-
Original Article
Association of Overweight and Consistent Anovulation among Infertile Women with Regular Menstrual Cycle: A Case-control Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):834-839
01-12-2021
Summary
Original ArticleAssociation of Overweight and Consistent Anovulation among Infertile Women with Regular Menstrual Cycle: A Case-control Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(11):834-839
01-12-2021Views162See moreAbstract
Objective
It has been suggested that excess body weight could represent a risk factor for infertility outcomes. The present study aimed to evaluate the association of overweight and anovulation among infertile women with regular menstrual cycles.
Methods
We conducted a retrospective case-control study with consistently anovulatory patients undergoing assisted reproduction treatment. The patients were stratified into normal weight (body mass index [BMI]: 18.5-24.9kg/m2) and overweight (BMI: 25.0- 29.9kg/m2).Those with polycystic ovary syndrome or obesity were excluded. The groups were matched for age, duration of infertility, prolactin, follicle stimulating hormone (FSH), thydroid stimulating hormone (TSH), luteinizing hormone (LH), and estradiol levels.
Results
Overweight was significantly associated with anovulation, when using the World Health Organization (WHO) criteria for anovulation: progesterone levels>5.65 ng/ml and ultrasonography evidence of follicle collapse (odds ratio [OR]: 2.69; 95% confidence interval [CI95%]: 1.04-6.98).
Conclusion
Body mass index above the normal range jeopardizes ovulation among non-obese infertile women with regular menstrual cycles.
-
Original Article
Antral Follicles Count and Anti-Müllerian Hormone Levels after Gonadotoxic Chemotherapy in Patients with Breast Cancer: Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):162-168
04-01-2017
Summary
Original ArticleAntral Follicles Count and Anti-Müllerian Hormone Levels after Gonadotoxic Chemotherapy in Patients with Breast Cancer: Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):162-168
04-01-2017Views112Abstract
Aim
To assess ovarian reserve (OVR) by means of follicle-stimulating hormone (FSH), anti-Müllerian hormone (AMH), and antral follicle count (AFC) measurement in eumenorrheic women with breast cancer, exposed to gonadotoxic chemotherapy.
Method
Fifty-two women (35.3 ± 3.8 years old) with breast cancer and undergoing cyclophosphamide-containing chemotherapy were enrolled. The assessment was performed before chemotherapy (T1) and after 2 (T2) and 6 months (T3).
Results
Six months after chemotherapy, the prevalence of regular cycles was 60%. Anti-Müllerian hormone decreased down to undetectable levels at T2 and T3 (T1: 2.53 [1.00–5.31]; T2 < 0.08; T3: < 0.08 [< 0.08–1.07] ng/mL), (p< 0.0001). Antral follicle count was 11 [8.0–13.5] follicles at T1 and lower at T2 (5.50 [3.75–8.0] and T3 (5.0 [2.5–7.0]) (p< 0.0001). In patients who remained with regular cycles during chemotherapy or resumed normal menses, FSH and estradiol levels remained unchanged.
Conclusion
Anti-Müllerian hormone and AFC are useful as markers of OVR decline in women exposed to chemotherapy. Follicle-stimulating hormone is only adequate in women who become amenorrheic.
Key-words AnovulationAnti-müllerian hormoneantral follicle countchemotherapy-induced amenorrheaOvarian reserveSee more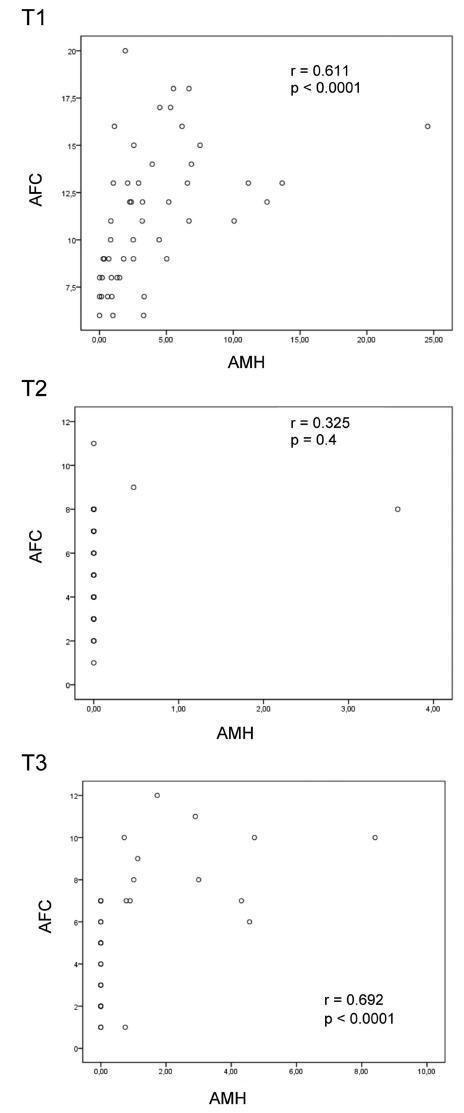
-
Artigos Originais
Spontaneous pregnancies after ovarian puncture for in vitro maturation in women with the polycystic ovary syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(3):138-141
06-09-2009
Summary
Artigos OriginaisSpontaneous pregnancies after ovarian puncture for in vitro maturation in women with the polycystic ovary syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(3):138-141
06-09-2009DOI 10.1590/S0100-72032009000300006
Views109See morePURPOSE: to report three cases of spontaneous gestation in women with polycystic ovarian syndrome (PCOS), that occurred in the months subsequent to transvaginal oocyte retrieval for in vitro maturation (IVM). METHODS: three infertile patients with PCOS, submitted to oocytes' IVM without previous ovarian stimulation, were included in the study. During the procedure of oocytes' collection, each ovary was drilled from four to eight times. RESULTS: none of the patients got pregnant with the IVM technique. Evaluating the cases' follow-up, in seven months after the procedure, the three patients got pregnant without the help of techniques of assisted reproduction, which resulted in three births. CONCLUSIONS: the multiple drillings in the ovary of these patients with PCOS, during the process to collect oocytes, may have contributed to their pregnancy in the months following the procedure.


