Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):878-882
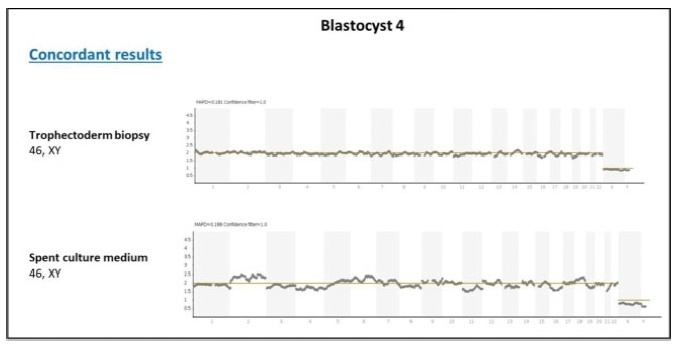
Non-invasive preimplantation genetic testing for aneuploidies (niPGT-A) aiming to assess cell-free embryonic DNA in spent culturemedia is promising, especially because it might overcome the diminished rates of implantation caused by the inadequate performance of trophectoderm (TE) biopsy. Our center is part of the largest study to date assessing the concordance between conventional PGT-A and niPGT-A, and we report here the delivery of the first baby born in Brazil using niPGT-A. The parents of the baby were admitted to our center in 2018. They did not present history of infertility, and they were interested in using in vitro fertilization (IVF) and PGT-A in order to avoid congenital anomalies in the offspring. A total of 11 (3 day-5 and 8 day-6) expanded blastocysts were biopsied, and the spent culture media (culture from day-4 to day-6) from 8 day-6 blastocysts were collected for niPGT-A. Overall, 7 embryos yielded informative results for trophectoderm (TE) and media samples. Among the embryos with informative results, 5 presented concordant diagnosis between conventional PGTA and niPGT-A, and 2 presented discordant diagnosis (1 false-positive and one falsenegative). The Blastocyst 4, diagnosed as 46, XY by both niPGT-A and conventional PGTA, was warmed up and transferred, resulting in the birth of a healthy 3.8 kg boy in February 2020. Based on our results and the recent literature, we believe that the safest current application of niPGT-A would be as a method of embryo selection for patients without an indication for conventional PGT-A. The approximate 80% of reliability of niPGT-A in the diagnosis of ploidy is superior to predictions provided by other noninvasive approaches like morphology and morphokinetics selection.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):608-615
To establish a relationship between serum progesterone values on the day of frozen blastocyst transfer in hormone-replaced cycles with the probability of pregnancy, miscarriage or delivery.
This was an ambispective observational study including all frozen-thawed embryo transfer cycles performed at our department following in vitro fecundation from May 2018 to June 2019. The outcomes evaluated were β human chorionic gonadotropin (β-hCG)-positive pregnancy and delivery. Groups were compared according to the level of serum progesterone on the day of embryo transfer: the 1st quartile of progesterone was compared against the other quartiles and then the 2nd and 3rd quartiles against the 4th quartile.
A total of 140 transfers were included in the analysis: 87 with β-HCG>10 IU/L (62%), of which 50 (36%) delivered and 37 had a miscarriage (42%).Women with lower progesterone levels (< 10.7ng/mL) had a trend toward higher β-HCG-positive (72 versus 59%; p>0.05), lower delivery (26 versus 39%; p>0.05) and higher miscarriage rates (64 versus 33%; p<0.01). Comparing the middle quartiles (P25-50) with those above percentiles 75, the rate of pregnancy was similar (60 versus 57%; p>0.05), although there was a trend toward a higher number of deliveries (43 versus 31%; p>0.05) and a lower number of miscarriages (28 versus 45%; p>0.05). These differences were not statistically significant.
There were no differences in pregnancy and delivery rates related with the progesterone level when measured in the transfer day. The miscarriage rate was higher in the 1st quartile group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(7):335-340
DOI 10.1590/S0100-72032008000700003
PURPOSE: to evaluate the effect of exposure of female rats to therapeutic ultrasound in the pre-implantation phase. METHODS: pregnant Wistar female rats have been exposed to 3 MHz, 0.6 W/cm² ultrasound, pulsatile ultrasound (PUS) or continuous ultrasound (CUS), and controls, unplugged ultrasound (UUS), for five minutes. The rats were sacrificed at the 20th day post-insemination. Biochemical and hematological analyses have been done. Animals have been submitted to necropsy in order to identify lesions of internal organs, and to remove and weight the liver, kidneys and ovaries. Alive, malformed, dead and reabsorbed fetuses have been counted. RESULTS: the rats have not presented changes in their body and organs weight, and neither in their reproductive capacity, but there has been an increase in triglycerides in the PUS and CUS groups, when compared to the UUS group. The fetuses' relative weights of the heart (0.7 ± 0.9), liver (9.8 ± 0.8), kidneys (6.2 ± 0.8) and lungs (3.8 ± 0.4) increased in the CUS, when compared to the heart (0.7 ± 0.9), liver (9.8 ± 0.8), kidneys (6.2 ± 0.8) e lungs (3.8 ± 0.4) of the UUS. CONCLUSIONS: in the experimental model, the therapeutic ultrasound used has not caused meaningful maternal toxicity. Pulsatile waves have not changed fetal morphology, but continuous waves have caused increase in the relative weight of the fetuses' heart, liver, lungs and kidneys.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(5):219-223
DOI 10.1590/S0100-72032008000500003
PURPOSE: to evaluate the toxicity of tacrolimus on embryonic development in rats treated during the tubal transit period. METHODS: sixty Wistar rats were distributed into four groups (15 animals each), which received different doses of tacrolimus through intragastric administration: (T1) 1.0 mg/kg/day, (T2) 2.0 mg/kg/day and (T3) 4.0 mg/kg/day. The control group (C) received distilled water. The rats were observed daily to detect clinical signs of toxicity. The treatments were performed from the first to the fifth day of pregnancy. The following maternal variables were analyzed: body, ovary, liver, and kidney weights, food intake, number of corpora lutea, implants, alive and dead fetuses, and implantation rates. The fetuses and placentae were weighed and the former were observed in order to detect external malformation. Statistical analysis was performed by one way: analysis of variance (ANOVA), folowed by the Dunnet test (alpha=0.05). RESULTS: there were no signs of maternal toxicity, such as body weight loss, decrease in food intake or in organ weights (p>0.05). There was also no significant difference among weights of fetuses (C: 1.8±0.6; T1: 2.2±0.5; T2: 1.9±0.5 and T3: 2.0±0.5 g) and placentae (C: 1,6±0.4; T1: 1.5±0.4; T2: 1.8±0.4 e T3: 1.6±0.4 g), with p>0.05; no external malformation was detected in the fetuses. CONCLUSIONS: the administration of tacrolimus to pregnant rats during the tubal transit period does not seem to generate any toxic effect to mother or embryo.