Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(3):142-148
07-10-2023
To understand the impact of the coronavirus disease 2019 pandemic on in vitro fertilization (IVF) clinical pregnancy rates and analyze factors that may have influenced their outcome.
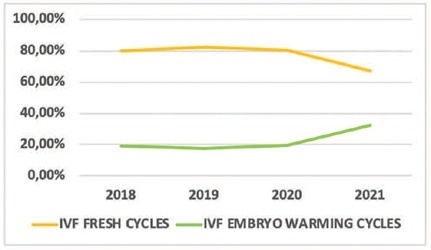
This was a retrospective observational study conducted at a tertiary-care Brazilian fertility center. All fresh IVF and embryo warming cycles performed from March 11 to December 31, 2018–2021 were analyzed, and their data were used to calculate fertilization, embryo cleavage, cycle cancellation, embryo transfer (ET), and clinical pregnancy rates. Statistical tests were used to evaluate the alterations found. Logistic regression models were used to explore the association of the categorical variables with the observed clinical pregnancy rates. Data from 2018 and 2019 (prepandemic) and 2020 and 2021 (pandemic) were grouped.
A total of 756 cycles were analyzed (n = 360 prepandemic and n = 396 pandemic). The age group of the patients, fertilization rates, and cleavage rates did not have significant differences (p > 0.05). There was a reduction in the percentage of fresh IVF and an increase in embryo warming cycles (p = 0.005) during the pandemic. There was also an increase in fresh cycle cancellations (p < 0.001) and a reduction in ET rates (p < 0.001). The pandemic had a negative impact on clinical pregnancy rates (p < 0.001) especially due to the increase in fresh cycle cancellations (p < 0.001).
Embryo warming cycles with subsequent frozen-thawed ET were presented as a viable alternative to continue assisted reproductive treatments against pandemic restrictions on fresh cycles, ensuring clinical pregnancy, albeit at a lower rate than that of the prepandemic period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):834-839
01-12-2021
It has been suggested that excess body weight could represent a risk factor for infertility outcomes. The present study aimed to evaluate the association of overweight and anovulation among infertile women with regular menstrual cycles.
We conducted a retrospective case-control study with consistently anovulatory patients undergoing assisted reproduction treatment. The patients were stratified into normal weight (body mass index [BMI]: 18.5-24.9kg/m2) and overweight (BMI: 25.0- 29.9kg/m2).Those with polycystic ovary syndrome or obesity were excluded. The groups were matched for age, duration of infertility, prolactin, follicle stimulating hormone (FSH), thydroid stimulating hormone (TSH), luteinizing hormone (LH), and estradiol levels.
Overweight was significantly associated with anovulation, when using the World Health Organization (WHO) criteria for anovulation: progesterone levels>5.65 ng/ml and ultrasonography evidence of follicle collapse (odds ratio [OR]: 2.69; 95% confidence interval [CI95%]: 1.04-6.98).
Body mass index above the normal range jeopardizes ovulation among non-obese infertile women with regular menstrual cycles.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(1):32-37
06-19-2006
DOI 10.1590/S0100-72032006000100006
PURPOSE: to evaluate the rate of chemically diagnosed pregnancy (serum beta-HCG>25 mIU/mL levels obtained fourteen days after the embryonic transfer) clinically diagnosed pregnancy (gestational sac visualized by ultrasound four to six weeks after the embryonic transfer) and miscarriage rates in women submitted in vitro fertilization to (IVF) and intracytoplasmic sperm injection (ICSI) in a tertiary center of assisted reproduction and to correlate these rates with age. METHODS: retrospective transverse study with analysis of 1016 cycles of controlled ovarian hyperstimulation of 932 infertile women with indication of IVF (370 cycles) or ICSI (646 cycles). The patients' age ranged from 22 to 46 years. All women with age over 35 years included in the study had FSH<15 IU/L. The studied cycles were divided into two groups: the first including the cycles referring to women of 22 to 30 years and the second group, to those of 31 to 46 years. The studied variables were: pregnancy (chemical or clinical) and miscarriage rates. The chi2 test was used to compare these rates between the groups. RESULTS: the total pregnancy rate was 36.42%, with a significant reduction starting at 30 years (p=0.0001). From 22 to 30 years (303 cycles) the pregnancy rate was 45.4%, while in the range from 31 to 46 years (713 cycles), it was 25.1%. The miscarriage rates were, 10.2 11,6%, respectively (p=0.6854). CONCLUSION: although the miscarriage rates did not differ between the groups, a decrease in the pregnancy rate of infertile women submitted to IVF or ICSI was observed after the age of 30 years. Thus, we recommend the gynecologists not to postpone the investigation and the referral for treatment of infertility.