Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(9):534-540
DOI 10.1590/S0100-72032005000900006
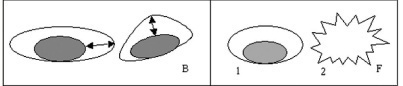
PURPOSE: to evaluate the role of morphological (12) and Doppler velocimetry (17) ultrasonographic features, in the detection of lymph node metastases in breast cancer patients. METHODS: 179 women (181 axillary cavities) were included in the study from January to December 2004. The ultrasonographic examinations were performed with a real-time linear probe (Toshiba-Power Vision-6000 (model SSA-370A)). The morphological parameters were studied with a frequency of 7.5-12 MHz. A frequency of 5 MHz was used for the Doppler velocimetry parameters. Subsequently, the women were submitted to level I, II and III axillary dissection (158), or to the sentinel lymph node technique (23). Sensitivity, specificity, and positive and negative predictive values were calculated for each parameter. The decision tree test was used for parameter association. The cutoff points were established by the ROC curve. RESULTS: at least one lymph node was detected in 173 (96%) of the women by the ultrasonographic examinations. Histological examination detected lymph node metastases in 87 women (48%). The best sensitivity among the morphological paramenters was found with the volume (62%), the antero-posterior diameter (62%) and the fatty hilum placement (56%). Though the specificity of the extracapsular invasion (100%), border regularity (92%) and cortex echogenicity (99%) were high, the sensitivity of these features was too low. None of the Doppler velocimetry parameters reached 50% sensitivity. The decision tree test selected the ultrasonographic parametners: fatty hilum placement, border regularity and cortex echogenicity, as the best parameter association. CONCLUSION: the detection of axillary cavity lymph node stage by a noninvasive method still remains an unfulfilled goal in the treatment of patients with breast cancer.