-
Original Article07-10-2023
The Relationship between Bone Mineral Densitometry and Visceral Adiposity Index in Postmenopausal Women
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):082-088
Abstract
Original ArticleThe Relationship between Bone Mineral Densitometry and Visceral Adiposity Index in Postmenopausal Women
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):082-088
Views216Abstract
Objective
It was aimed to compare visceral adiposity index (VAI) levels in patients with normal bone mineral density (BMD), osteopenia, and osteoporosis.
Methods
One hundred twenty postmenopausal women (40 with normal BMD, 40 with osteopenia, and 40 with osteoporosis) between the ages of 50 to 70 years were included in the study. For females, the VAI was calculated using the formula (waist circumference [WC]/[36.58 + (1.89 x body mass index (BMI))]) x (1.52/High-density lipoprotein [HDL]-cholesterol [mmol/L]) x (triglyceride [TG]/0.81 [mmol/L]).
Results
The time of menopause from the beginning was similar in all groups. Waist circumference was found to be higher in those with normal BMD than in the osteopenic and osteoporotic groups (p = 0.018 and p < 0.001, respectively), and it was also higher in the osteopenic group than in the osteoporotic group (p = 0.003). Height and body weight, BMI, blood pressure, insulin, glucose, HDL-cholesterol, and homeostasis model assessment-insulin resistance (HOMA-IR) levels were similar in all groups. Triglyceride levels were found to be higher in the normal BMD group, compared with the osteoporotic group (p = 0.005). The level of VAI was detected as higher in those with normal BMD, compared with the women with osteoporosis (p = 0.002). Additionally, the correlation analysis showed a positive correlation between dual-energy X-ray absorptiometry (DXA) spine T-scores, WC, VAI, and a negative correlation between DXA spine T-scores and age.
Conclusion
In our study, we found higher VAI levels in those with normal BMD, compared with women with osteoporosis. We consider that further studies with a larger sample size will be beneficial in elucidating the entity.
Key-words Bone mineral densitydual-energy X-ray absorptiometryObesitypostmenopausal osteoporosisvisceral adiposity indexSee more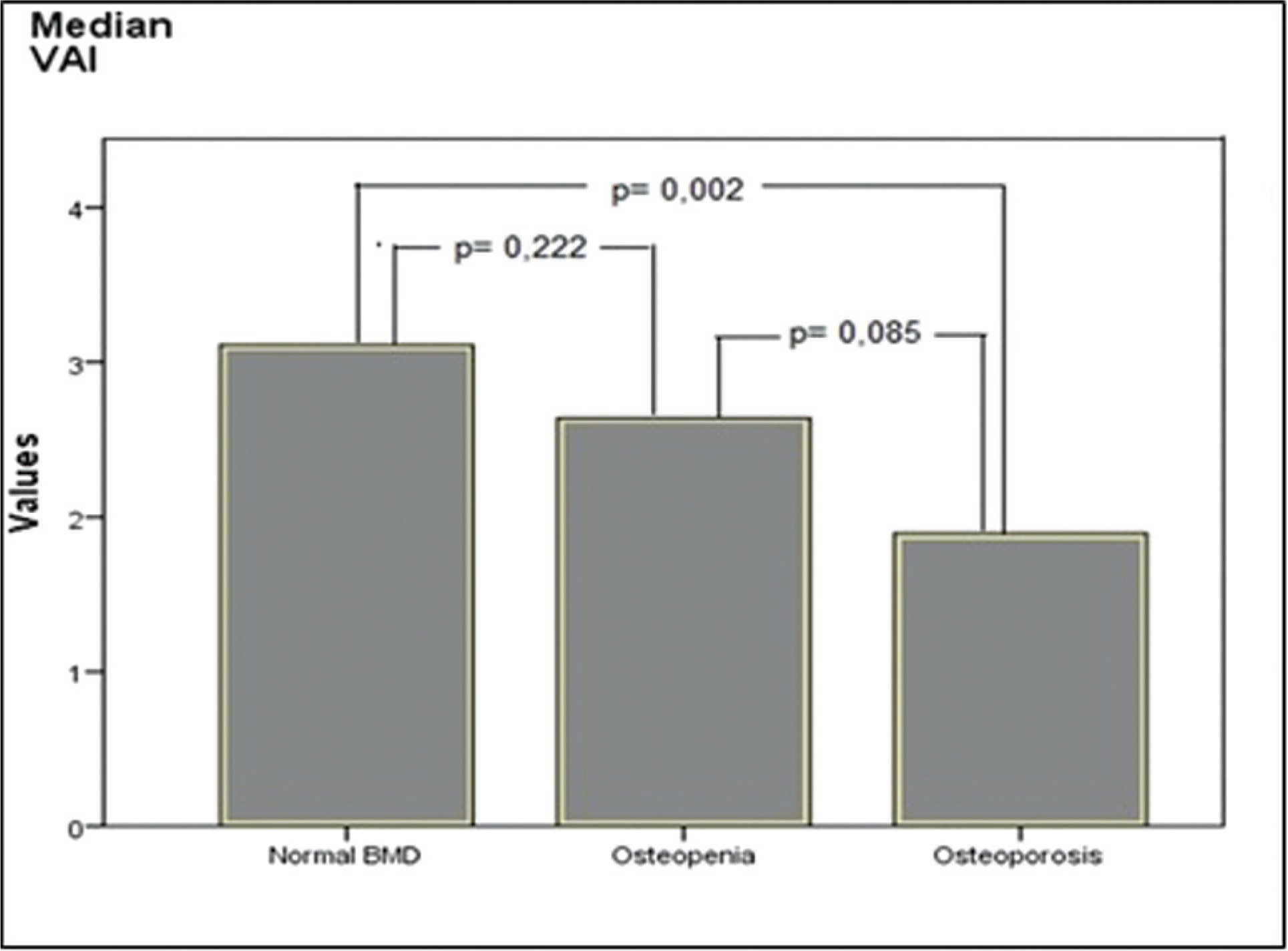
-
Original Article09-02-2004
Serum leptin levels and bone mineral density in postmenopausal women
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(6):429-433
Abstract
Original ArticleSerum leptin levels and bone mineral density in postmenopausal women
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(6):429-433
DOI 10.1590/S0100-72032004000600002
