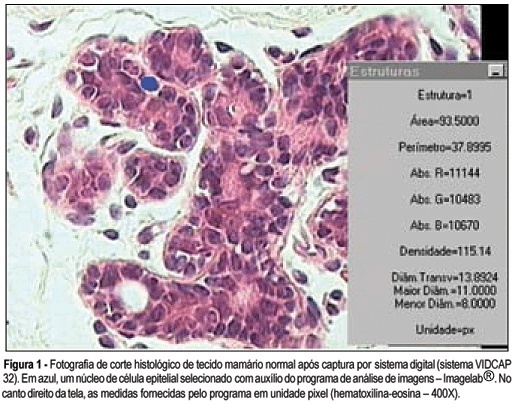
PURPOSE: to analyze breast tissue of postmenopausal women before and after six months of continuous combined estrogen-progestin replacement therapy (0.625 mg conjugated equine estrogens associated with 2.5 mg medroxyprogesterone acetate). METHODS: all patients were evaluated before treatment and considered eligible to receive the drug. The material was obtained from the upper outer left quadrant, through a percutaneous large-core breast biopsy. Epithelial density and nuclear volume on hematoxylin-eosin-stained plates were evaluated for the morphological study. Morphometry was graphically analyzed by optical microscopy (400X) after acquisition of image by a digital image-capturing system (Vidcap 32) and image analysis system (Imagelab 2000 Software®). RESULTS: after six months of estrogen-progestin replacement therapy, there was a significant increase in nuclear volume in late postmenopausal women (103.6 to 138.1 µm³). There was no difference in epithelial density with the treatment (before 0.08 and later 0.10). CONCLUSIONS: estrogen-progestin combined replacement therapy for six months induced an enhacement in nuclear volume of breast epithelial cells, suggesting an increase in their metabolic activity. However, it is important to emphasize that this finding was observed only in late postmenopausal women. The increased nuclear volume could precede other events that confirm the stimulation of cellular proliferation by these hormones.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(5):298-303
DOI 10.1590/S0100-72032006000500006
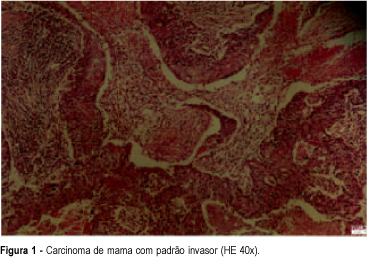
PURPOSE: to assess p53 protein expression in infiltrating ductal breast carcinoma and to analyze its association with histological and nuclear grade. METHODS: sixty-five consecutive females who were diagnosed with primary infiltrating ductal breast tumor from July 1999 to July 2001 were included in the present study. Mean patient age at diagnosis was 69.2 years (range 41 - 90). All patients were first treated with surgical therapy, conservative surgery or mastectomy. None of the patients received any preoperative adjuvant therapy. Resected breast tumor specimens were fixed in 10% formalin, paraffin embedded, and conserved for immunohistochemical analysis. p53 protein expression was evaluated. Primary monoclonal anti-human p53 antibody DO-7 (DAKO) was used. Frequency distributions were tested by the chi2 test. A level of p<0,05 was considered significant. RESULTS: p53 expression was detected in 24 (36,9%) of 65 carcinomas. Of the cases with protein expression, 13 (54,2%) were high or histological grade III, 8 (33,3%), were grade II, 3 (12,5%) were grade I. On nuclear grade analysis, of the cases with protein expression, 13 (4,2%) were nuclear grade III, 9 (37,5%) were grade II and 2 (8,3%) were grade I. p53 expression was frequent in carcinomas with high histological and nuclear grades. CONCLUSIONS: p53 expression was significantly associated with the histological grade. On the other hand, nuclear grade was not significantly related to p53 expression.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(7):419-421
DOI 10.1590/S0100-72031999000700009
Squamous cell carcinoma of the mammary tissue is a very rare neoplasm, representing less than 1% of all breast carcinomas. The present study reports a case of squamous cell carcinoma of the breast, treated at the Hospital Araújo Jorge/ACCG. The tumor diagnosis, treatment and prognosis are also discussed.