Views139See moreOBJECTIVE: to correlate serum leptin concentration with bone mineral density (BMD) in postmenopausal women. METHODS: twenty-two healthy postmenopausal women were included in the present study. BMD was measured by dual energy X-ray absorptiometry at the lumbar spine and femoral neck. Serum leptin concentrations were determined using an immunoradiometric assay. Statistical analysis was performed by ANOVA and Dunn and Pearson's correlation tests. RESULTS: mean BMD values were 0.898 ± 0.140 g/cm² at the lumbar spine and 0.760 ± 0.152 g/cm² at the femoral neck. Mean serum leptin concentration was 17.2 ± 9.4 ng/ml and no significant differences were observed among women with normal BMD, osteopenia and osteoporosis (18.6 ± 7.8, 18.9 ± 9.9 and 15.6 ± 10.6, respectively; p > 0.05). No significant correlations were observed between serum leptin levels and BMD measurements at the lumbar spine and femoral neck, when the whole sample was considered and when patients were divided into groups with osteoporosis and/or osteopenia and a control group. We observed a positive significant correlation between serum leptin levels and body mass index (BMI) (r = 0.66; p = 0.0044). CONCLUSIONS: there was no direct correlation between leptin and BMD in postmenopausal women, although we observed positive significant correlation between leptin and BMI. This fact indicates a possible indirect effect of leptin on bone metabolism.
-
Original Article11-04-2003
Prevalence of osteoporosis in postmenopausal women and association with clinical and reproductive factors
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):507-512
Abstract
Original ArticlePrevalence of osteoporosis in postmenopausal women and association with clinical and reproductive factors
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(7):507-512
DOI 10.1590/S0100-72032003000700007
Views124See morePURPOSE: to evaluate the prevalence of osteoporosis in climacteric women and analyze the influence of general and reproductive risk factors on bone mineral density. METHODS: a cross-sectional study with the evaluation of the 473 hospital records of climacteric women followed up at the Menopause Outpatient Facility of CAISM/Unicamp, between 03/28/2000 and 04/17/2001. These women were at least 12 months in amenorrhea and presented the results of a bone densitometry study performed at the Nuclear Medicine Department of HC/Unicamp. The following variables were evaluated: age, color, body mass index, level of education, smoking, use of medication, age at menopause, parity, use and length of hormone replacement therapy and its effect on bone mineral density. Statistical analyses were performed using logistic regression ajusted by age and hormone replacement therapy use. RESULTS: the mean age of the studied women was 53.9 years (± 7.1 SD) with mean age at menopause being 45.9 years (± 6.9 SD). Osteoporosis occurred in 14.7% and osteopenia in 38% of the cases in the lumbar vertebrae (L2-L4 interspace) and in 3.8 and 32.7% in the femur, respectively. Logistic regression adjusted to age and hormone therapy showed an association between the following variables: level of education, age at menopause and body mass index. CONCLUSION: there was a high prevalence of osteoporosis and osteopenia in the studied population. Advanced age, lower level of education, late menarche, early menopause and lower body mass index were identified as risk factors for developing decreased bone mass in the studied population.


